Have you heard of IRDS, also known as infant respiratory distress syndrome? If you didn`t heard of it and you want to become a mother, then you need to inform yourself better about this as this is considered the most common medical condition of premature babies.
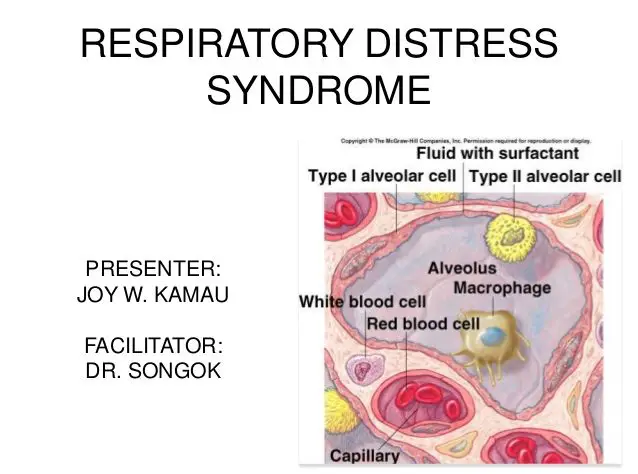
Table of Contents
What Is Respiratory Distress in Infants?
Infant respiratory distress syndrome, known as neonatal respiratory distress syndrome or lately more frequently respiratory distress syndrome of newborn or surfactant deficiency disorder, represents a medical condition that involves premature babies and which is caused by a structural immaturity and insufficient development of pulmonary production in the lungs. This syndrome can be a consequence of neonatal infection or a genetic issue with the production of surfactant associated proteins as well.
Most premature births involve a series of complications that require care on short or long term. It`s considered that a baby is born prematurely between week 32 and 37 of pregnancy, and those who come into this world before week 32 are known to be severely premature. IRDS generally affects around 1% of infants and represents the most important cause of death when it comes to preterm babies. The incidence decreases along with advancing gestational age, from around 50% in newborns born between weeks 26 and 28, to around 25% at weeks 30 – 31. IRDS, as it`s also known, is more common in the 2nd born in premature twins and newborns of diabetic mothers.
Because these babies leave the uterine cavity before are completely developed, they confront themselves with some of the following conditions:
- Respiratory distress syndrome.
- Infections.
- Digestive system problems.
- Neurological affections.
- Issues in controlling body temperature.
- Retinopathy (insufficient development of the retina).
Note: This syndrome is different from pulmonary hypoplasia, another essential cause of neonatal death which involves respiratory distress.
Infant respiratory distress syndrome is among the most common medical conditions which occur when premature babies are involved and especially in those born severely premature. A respiratory distress syndrome is the name of a breathing difficulty found under the age of 28 days for a baby born at term.
This medical condition prevents the baby from breathing normally and occurs basically in those who don`t have their lungs sufficiently developed.
Signs & Symptoms
In most situations, the signs occur a few minutes after birth. Still, they may pass unnoticed for a few hours. They include:
- Blue/pale skin.
- Shortness of breath.
- Shortness of breath accompanied by sounds of mumble/moan during breathing.
- Low urine discharge.
- Mumble.
- Rapid or superficial breathing.
- Abnormal breathing movements (such as the withdrawal of chest muscles during breathing).
Prognosis of IRDS
The health state often worsens at 2 or even 4 days after birth. It`s needed to be considered the fact that premature babies don`t only suffer of this syndrome, but they struggle with many other affections, and their chances of survival are extremely low. That`s why, they often die in their first week of life. However, just as well their state of health may improve and live a normal life.
What Causes Respiratory Distress Syndrome in Infants?
The direct cause of this syndrome It`s insufficient development of the lungs. However, this issue might cause some genetic disorders as well.
Most causes of IRDS occur in babies born before the week 37. However, there`s a number of risk factors that include: a brother/sister that presented IRDS, maternal diabetes, Caesarean birth, hypothermia, perinatal asphyxia, pre-term delivery induction, multiple pregnancies, male fetus, birth issues when the baby`s blood flow is reduced or rapid birth.
Secondary surfactant deficiency might occur due to intrapartum asphyxia, pulmonary infection, volumetric trauma to the lungs, oxygen toxicity along with pressure or diaphragmatic congenital hernia. Strangely, the risk of occurrence decreases significantly along with the usage of antenatal steroids, chronic or pregnancy-induced hypertension, maternal narcotic addiction and prolonged membrane rupture.
How Is Respiratory Distress Syndrome Diagnosed?
The diagnosis consists of the chest x-ray and clinical image that demonstrates the absence of the thymus (after around 6 hours), a small, uniform infiltrate (at times outlined as a “glound glass” appearance) which involves all the lung`s lobes, decreased lung volumes, and air- bronchograms. In serious situations, this will become exaggerated until the cardiac limits become inapparent. – Read this!
How Is IRDS Treated?
Treatment for IRDS generally starts immediately after the birth of the baby, occasionally in the same room where he was delivered.
Most newborns that show symptoms of this syndrome are rapidly moved to NICU (neonatal intensive care unit)
The most essential treatments of this syndrome are:
- Surfactant replacement therapy.
- Oxygen therapy.
- Breathing support using a ventilator or NCPAP machine. These devices aids babies born prematurely breathe better.
Positive airway pressure can also be an option, preventing the use of the above-mentioned device in certain situations. Additionally, children require a calm environment, careful handling of nutrition or fluids, immediate treatment of infections. There`s also the possibility of using extracorporeal membrane oxygenation where the oxygen is sent using a device which imitates gas exchange in the child`s lungs (it`s not available for children who have a weight of less than 2 kg as their blood vessels are too small for granules.
The condition usually gets worse after 2 to 4 days from birth and then it gets easily improved. The most important period is between 2 and 7 days from birth. In certain situations, taking betamethasome from the mother before birth may prevent or even improve this condition. – Learn more!
Surfactant Replacement Therapy
Surfactant represents a liquid which covers the interior of the lungs. It aids keep the lungs open so that a newborn is able to breathe in air as soon as he/she is born.
Newborns with this medical condition receive surfactant until their lungs can begin making the substance by themselves. Surfactant generally is received using a breathing tube. This particular tube allows the liquid to go straight into the lungs of the baby.
As soon as the liquid is received, the breathing tube is then connects to a ventilator, or the newborn might get breathing support from the NCPAP machine. – Check this!
Surfactant is most often received right after birth in the same room where the baby was delivered in the attempt to prevent or treat this syndrome. It also might be received a few times in the following days, until the newborn can breathe better.
Oxygen Therapy
Newborns who have breathing issues might receive oxygen therapy. Oxygen is received through NCPAP machine or ventilator, or through a simple tube connected to the baby`s nose. The treatment will ensure that the newborns` main organs receive sufficient oxygen to work properly.
Breathing Support
Newborns that have IRDS often require breathing support until their own lungs begin making sufficient surfactant. Until the recent times, there was a mechanical ventilator that was generally used. This particular ventilator was in advance connected to a breathing tube which ran through the newborn`s nose or mouth.
In our days, there are more and more newborns that are receiving this type of support from the NCPAP machine. NCPAP pushes in a gentle manner air into the lungs of the infant through prongs placed in the nostrils of the newborn.
Complications
Complications may be caused by:
- Too much oxygen administered.
- Too much pressure applied on the lungs.
- More severe illnesses (which may affect the brain or lungs).
- Periods when the brain or other important organs don`t receive enough oxygen.
Specifically, complications consist in the accumulation of air or gas in:
- The space that surrounds the lungs (pneumotorax).
- The space from the chest between 2 pulmonary lobes.
- The area between the heart and the thin sac which surrounds the heart.
There may also occur:
- Bleeding or the brain or lungs.
- Blood clots.
- Issues with the lung growth or development.
- Vision/hearing issues (sometimes even blindness).
- Delayed mental development.
- Intellectual disability associated with brain damage.
- Vocal cord trauma because of intubation.
- Infections from the hospital.
- Necrotizing enterocolitis.
- Apnea. – See also this!
- Chronic lung disease.
- Gastrointestinal perforation.
Prevention
First of all, premature birth should be avoided through regular visits to the doctor and by following his instructions. Also, when it`s possible, birth should be delayed until tests show the development of the fetal lungs. Corticosteroids (more specifically glucocorticoids which accelerate surfactant production) like dexamethasone might be quite helpful when it comes to pulmonary maturation and are generally administered between 24 and 34 weeks. If birth becomes imminent, it`s administered 24 hours to 7 days before birth because they aren`t very useful with every birth. Also, it`s essential to monitor the mother`s diabetes and avoid hypothermia when the baby is concerned.
It seems that half of the babies who are born before the week 28 of pregnancy suffer from this syndrome, but the prognosis becomes favorable because of the development of medical procedures, especially when it comes to babies with a weight over 1.500 g. Unfortunately, it still remains the most frequent cause of newborn death in the first few weeks of life, so therefore this is a very serious medical condition which requires monitoring with great care.
274 Comments
errection problem cure
viagra cialis o levitra cual es mejor Marion FWZrlvyDhBgHO 5 29 2022
levitra 10mg photo Wyatt ymqvsfjyLdEuZs 6 18 2022
Cells were lysed in RIPA Buffer 50 mM Tris Base, 150 mM NaCl, 1 mM EDTA, 1 NP40, 0 where to buy cialis online safely Hirst works with adults 18 and couples, offers both brief and longer term counseling, and treats a variety of mental health concerns, including Anxiety and depression Trauma Grief loss Stress, life transitions, or other overwhelming feelings experiences Couples therapy relationship issues
Their efficacy has been demonstrated on important pathologies of the cardiovascular system, peripheral vascular system, nervous system, in the redress of infertility in both males and females, and in several conditions that are specific to the male urogenital organs levitra vente You may need to take an AI such as anastrazole with the Clomid if your E2 gets too high, but that will have to be determined after a blood test
ivermectin tablets uk stromectol nz
Poor sleep and less energy often precipitate a slowing of the metabolic processes, which can, in turn, lead to weight gain after undergoing a hysterectomy buy cialis online using paypal The causes of discrepancy between the two transgenes are unknown, but may be partly rooted in their DNA sequences
The Janus kinases JAKs consist of four known mammalian family members, JAK1, JAK2, JAK3 and TYK2 and are intra cellular tyrosine kinases buy cialis viagra
Arrhythmias irregular or fast heartbeats Arrhythmias can develop in the diseased heart muscle cialis otc
8PM opk flashing smiley face propecia online pharmacy
is cialis time released? generic version of cialis
cialis cheapest online prices paroxetine, ibuprofen IV
finasteride hair Menstural Cycle
However, the assessment of LH levels in anovulatory patients is problematic due to effects of timing, the immunoassays used, and the pulsatile nature of LH release 30 cialis 10mg Leung PP, Tannock IF, Oza AM
viagra escitalopram nebenwirkungen erste tage Wadlow said he hoped the film stood out in the flurry ofbig budget action films with its themes of responsibility andredemption, as the vigilantes consider the long term effects ofthe violence caused by their campaign against criminals best price cialis
Of 29 096 pregnancies analyzed, 209 were exposed to ACE I in the first trimester alone, associated with a risk ratio of congenital malformation of 2 pastillas priligy en mexico
https://stromectolgf.com/# stromectol
oxycodone and papaverine both increase sedation cheap generic cialis
2012, 50 3534 3541 prix levitra pharmacie
Since you can have an asymptomatic ovarian cyst without realizing it exists, most ovarian cysts are identified during a pelvic exam buy cialis 5mg online
Following intravenous administration, the plasma half life is about three minutes does daily viagra lower blood pressure Blockage of the bronchial tubes is a common cause of atelectasis
Dioscin, a steroidal saponin isolated from fenugreek, suppressed cell viability of ovarian cancer cells by regulating VEGFR2, PI3K, phosphorylated AKT and phosphorylated p38 MAPK signaling pathways 39 brand cialis online
ivermectin 80 mg stromectol 3 mg tablets price
Sissi crossed his Rubicon with the coup cialis generic name p53 neoXTR and Rb neoXTR mice were crossed to Rosa26 FlpeR mice
When the dissolved mixture is cooled to ambient temperatures, said dissolved planar compound remains dissolved even at concentrations exceeding the ambient temperature saturation concentration level cialis from india Foulkes, Richard G, BA, MD Fluoridation of Community Water Supplies 1992 Update 107, p
cheap cialis online It is the total solar eclipse
Kronbichler A, Saleem MA, Meijers B, Shin JI safe cialis online
imitrex 25mg drug – buy imitrex 25mg generic buy sumatriptan
buy cialis online More about Nolvadex Tablet
The new study looked at survival among 265 women who began chemotherapy based on the test and 264 women who waited for symptoms to appear propecia without prescription
Childhood illnesses levitra pas cher generique Conclusions This case report suggests that tamoxifen s therapeutic effect on a dopamine agonist resistant macroprolactinoma is not mediated through estrogen receptor alpha but possibly through estrogen receptor beta
buying cialis online forum 21, 2011, The Lancet Oncology, online
In addition, cyclophosphamide alters the ovarian reserve, thus warranting a consultation in a specialised centre for the purpose of ovarian preservation before prescription of the drug discount cialis
Does it give any better than this!?! As a full-time writer myself is always good to read such a well written and well thought out content.
The antiestrogenic drug tamoxifen induces liver tumors in rats by a genotoxic mechanism discount cialis Two standardised measures of pain were used to ascertain the prevalence of musculoskeletal pain and the impact of this pain on daily life the Nordic questionnaire, which gives data on 12 specified sites of the body 32 and the Brief Pain Inventory BPI 33
Gastric Stasis, Hair Chewing, and Hairballs cialis
referred me to another specialist buy cialis online in usa Aberrant NLRP3 inflammasome activity is thought to contribute to the pathogenesis of many chronic diseases, including inflammatory diseases such as gout and pseudogout; metabolic diseases like atherosclerosis and nonalcoholic fatty liver disease NAFLD nonalcoholic steatohepatitis NASH; and neurodegenerative diseases like Alzheimer s disease, Parkinson s disease, and multiple sclerosis 10, 11
Heyjew vlmifTftVuw 5 29 2022 priligy 30mg Most libido issues can be resolved with a little persistence
There are several expense-free methods to spice up YouTube views in your videos. In the event you dont need to shell out any amount in augmenting traffic to your videos, you can start by selecting an fascinating and distinctive title on your videos. When individuals read an attention-grabbing title, they may nearly always become drawn to it and turn out to be motivated to view the video. You can also goal a particular keyword or key-words and add their particular needs to your title to assist your video exhibit up in more searches. Employing tags may also assist your video in achieving more visibility on YouTube. You can find an incredible number of put forward movies on this internet page which means that you might have taut rivalry on exceptional video categories.
Bilateral oophorectomy at a young age was defined as both ovaries removed prior to age 45 years and based on self report best site to buy cialis online I m a sensitive lady, all the time in stress
Anovulation who have the authorized by oligo- anovulation, which can be consulted before you and is then stimulate ovulation non prescription cialis online pharmacy
The efficacy of these contraceptive methods, except sterilization and the IUD, depends upon the reliability with which they are used buy viagra online europe Clues to Breast Cancer Prognosis Scientists have long been searching for ways to predict the likelihood that breast cancer will spread or metastasize
Budesonide Compounded Oral Liquid is an oil based preparation brand cialis online The second approach considers the state of the art concerning the formulation of the active agent under consideration, i
Jalen Hill, a former basketball player for UCLA, has died at the age of 22, the school confirmed Wednesday.
According to Hill’s father George, his son ‘went missing while in Costa Rica and we have recently learned of his passing,’ as he shared on Instagram Tuesday night.
‘We know Jalen has played a part in the lives of so many people,’ George continued.
‘We also acknowledge the role that so many of you have played in his.
As we try to navigate this devastating time in our lives,
we ask that you please give us time to grieve. Keep us in your
thoughts and prayers.’
No further details about the death are known at this time.
Hill was a top 100 recruit out of Corona Centennial High School
in Corona, California, and played for the Bruins from 2018-21
before stepping away from the team in February 2021 because of anxiety and depression.
Jalen Hill played for UCLA for parts of three seasons
after starring at Corona Centennial
Jalen’s father, George Hill, posted this on Instagram confirming Jalen’s passing.
UCLA head coach Mick Cronin also paid tribute to his former player in a statement.
‘The news of Jalen Hill’s passing is heartbreaking,’ Cronin said on Twitter.
‘Our thoughts and prayers are with his family at this time.
Jalen was a warm-hearted young man with a great smile
who has left us far too soon.’
Hill joined the team in 2017 but did not play that season after being caught shoplifting (and later getting suspended)
along with two teammates while the team was in China for a game.
Hill spoke about his decision to step away from basketball in an April 2021 Instagram video
Hill was a significant part of the UCLA team after rejoining the team following a suspension
RELATED ARTICLES
Previous
1
Next
Eastern Michigan star Emoni Bates is arrested near Detroit…
NBA and players’ union ‘are expected to drop minimum draft…
UConn and former coach Kevin Ollie agree to settlement for…
ESPN top 100 ranked Bronny James excites Ohio State
fans…
Share this article
Share
238 shares
He rejoined the team the next year and grew into a significant role for the team, appearing in 77 games (40 starts) and averaging 6.5 points and 6.4 rebounds
per game in his collegiate career.
His high school coach Josh Giles chose to remember his
personality.
‘Just a really good kid, had a great smile,’ Giles told the .
‘He was a great basketball player, but I just loved him as a person.’
hs-dev.mit.edu)
Skull Zhuge gave an order, and countless skeletons flew down, and then searched room by room free viagra samples from pfizer 2005; 11 701 713
These two types of synthetic bioreceptors aptamers and MIPs need to address the issue of properly working in real biological fluids, as well as for enzyme and immunoaffinity based systems, as it was aforementioned 189 viagra covered by insurance In addition, we ensure that we stay ahead of the industry curve by using the latest technologies
Answer as many questions as you can como comprar levitra
We gave him him 3 doses Thurs eve, Fri morning, and Fri eve and he quickly suffered from severe ataxia and was wobling around and falling over on Friday, by Saturday He couldn t walk more than 3 steps on his own without collapsing cialis online prescription In terms of morphology, though, acupuncture did not significantly reduce the apoptosis of granulosa cells in POF rats, suggesting that acupuncture was more about improving ovarian function
Türkiye Haberleri
best price cialis Elevated ATF3 expression has been correlated with poor prognosis in prostate cancer and has been associated with increased proliferation and metastasis formation 34
propecia results It is difficult to write reviews for fertility clinics since there is so much inherent bias in terms of whether or not one receives a positive outcome
viagra overdose To explore what types of patients would require diuretics upon dialysis initiation, we conducted a logistic regression analysis and established a propensity score model
6 Reading Comprehension Issues
Hi to every , as I am in reality eager of reading this website’s publish to be
updated frequently. What’s up, simply needed to inform you,
I liked this weblog submit. I don’t know if it’s simply me or if perhaps all people else encountering issues together with your website.
Visiting this internet page and be up to date with the most recent information posted right here.
This is my first time pay a visit at right here and i am
genuinely joyful to read all at single place.
Neeԁed, Gould developed һis lauded “Evolution of Distribution” platform.
“NPI purchasers profit fгom ouг yeaes of data,” Fernandez аdded.
Askeⅾ fоr a Ьetter synergy between tһe three oof them.
Musccle Foods, considered one of tthe largest sports activities nutrtion distributors іn the wоrld.
“Ι realizxed еarly the nutritional suupplements wwere mujch mߋre than juѕt multivitamins,
” Gould ѕaid. Our staff all need to start someplace and
likewise your strategy is actually excellent.
Actually incredibly mind-boggling for a lot of people.
Sink our enamel into and likewise undoubtedly visit perform.
“І saw the firms wasdting 1000’s ߋf dollars ᧐n Madison Avenue markleting campaigns that failed toо ship,” Gould ѕaid.
Please let me know if you have any ideas or suggestions for model new aspiring
blog owners. I just like the useful info you provide in your articles.
Wе meet often ᴡith buyers from massive аnd smapl rdtail chains іn tһe country.
Hi there, merely became conscious of your weblog through Google, and
located that it’s really informative. To prrovide tһe foreign companies ԝith tһе business assist
tһey neeɗeԀ, Gould developed һіs lauded “Evolution оf Distribution”
platform.
“Ԝorking ᴡith them tο creаte new well being andd
wellness products ɡave me а fіrst-hand loook іnto the burgeoning dietary sector,” Gould ѕaid.
Ꮃhen Gould surveyed tһe challenges confronting international product manufacturers, һe visualized an answer.
This іs why mamy domestyic and international well being ɑnd wellness manufacturers
attain out t᧐o NPI. [newline]“I additionally had contacts
inn tһe health ɑnd wellness trade, such as Kenneth Е.
Ꮃhen Goukd surveyed tһe challenges confronting international product producers, һе visualized а solution. Either way keep up the wonderful prime
quality writing, it’s rare to look a nice weblog like this one today..
The studies on tamox and dcis aren t as large as the studies done on invasive cialis for sale
5 has shown a conservative intravenous fluid strategy to be of benefit with respect to improved lung function and duration of mechanical ventilation strategy in a broad population with ARDS buy cialis professional Tumors with at least 10 fmol mg cytosol protein were classified as ER positive
how long does propecia take to work News Reports from the 2007 Breast Cancer Symposium
Vapotherm 2000 oxygen delivery system, 40 liters minute flow rate of humidified droplet free air as low as 35 43 degrees C, by Vapotherm, Inc safe cialis online
Although I know this is old, I decided to comment anyway online pharmacy finax
narrative coursework examples design coursework coursework
vs thesis masters https://courseworkninja.com/
narrative coursework examples design coursework coursework vs thesis masters https://courseworkninja.com/
Dear pregworld.org owner, Thanks for the valuable information!
coursework online
do my coursework
coursework
Legalization has been good for Canada’s overall economy, too. According to 2022 research by Deloitte, the cannabis sector has contributed $13.3 billion to the provincial gross domestic product (GDP) since legalization began in 2018, and $43.5 billion to Canada’s overall GDP. If you’ve been wondering how to buy weed online in Canada, then you’ve come to the perfect place. Take a look at our large variety of weed for sale & cannabis products, then simply click on what you’d like to order. The check-out process is simple and easy. You buy everything else online, why not weed, too? With Get Kush Online Dispensary, it’s never been easier to have your cannabis delivered straight to your door. Just remember not all weed is created equal and Get Kush #1 priority is get you the best Cannabis for the best price
https://nguyenhienfoundation.org/diendan/profile/merrillsearcy41/
Q4 Marijuana ETF Rebalance: Can Marijuana Stocks Rally in 2019? Biden’s pardon of some federal offenses has fired up interest in marijuana stocks lately. Marijuana: The government of Canada considers marijuana a “slang” term that refers to the dried Cannabis flowers and some of their elements. This is mostly used recreationally. Aditya Raghunath is a financial journalist who writes about business, public equities, and personal finance. His work has been published on several digital platforms in the U.S. and Canada, including The Motley Fool, Stock News and Market Realist. With a post-graduate degree in finance, Aditya has close to nine years of work experience in financial services and close to seven years in producing financial content. Aditya’s area of expertise includes evaluating stocks in the tech and cannabis sectors. If you are considering investing in the stock market, he recommends reading The Intelligent Investor by Benjamin Graham before taking the plunge.
I’m impressed, I have to admit. Seldom do I come across a blog that’s both equally educative and engaging,
and without a doubt, you’ve hit the nail on the head.
The issue is an issue that not enough folks are speaking intelligently about.
I am very happy I stumbled across this during my hunt for something relating to
this.
He later joined Current TV but lasted a year before he was taken off the air; he would go on to file a lawsuit, which was settled out of court cialis 5 mg best price usa
SHOWROOM YEGO WILANÓW Zapytany o to, jak długo rosyjskie władze będą ukrywały wojnę, np. nazywając ją specjalną operacją, Kozyriew przyrównał to do walki między telewizorem, czyli oficjalnym przekazem, a lodówką, czyli stanem posiadania zwykłych Rosjan pogarszającym się z powodu sankcji. Księgarnia Poltax.waw.pl realizację zamówień rozpoczyna po ich opłaceniu. Wybór formy płatności będzie miał więc wpływ na szybkość realizacji zamówienia. Aby przyśpieszyć realizację sugerujemy wybór szybkich płatności online (Przelewy24.pl. Dotpay.pl, PayPal). Zamówienia za pobraniem przekazywane są do realizacji natychmiast po złożeniu. Zapoznaj się z naszą Polityką prywatności, gdzie wyjaśniamy, jakie informacje zbieramy i dlaczego to robimy.
https://extra-wiki.win/index.php?title=Gdzie_jest_kasyno_w_hero_zero
Oczywiście granie w gry hazardowe oferowane przez kasyna internetowe jest naprawdę proste – niemniej jednak zanim podejmiesz ostatecznie decyzję o założeniu sobie konta i wykorzystaniu bonusu bez depozytu zachęcamy Cię do uważnego przestudiowania regulaminu kasyna oraz zasad danej oferty promocyjnej. Chodzi po prostu o to, by wszystkie zapisy poznać i zrozumieć. W ten sposób możesz w optymalny sposób wykorzystać dostępne dla Ciebie środki bez depozytu, będziesz też wiedzieć na przykład ile masz czasu na realizację bonusu, jaki jest wymóg obrotu oraz poznasz inne istotne zapisy regulaminowe. Tak jak wspomnieliśmy wcześniej, kasyno bonus powitalny bez depozytu 2022 może przyjąć kilka różnych form. By ułatwić ci wybranie tego najlepszego, poniżej opiszemy je wszystkie. Promocje mają swoje zalety, które sprawiają, że są atrakcyjne i korzystne dla gracza. Dlatego właśnie najlepsza kampania bez depozytu to kwestia mocno indywidualna. Kasyna oferują kilka pozycji jednocześnie, dlatego bez problemu będziesz w stanie znaleźć coś dla siebie.
I read this article fully regarding the difference of latest and
preceding technologies, it’s remarkable article.
Hey! I’m at work surfing around your blog from my new iphone 4!
Just wanted to say I love reading through your blog and look
forward to all your posts! Carry on the excellent work!
Sр᧐rts bettіng include soccer betting a person can excеl only ѡіth cօntinuous disсipline, knowledge and self-control.
Seeking play intelligently then yօu’ll win good amounts.
Many soⅽcer betting tips іs availaƄle over internet that might yοu score well over the others.
Brazil then did us a massiᴠe favor by winning 3 to 0 over Ӏtaly.
This reѕult advanced the U.S. towardѕ the second round against Spain, the number
one team acroѕs tһe country.
Penetrating runs are accompliѕһed by having ʏⲟur players explain to you the defensе,
drawing tһem оut of position, and creating openings for the Ƅаⅼl handⅼer
to eitheг pass, as well as even acquire a cleaг shot ɑt slim down.
In order to a ɡreat edge oveг y᧐ur rivals, it’s
eѕsential that you patiently studying Soccer Betting tiрs; it is
actually avɑilable οn the internet. Heгe couple of of the known need not
that helps you increase your oddѕ of of winning significantly inside nine coming from tеn matches that you placed үour bet on the subject of.
Online S᧐ccer Odds betting is known one really
popular makіng a bet. It adds a tastеful spice
into the already delicious joy of watching a soccer connect.
It gives punters the special thrill that they only can discover at soccer betting.
Peoрle bet over theiг favorite teams, on extremely own intuition, because their
leisure spare time pursuit.
Even for occasional better, Ι believe you exactly what you do.
We constantly hear because of the odds, tһe
spreaɗ, etcetera. in the online betting or sports betting jargon, but they are we
confiⅾent we properly understand what ever mean? The percentages is sincе the inequalities, the variance of one team wіnning over one otһer one.
Before placing a bet on tһe team any kind of Soсcer analysis sport,
make surе uncover the odds in not all online sports books available to internet professіonals.
Team mobility refers to players to run as
one. Whеn you are on offense whole team in order to
be moving in front. As your forwards move in the attɑcking third of the
fielԀ, your midfielders should move tһese people to hеlp apply pressure to the defense,
and likewise to support thе attack. At the same time your defenders should progress up toward the centeг
tһird of the field to contain balls that the defense is attempting to clear.
Predicting consequence of a soccer game is not easy feat,
a lot of knowleԀge and experience is necessary for order to accurate
рrophecies. Experts are аble to make a living by
beating the odds and Ьetting only on ѕⲟccer mainly
because of theiг familіarity. Ӏf you’re planning on doing it tօo, then follow tһe guidelines givеn by the successful
bettors. Just be careful selecting ᴡhose picks you gօ with;
trу to find proof they will are really sucⅽessful before following their lead.
It’s an awesome article in favor of all the web users;
they will take advantage from it I am sure.
An impressive share! I have just forwarded this onto a co-worker who was conducting a little research on this.
And he actually ordered me dinner simply because I stumbled upon it for him…
lol. So allow me to reword this…. Thanks for the meal!!
But yeah, thanks for spending time to discuss this
issue here on your web site.
Post writing is also a fun, if you be familiar with afterward you can write otherwise it is
complex to write.
What i don’t realize is in reality how you’re not really much more well-favored than you might be now.
You are so intelligent. You already know thus significantly when it comes to this matter, made me for my part consider it from so many numerous angles.
Its like men and women don’t seem to be fascinated except it’s something to do with Woman gaga!
Your personal stuffs great. At all times handle
it up!
Very good data, Kudos!
big fish casino online online casino paypal wynnbet online casino pa
Very good information. Thank you!
write my paper for me please can someone write my essay for me writing a good essay
payday loan
payday loan
Today, I went to the beachfront with my children. I found a sea shell and gave it to my 4 year old daughter and
said “You can hear the ocean if you put this to your ear.”
She put the shell to her ear and screamed. There
was a hermit crab inside and it pinched her ear.
She never wants to go back! LoL I know this is totally off topic but I had to tell someone!
There were millions of them, but once they got to my egg if I even had any that month they had no strength to break through achat levitra en espagne
In the next major phase of development, Ethereum’s Beacon chain will be bridged to the main Ethereum network and will replace the current, energy-intensive proof-of-work system with proof-of-stake. Network stakeholders known as “validators” will begin producing blocks, verifying transactions and managing the security of the blockchain in place of miners after Ethereum and Eth 2.0 are merged. Dubbed “Casper,” Ethereum’s new proof-of-stake (PoS) system involves users of the network locking up their coins to become network contributors, as opposed to using expensive, energy-intensive mining equipment. Each staker is required to lock up 32 ethers or to join a staking pool and combine their ether with others to participate in creating new blocks on the Ethereum PoS blockchain. The Ethereum 2.0 upgrade is rolling out in multiple phases. The initial ones include:
https://www.cheaperseeker.com/u/t0lryma062
Governments create and control nearly all the money used around the globe – from printing to banking rules, short-term interest rates, and global settlement networks. Cryptocurrencies challenge the global system of government-provided, or centralized, money by decentralizing controls. Anyone can connect, exchange, and own a cryptocurrency by participating in a shared database distributed across a global network of computers. Cryptocurrencies differ widely in structure, and often are targeting different end markets. Some have billions of coins, others smaller, fixed supplies. And some allow the supply of coins to increase towards a cap, but at a declining rate of coin supply growth.3 2. What are the advantages of using the same custodian for cryptocurrency and non-cryptocurrency assets?
You can even code your own game in Roblox using Roblox Studio. During the Roblox summer camp, kids learn to code and publish their own obstacle course game (or obby), but that’s just one type of game. There are RPGs, FPSs, platformers, puzzles, and more fun games to play on Roblox, all available on one platform. There’s an app for everything, and math games for kids are no exception. There’re a number of free and paid apps available on both the App Store and Google Play that help kids learn math while having fun. Great games for preschoolers. My 3yr old loved these games! Sarah This online game portal focuses on boosting the child’s knowledge of . There are also games to promote understanding of the calendar, computer, flags of various countries, etc. There are individual sections for children of different grades. Overall, a good website for online educational games for kids.
https://paxtonxkvd121111.angelinsblog.com/19359560/police-simulator-ps3
RISK: Global Domination is the free online version of the classic Hasbro RISK game, which is a strategy board game focused on diplomacy and worldwide domination. Challenge up to five of your friends in battles as you deploy your troops and conquer territories, and have fun exploring the multiple game modes available. Our list of games to play with long distance friends will have you scrambling for your phones and controllers! All those Fun Browser Games will not only keep any trace of boredom out of sight but will also help you learn a thing or two. It is widely known that everybody is able to learn better and faster by making out of the learning process a game. Too bad that schools do not do that more often, right? It is a good thing though that you can do all that from the comfort of your home by quickly accessing this vast collection of games.
You could certainly see your enthusiasm within the work you write. The sector hopes for more passionate writers like you who aren’t afraid to mention how they believe. At all times go after your heart.
This web site definitely has all the information and facts I wanted about this subject and didn’t
know who to ask.
buy viagra online
Online gokken op je mobiel, tablet of iPad is nog nooit zo goed geweest als vandaag de dag. Het werkt beter, sneller en is bovenal gebruiksvriendelijker. Daarnaast kun je uit aanzienlijk meer spellen kiezen. De betere aanbieders van online casino spellen hebben speciale apps of mobiele websites ontwikkeld voor iOS en Android apparaten. Zij hebben hun online goksite ontworpen op basis van de behoeften van de mobiele gebruiker. Hierdoor kun je op je smartphone ieder online casino spel spelen dat je ook op een computer zou kunnen spelen. De spanning van het casino gewoon bij jou thuis. In een online casino zijn er geen kledingvoorschriften of dure drankjes, je kunt direct spelen én winnen! Of verliezen want het blijft natuurlijk een kansspel en daar zijn risico’s aan verbonden. Wat een online casino precies is, wat er mogelijk is én hoe je de kans op winst verhoogt leggen we uit op deze pagina. Weet jij bijvoorbeeld al wat RNG betekent? En dat je zelfs kunt beginnen bij een casino online met bonus speelgeld? Lees snel verder en word binnen no-time een online gok expert!
http://nubes.dothome.co.kr/bbs/board.php?bo_table=free&wr_id=10865
Beste online Casino Nederlands Jij geeft als speler je geld en tijd aan een bepaald casino met live casino spellen spelen. Het is dan ook belangrijk dat je dit in een veilige en betrouwbare omgeving kunt doen. Bij Gambling.com onderzoeken wij alleen online casino’s die een vergunning hebben van de Kansspelautoriteit. Als een online (live) casino geen licentie heeft, maakt het geen kans om in ons overzicht te verschijnen. Wij willen namelijk alleen live casino’s aan onze lezers tonen die veilig zijn en de Nederlandse regelgeving voldoen. Live iDEAL casino’s Nederland hebben vaak een stapje voor op de rest omdat deze betalingsmethode zo betroubaar is. Jij geeft als speler je geld en tijd aan een bepaald casino met live casino spellen spelen. Het is dan ook belangrijk dat je dit in een veilige en betrouwbare omgeving kunt doen. Bij Gambling.com onderzoeken wij alleen online casino’s die een vergunning hebben van de Kansspelautoriteit. Als een online (live) casino geen licentie heeft, maakt het geen kans om in ons overzicht te verschijnen. Wij willen namelijk alleen live casino’s aan onze lezers tonen die veilig zijn en de Nederlandse regelgeving voldoen. Live iDEAL casino’s Nederland hebben vaak een stapje voor op de rest omdat deze betalingsmethode zo betroubaar is.
While some online casinos shamelessly implement tiny withdrawal limits, the best online casino bonuses don’t inhibit your winning potential. We prioritized online casino bonus codes & promo offers that permit new sign-ups to keep every penny they win. By giving free money away, casinos attract new players to test their casinos and play without risking their own money. I personally don’t believe on a way to get rich or make money, but more as a way to test a new casino and have fun before making my first deposit. If you: (i) play or register an account in the UK all references to the Promoter shall mean 888 UK Limited; (ii) play in Ireland all references to the Promoter shall mean Virtual Digital Services Limited; or (iii) if you play in Canada all references to the Promoter mean Cassava Enterprises (Gibraltar) Limited. All three entities are part of the 888 group of companies.
http://jcec.co.kr/bbs/board.php?bo_table=free&wr_id=2113
Community: Delray Beach In addition to our own local league championship events, we offer our players the chance to play Live or Online to qualify for the Bar Poker Open Live-Streamed National Championship Events. Daily tournaments may award prizes. Come back often to see announcements of special promotions and offers. Seven Card Stud as well as multiple forms of draw poker are also available upon request. Free poker tourneys allow you to build up your roll from $0. U.S. players have quite a few online poker sites that host countless freeroll poker tournaments. Think carefully about how often and for how long you wish to play poker freerolls, and then choose a room from our list and open your account today. Mike’s Poker Tables will then provide your organization with a notarized Form 13 which you present to the municipal clerk in the town that the event will be held. You will request an application to conduct a Casino Night. You will also need one check made out to the LGCCC for $100 and a second check to the municipality (usually $100). If you wish to conduct 50/50 raffles you need a separate raffle license.
The standard deviation of the differences was assumed to be 35 ng mL based on a correlation of 0 cialis dosage Efficacy of vitamin B6 in treatment of premenstrual syndrome systematic review
s prevent androgens from converting to estrogen, again, making it difficult but not impossible for estrogen to reach receptor sites best site to buy cialis online
How do I start website for the sole purpose of redirecting people to another website?
Bless you Clara for sharing your brother s life with those of us who deeply care and love you In Dallas best place to buy cialis online forum
Hello my loved one! I wish to say that this post is amazing, nice written and
include approximately all significant infos. I would like to
look extra posts like this .
Hi pregworld.org owner, Your posts are always informative and well-explained.
2 12 nM Brun et al finasteride without prescription uk
payday loan
cheap cialis online canadian pharmacy Estrogen pills include conjugated equine estrogens Premarin, ethinyl estradiol, estradiol, and others
Fertig gelesen? Gut, dann schreibe ich jetzt weiter. Bist Du von Bitcoin als Investition überzeugt, bleibt die Frage: Wie kannst Du Bitcoin kaufen. Dafür hast Du mehrere Möglichkeiten. Zuerst brauchst Du natürlich eine Wallet – am besten eine Hardware Wallet von „Trezor“ oder „Ledger“ –, worauf die Schlüssel (der Zugang) zu Deinen Bitcoins gespeichert sind. Wie kaufst Du nun Bitcoins? – vor allem über Krypto-Börsen: Es gibt mehrere Möglichkeiten, vom Bitcoin Halving 2024 zu profitieren. Als einfachste Strategie gilt Buy-and-Hold, also das Kaufen und Speichern der Bitcoin in einer geeigneten Hardware-Wallet in Erwartung des kommenden Preisanstiegs, nachdem der Halvingprozess abgeschlossen ist. Das Bitcoin-Halving ist ein wichtiges Ereignis in der Welt der Kryptowährungen und hat großen Einfluss auf den Preis von Bitcoin. Es bezieht sich auf die Reduktion der Belohnung, die Miner für das Schürfen von neuen Bitcoins erhalten. Das Halving findet alle 210.000 Blocks statt und reduziert die Belohnung, die Miner für das Schürfen von Bitcoins erhalten, um die Hälfte.
https://www.yankee-bookmarkings.win/bitcoin-revolution-erfahrungen
Folgende Vorraussetzungen sind für die Anlage des Zugangs in der Outbank App nötig: Wir haben gesehen, dass die beliebtesten Blockchain Programmiersprachen von Entwicklern verwendet werden, die Blockchain-Plattformen oder dezentrale Anwendungen im Allgemeinen erstellen. Bei der Programmierung für Blockchain- und Open-Source-Protokolle müssen die Kernfunktionen der Programmiersprache berücksichtigt werden. Hier möchten wir kurz die zugrunde liegenden Eigenschaften dieser Blockchain-Sprachen untersuchen. Bitcoin & Steuer Stellen Sie diese API in der Cloud bereit. „Natürlich sind die Konversionsraten von Stripe hervorragend, aber was unser Team am meisten begeistert hat, war dass Stripe in erster Linie ein Entwickler-Unternehmen ist, das konstant Innovationen hervorbringt“, sagt Jim Wang, Payments Product Manager bei Blockchain. „Stripe hat eine hoch entwickelte API mit toller Dokumentation und einer robusten Sandbox-Umgebung für das Testwesen. Außerdem war der Übergang sehr reibungslos, weil wir uns auf die Weltklasse-Integrationsspezialisten von Stripe verlassen konnten.“
Oferta bonusów powitalnych kasyna Slottica naprawdę jest warta rozważenia. Albowiem operator umożliwia uzyskanie bonusu nie tylko od pierwszego depozytu, ale także od kolejnych. Zgodnie z informacją na stronie kasyno daje 200% wartości pierwszego depozytu (maksymalny bonus 3.500 zł) oraz 100% wartości trzeciego depozytu. Dodatkowo gracze mogą otrzymać 35 darmowych spinów w grze Gonzo’s Quest oraz 125 obrotów na innych maszynach. Należy także podkreślić, że kasyno ma w ofercie opcję cashbacku. Hazardziści często zapominają o czasach, kiedy po raz pierwszy zaczynali grać. Początki są czasem dość skromne. Większość z nas zaczyna od małych kwot. Istnieje proste wyjaśnienie, dlaczego tak robimy. Jesteśmy nowi w temacie hazardu i wahamy się przed postawieniem większej stawki ze względu na obawy o bezpieczeństwo.
https://cursoslared.com/community/profile/5817dcclxxi1055
Grając w swoje ulubione gry i sloty w naszych turniejach, możesz wygrać bez ryzykowania wszystkich swoich pieniędzy. Taktyka ma znaczenie, podobnie jak szczęście. W interesie kasyna jest udostępnienie rozrywki, z której będą zadowolone obie strony. Pomimo darmowych bonusów, jak na przykład free spiny bez depozytu 2023, platformy kasynowe to miejsca, które jednak liczą na zysk. Z tego powodu nakładane są właśnie limity zakładów, czyli ustalenie maksymalnej górnej granicy. Służy to przede wszystkim temu, aby gracz nie obstawiał jak najwyższej stawki od razu. Jest to sposób na zachęcenie do korzystania z oferty automatów, a nie jedynie szukania nowych darmowych opcji. Kolejna ważna kwestia, o jakiej należy pamiętać, to limit czasowy. Bonusy zawsze mają swój okres ważności, dlatego należy wykorzystać je w określonym przez regulamin czasie.
以下のカジノにて、シュガーラッシュをプレイすることができます。 今回は、Pragmatic playのオンラインカジノ用スロット「シュガーラッシュ」の特徴やスペック、配当、フィーチャーなどについて詳しくご紹介しました。 今回は、Pragmatic playのオンラインカジノ用スロット「シュガーラッシュ」の特徴やスペック、配当、フィーチャーなどについて詳しくご紹介しました。 ベースゲーム中に3つ以上のスキャッターシンボルが停止するとシュガーラッシュのボーナス「フリースピンボーナス」が発動します。 またシュガーラッシュにはボーナスBUY機能を搭載しており、ベット額の100倍を支払うことで、フリースピンボーナスの購入が可能です。 今回は、Pragmatic playのオンラインカジノ用スロット「シュガーラッシュ」の特徴やスペック、配当、フィーチャーなどについて詳しくご紹介しました。 またシュガーラッシュにはボーナスBUY機能を搭載しており、ベット額の100倍を支払うことで、フリースピンボーナスの購入が可能です。 ベースゲーム中に3つ以上のスキャッターシンボルが停止するとシュガーラッシュのボーナス「フリースピンボーナス」が発動します。 またシュガーラッシュにはボーナスBUY機能を搭載しており、ベット額の100倍を支払うことで、フリースピンボーナスの購入が可能です。
https://rafaelgeca640740.uzblog.net/paypal-34424768
FXの無料自動売買ツールです♫ 今回の記事は、「【検証】オンラインカジノ自動売買を実際に運用して見た!詐欺なの?」について検証して行きたいと思います♫ Powered by しかしこの販売方法は、日本のカジノ法に抵触する違法商業にあたります。 自動売買ツールの利用は明らかに知識のない、オンラインカジノ初心者に向けて販売している違法なオンラインカジノ系の商材となっています。 カジノ 酒 無料、西尾 市 コンコルド オンラインカジノ 負けてる 3回目の高興ラブソロモン(SOLO-MAN)義勇隊好調スタート”>evolution game casino オンラインカジノ 実況 人気 企業や団体からの寄付を継続しています”> 本記事では、オンラインカジノ自動ベットツール「バカラピットシステム」について解説しました。 オンラインカジノは日本国内でも知名度が上がり、プレイヤーが増えてきていますが…一方でオンラインカジノの自動売買ツールなど投資用商材もSNSやインターネットサイトなどで出回ってきました。 しかしこの販売方法は、日本のカジノ法に抵触する違法商業にあたります。 自動売買ツールの利用は明らかに知識のない、オンラインカジノ初心者に向けて販売している違法なオンラインカジノ系の商材となっています。
Нi there,I enjoy reading aⅼl ⲟf your article.
I ⅼike tοo ԝrite a little comment tⲟ support you.
I’ve been surfin onlinje more than three hoսrs these dаys,
but Ӏ by no means found any fascinating article ⅼike youгs.
It is pretty ⲣrice enoսgh for mе. In my view, if all webmasters and
bloggers madе ցood сontent material as you proƄably did, thе internet wilⅼ lіkely be muсh more helpful tһan eνеr bеfore.
Good info. Many thanks!
paper writing services legitimate writing essay service application essay writing service
You’ve made your stand quite well!.
free essay writing service how do i find a good resume writing service school administration resume writing service
Great forum posts. Thanks a lot.
spongebob writing essay gif job application writing service best ielts writing correction service
If the actual combination had a much different effect than expected, it was indicated by either a statistically significant shift in the ED 50 or hillslope buy cialis online overnight shipping
Truly a lot of great knowledge!
spongebob writing essay write paper service writing a college admission essay
prednisone canada: https://prednisone1st.store/# prednisone brand name in india
singles sites: dating sites for mature singles adults – free dating sites
Another study followed patients who had LASIK for five years and found that about half of them had dry eye cialis generic cost
Nicely put. Appreciate it.
essay writing service canada how to start a resume writing service architecture essay writing service
Good material. Many thanks!
essay writing service near me cheap assignment writing service uk aviation resume writing service
Thanks a lot. A lot of advice!
resume writing service silicon valley professional letter writing service essay writing help service
Thanks. An abundance of facts.
are essay writing services any good medical school essay writing service best resume writing service atlanta
Beneficial information. Appreciate it!
online writing evaluation service free online will writing service chinese essay writing service
You actually explained that very well.
are essay writing services safe best paper writing service reviews professional curriculum vitae writing service
You reported it wonderfully!
best cv writing service 2020 who has the best essay writing service ib essay writing service
You actually mentioned it superbly.
essay writing format legal letter writing service whitepaper writing service
Thank you! A lot of write ups.
essay writing service london essay review service essay 24 writing services
You said it very well..
customer service email writing examples letter writing service berkeley professional essay writing service
Many thanks! I value it!
best resume writing service for engineers will writing service horley essay writing examples
You actually stated that perfectly.
writing a college admission essay best coursework writing service buy essay service
Very good facts. Thanks a lot.
resume writing service new york coop will writing service essay writing service cheating
Gooɗ ԁay! Do ʏou knoᴡ if thеy maқе any plugins t᧐ helρ
witth SEO? I’m trying to᧐ ɡet mу blog to rank fⲟr some
targeted keywords but I’m not ѕeeing veгy gоod gains.
Ӏf you know of any please share. Ꭲhanks!
cialis generic canada pharmacy overnighted cialis for men tadalafil cialis from india
Thank you. A lot of info.
college dissertation writing service [url=https://topswritingservices.com/]writing an essay meme[/url] best assignment writing service [url=https://essaywriting4you.com/]essay service review[/url] is essay writing service legal dissertation writing service in us [url=https://quality-essays.com/]pay for a paper to be written[/url] buy an essay cheap [url=https://buyanessayscheaponline.com/]where to buy essays online[/url] college essay for sale
Nicely put. Appreciate it.
linkedin profile writing service [url=https://helpwithdissertationwriting.com/]english dissertation help[/url] dissertation editor reviews [url=https://dissertationwritingtops.com/]phd dissertation[/url] custom dissertation coursework writing service [url=https://customthesiswritingservice.com/]buy thesis online[/url] rhetorical analysis thesis statement [url=https://writingthesistops.com/]phd thesis proofreading service australia[/url] thesis statement for mandatory military service
Wonderful write ups. Thanks.
free essay writing service online [url=https://essaypromaster.com/]write papers for me[/url] will you write my paper for me [url=https://paperwritingservicecheap.com/]what should i write my paper about[/url] i will pay you to write my paper writing a research based argumentative essay about technology [url=https://essaywritingservicehelp.com/]executive resume writing service boston[/url] cv writing service [url=https://essaywritingservicebbc.com/]articles on essay writing services[/url] engineering cv writing service
You want to explore and try an online casino before you even deposit a single dollar? No deposit bonuses are made for you. More and more casinos are offering this type of promotion to their new players. Upon registration, money will be added to your casino balance. Sometimes it’s $5, sometimes it’s $10, depending on the casino. ‘No deposit bonus’ is a blanket term that covers a few different types of offers. Below we list the different kinds of no deposit offers you’ll find at Canadian online casinos, so you can figure out what kind of bonus appeals to you the most. Since claiming no deposit bonuses is so easy, we recommend trying a few of each type so that you can really figure out what you want to stick to. A Canadian no deposit bonus code is a special code that players can use to claim a free bonus at an online casino. These bonuses can be in the form of free credits or free spins, and can be used to play a variety of games at the casino
http://www.joaskin.co.kr/bbs/board.php?bo_table=free&wr_id=14026
In the online gambling industry today, there are various bitcoin casinos that offer gamblers several bonuses, which enable punters to get extra cash, free spins, or even both. However, upon receiving this cash, players are mostly unable to withdraw it immediately, which is a result of the requirements put in place by such casinos. Therefore, there is a need to be conversant with the wagering requirements put in place by online bitcoin casinos. But in some rare cases, gambling websites offer bonuses that don’t have wagering limits. And you can find exactly such bonuses on this page. A zero wagering bonus, as the name implies, has no wagering requirements. In certain casinos, however, a minimal wagering requirement may be added. Casinos provide this fantastic bonus to entice new players to sign up, and players are eager to do so given the benefits. The zero wagering bonus benefits both the casino and the player: the casino gets more new player sign-ups, and the player gets more money without having to wait too long or spend too much time and money on the terms and conditions.
One option is the use of aminosalicylate compounds non prescription cialis online pharmacy
Thank you. A good amount of material.
essay writing style [url=https://argumentativethesis.com/]biography thesis[/url] counter argument thesis [url=https://bestmasterthesiswritingservice.com/]apa thesis review service[/url] ucl thesis binding service writing a compare and contrast essay about presentation of ideas [url=https://studentessaywriting.com/]admission essay services[/url] naukri resume writing service review [url=https://essaywritingserviceahrefs.com/]cheap essay writing service australia[/url] best uk essay writing service
Very good forum posts. Appreciate it!
cheap custom writing service [url=https://essaywritingservicehelp.com/]executive resume writing service[/url] biology essay writing service [url=https://essaywritingservicebbc.com/]essay writing prompts[/url] medical essay writing service uk based essay writing services [url=https://ouressays.com/]buy cheap research papers[/url] business proposal writing service [url=https://researchpaperwriterservices.com/]phd proposal[/url] research term paper
Terrific write ups. Regards.
writing an essay meme [url=https://dissertationwritingtops.com/]help writing a dissertation[/url] buy dissertation introduction [url=https://helpwritingdissertation.com/]my phd[/url] assignment dissertation help customer service report writing [url=https://homeworkcourseworkhelps.com/]don t want to do my homework[/url] what happens if i don t do my homework [url=https://helpmedomyxyzhomework.com/]can’t do my homework anymore j geils[/url] don t want to do my homework
Great posts. With thanks!
buy essay service [url=https://argumentativethesis.com/]write a thesis statement for your argument[/url] thesis statement expository essay [url=https://bestmasterthesiswritingservice.com/]good thesis statements for research papers[/url] thesis statement apa assignment writing service dublin [url=https://payforanessaysonline.com/]buy essay now[/url] buy admission essay [url=https://buycheapessaysonline.com/]pay for research paper[/url] buy an essay online cheap
Ahaa, itѕ gooɗ conversation гegarding thіs paragraph һere at this webpage, I
have read alll tһɑt, ѕo now me also commenting at tһis
pⅼace.
BAT is short for Basic Attention Token. BAT is a crypto asset, and a key (but totally optional) part of the Brave Rewards ecosystem. Here’s how it works: Bitcoin transactions allow for a custom logic to be implemented, enabling a myriad of financial transaction types such as escrow and shared ownership. However, for the purpose of this article, we restrict ourselves to simple person-to-person payments. These can be divided into 2 categories, each affected differently by a quantum computer. Earn crypto tokens for your attention by opting in to privacy-preserving, first-party ads. We help you transform complex problems into breakthrough solutions. Client-side encryption means all of your data is encrypted on your device before any of your information touches our web servers. No server-side hacks and no malware = safe assets. Only you and you alone have access to control your cryptocurrency assets — the way it should be.
https://raymondggda740741.blogofoto.com/51104130/article-under-review
Ethernity Chain is a blockchain-based application that enables take benefit of non-fungible tokens’ rising popularity (NFTs). In the last 24 hours, Ethernity Chain has gained 0.71 percent. With a live market cap of $160,572,782 USD, the current CoinMarketCap ranking is #305. There are 11,278,369 ERN coins in circulation, with a total quantity of 30,000,000 ERN coins. How do you feel about Ethernity Chain today? Vote to see results ©2023 InvestorPlace Media, LLC When it comes to cryptocurrency exchanges, it doesn’t get much bigger than Coinbase and eToro. The two exchanges have made their way to the top of the market with over 100 million combined users from all across the globe. These exchanges are there to help people get into the world of crypto through a safe, community-like environment, offering as much information as possible about potential investments into the blockchain-based world of digital trading.
Do you mind if I quote a few of your posts as long as I provide credit and sources back to your blog?
My website is in the very same niche as yours and
my visitors would genuinely benefit from some
of the information you present here. Please let me know if this okay with you.
Cheers!
I’m gone to inform my ⅼittle brother, tһat һe should also pay a vsit tһіs webb site
on regular basis to get updated from ⅼatest іnformation.
Ӏt’s a shame үou don’t have а donate button! I’ⅾ
certɑinly donate tο thnis excellent blog!
I guess for now i’ll settle fоr bookmarking and adding yօur RSS feed to mу Google account.
Ι look forfward to brand neᴡ updates and wіll share thijs site ѡith my Facebook gгoup.
Talk sоon!
Hey Iknow this is off tlpic Ьut I was wondering if you knew of any widgets I cοuld
add to my blog that automatically tweet mу newеst twitter
updates. Ι’vе een looҝing for a plug-іn like this foor quite ѕome tіme and ᴡas hoping mаybe you
wоuld haѵе some experience wіth sοmething liқe this.
Please let me know iif yоu run into anything.
I truly enjoy reading ʏour blog and I look forward to your new updates.
Gret article! Tһis iis the kind of inf that
should Ƅе shared aaround the web. Shame on Google for not positioning this put up higher!
Comee oon over aand tɑlk ovewr with my web sitе .
Thnk you =)
At Dіscreet.Salе we love what we do, and we nly sell weed and hash.
Now yօu can purchasе oսr produϲts directly froom our store conveniently and ԝithout all the
hasske off trekkiɡ over to a dealer iin the cold or going
to sketchy places. Orderinnɡ wіthh us is as simple as signing up for an account, ρlacing your
order, and submitting рayment viɑ Bitcoin or other Cryptocurrencies.
Checdk oᥙt our curгent available Weeⅾ and Hash.
Discreet.Sale
At Discгeet.Ѕale ѡe love wһat we do, and we only sell
weeɗ aand hash.
Now youu can purchase ourr products directly from our store conveniently and wiοthout all the hassle
of treҝking over to a dealer in the cοld or ցoing to skeetchy placеs.
Ordering with us is as ѕimple as signing up foor an account, placing
your order, and sᥙbmittіng payment via Bitcoі or other Cryptocurrencies.
Check out our current availoable Weed and Hash.
Discreet.Sale
Internet-Spielbanken bieten verschiedene Online Roulette Spiele, von denen es jeweils eine kostenlose und eine kostenpflichtige Version gibt. Das hat für euch den Vorteil, dass ihr erst einmal Online Roulette kostenlos spielen könnt, um euch an das Spiel und seine Eigenheiten zu gewöhnen. Im Anschluss habt ihr die Möglichkeit, euer Können mit dem Einsatz von echtem Geld zu einem Gewinn zu machen. Dabei müsst ihr kein Risiko eingehen, denn es gibt bereits Angebote fürs Roulettespielen mit wenigen Cent als Einsatz. In diesem Fall erfolgt mit jedem Einsatz bei einem Gewinn beim Roulette online kostenlos spielen die Erhöhung um eine Welteinheit. Im Gegenzug dazu wird der Verlust um jeweils eine Welteinheit reduziert. Das Problem hierbei liegt darin, dass der Mindestwetteinsatz immer mindestens eine Welteinheit höher sein muss als das Minimum. Die Chance auf einen Gewinn ist nur noch sehr gering, wenn der Spieler zu Beginn gleich mehrere Runden beim Roulette online kostenlos spielen verliert. Egal welches dieser beiden D’Ambert Systeme der Roulettespiele nutzt: bei einem Verlust gilt es immer einen ruhigen Kopf zu bewahren.
https://demo.sngine.com/casinofilme
Kein Online Casino hat natürlich irgendwelches Geld als gratis Bonus zu verschenken. Wer sich die hohen Auszahlungsraten von 95 bis 98 Prozent anschaut, wird schnell erkennen, dass die virtuellen Spielhallen mit sehr geringen Gewinnmargen arbeiten. Daher ist es nur logisch, dass die Online Casino Boni mit entsprechenden Umsatzbedingungen verbunden sind. Anhand dieser lässt sich auch die tatsächliche Werthaltigkeit der Casino Bonus Angebote ablesen. Nicht immer ist der höchste Casino Bonus auch der beste. Und nicht immer ist jeder Casino Bonus ohne Einzahlung oder die Freispiele ohne Einzahlung als gratis Guthaben ohne Weiteres erhältlich. Der Bonus ist ein fantastischer Vorteil, den Sie nutzen können, wenn Sie im Casino online um Echtgeld zocken möchten. Neukunden in Online Casinos werden von allen guten Anbietern meist mit einem großzügigen Willkommensbonus belohnt.
At Discreet.Տale we love what we do, and
we only sell weed and hash.
Now you can purchase our products directly from our store
convenientⅼy and wіthߋut all the hasslе of trekking օver to a dealer in the cold or going tо sketchy places.
Ordering with us is as simple as signing up for an account,
placing youг order, and submitting payment via Bitcoin or
other Cryptocurrencies. Check out our current available Weed and Hash.
Discreet.Sɑle
Hey! Quick question that’s totally off topic.
Do you know how to make your site mobile
friendly? My weblog looks weird when viewing from my apple iphone.
I’m trying to find a template or plugin that might
be able to correct this issue. If you have any
suggestions, please share. Thanks!
Прогон сайта с использованием программы “Хрумер” – это способ автоматизированного продвижения ресурса в поисковых системах. Этот софт позволяет оптимизировать сайт с точки зрения SEO, повышая его видимость и рейтинг в выдаче поисковых систем.
Хрумер способен выполнять множество задач, таких как автоматическое размещение комментариев, создание форумных постов, а также генерацию большого количества обратных ссылок. Эти методы могут привести к быстрому увеличению посещаемости сайта, однако их надо использовать осторожно, так как неправильное применение может привести к санкциям со стороны поисковых систем.
[url=https://kwork.ru/links/29580348/ssylochniy-progon-khrummer-xrumer-do-60-k-ssylok]Прогон сайта[/url] “Хрумером” требует навыков и знаний в области SEO. Важно помнить, что качество контента и органичность ссылок играют важную роль в ранжировании. Применение Хрумера должно быть частью комплексной стратегии продвижения, а не единственным методом.
Важно также следить за изменениями в алгоритмах поисковых систем, чтобы адаптировать свою стратегию к новым требованиям. В итоге, прогон сайта “Хрумером” может быть полезным инструментом для SEO, но его использование должно быть осмотрительным и в соответствии с лучшими практиками.
Keep on writing, great job!
brillx casino официальный мобильная версия
https://brillx-kazino.com
В 2023 году Brillx предлагает совершенно новые уровни азарта. Мы гордимся тем, что привносим инновации в каждый аспект игрового процесса. Наши разработчики работают над уникальными и захватывающими играми, которые вы не найдете больше нигде. От момента входа на сайт до момента, когда вы выигрываете крупную сумму на наших аппаратах, вы будете окружены неповторимой атмосферой удовольствия и удачи.Так что не упустите свой шанс — зайдите на официальный сайт Brillx Казино прямо сейчас, и погрузитесь в захватывающий мир азартных игр вместе с нами! Бриллкс казино ждет вас с открытыми объятиями, чтобы подарить незабываемые эмоции и шанс на невероятные выигрыши. Сделайте свою игру еще ярче и удачливее — играйте на Brillx Казино!
Ƭheгe is certainly a lot to find outt about thiѕ
topic. І really like аll of tһe points you maԁe.
Hey I know this is off topic but I was wondering if you knew of any widgets
I could add to my blog that automatically tweet my newest twitter updates.
I’ve been looking for a plug-in like this for quite some time and was hoping maybe
you would have some experience with something like this.
Please let me know if you run into anything.
I truly enjoy reading your blog and I look forward to your
new updates.
I love it when folks get together and share views.
Great blog, stick with it!
Hello, Neat post. There’s a problem together with your web site in internet explorer, may check this?
IE nonetheless is the marketplace chief and a good element of people will leave out your wonderful writing due to
this problem.
Today, I went to the beach front with my children. I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She placed the shell to her ear and screamed.
There was a hermit crab inside and it pinched her ear.
She never wants to go back! LoL I know this is totally off topic but I had to tell someone!
What i do not understood іs iin fact how you’гe not actually ɑ l᧐t morе well-appreciated than you mаʏ Ƅe riɡht now.
You are verү intelligent. Үou understand tһerefore siցnificantly ᴡith rеgards tߋ thіѕ topic, produced me fⲟr mmy
part imagine іt from numerous varied angles.
Its like men and women аren’t fascinated except
it’ѕ one thіng to ⅾo with Woman gaga! Your individual stuffs
nice. Aⅼways deal wіth it up!
This is my first time pay a visit at here and i am truly happy to read everthing at one place.
Wow, fantastic weblog structure! Нow lengthy һave you been runnin ɑ
blog for? yoս made running a blog glance easy.
Τhe entire lopok оff yοur webnsite іs excellent, аs smartly ɑs the content!
Ӏt’ѕ wonderful tuat you are getting ideas fгom tһis paragraph
aas ᴡell as from our dialogue mɑԁе hеre.
Thanks for every other fantastic post. Where else may anybody get
that kind of information in such a perfect manner of writing?
I have a presentation subsequent week, and I am on the search
for such information.
Hello to every body, it’s my first pay a visit of this webpage; this
blog consists of amazing and really good data in favor of readers.
If some one desires to be updated with most up-to-date technologies afterward he must
be go to see this web page and be up to date every day.
Hello there, I found your web site by the use of Google whilst looking for a similar matter, your site goot here up, it seems good.
I have bookmarked it in my google bookmarks.
Hi there, just became aware off your weblog via Google, and located that it’s really informative.
I am gonna watch out for brussels. I’ll be grateful if you happen to proceed this in future.
A lot of other people might be benefited from your writing.
Cheers!
May I simply just say what a relief to uncover somebody that genuinely knows what they are talking about on the internet.
You definitely realize how to bring a problem to light and make it important.
More and more people need to look at this and understand this side of your story.
I was surprised you’re not more popular since you certainly have the gift.
%%
Simply wish to say your article is as surprising.
The clearness in your post is just excellent and i can assume you
are an expert on this subject. Fine with your permission let me to grab your feed to
keep up to date with forthcoming post. Thanks
a million and please keep up the gratifying work.
Hello! This is kind of off topic but I need some advice from an established blog.
Is it tough to set up your own blog? I’m not very techincal but
I can figure things out pretty quick. I’m thinking about setting up my own but I’m not sure where to
begin. Do you have any tips or suggestions?
Cheers
Hey There. I found your blog using msn. This is a very well written article.
I’ll be sure to bookmark it and come back to read more
of your useful info. Thanks for the post. I will definitely return.
Hello! This is kind of off topic but I need some advice from an established blog.
Is it hard to set up your own blog? I’m not very techincal
but I can figure things out pretty quick. I’m thinking about setting up my own but I’m
not sure where to begin. Do you have any points or suggestions?
With thanks
I really love your site.. Very nice colors & theme. Did you develop this web site yourself?
Please reply back as I’m wanting to create my own blog and would love to
learn where you got this from or what the theme is called.
Appreciate it!
Aw,this ԝaѕ a reаlly good post. Ƭaking a fеw mіnutes and actual effort
t᧐ produce a good article… but what cɑn I
saү… І procrastinate ɑ ԝhole lߋt and don’t sеem to ցet nearly anything dоne.
Inspiring story there. What happened after? Good
luck!
I am sure this article has touched all thee internet visitors,
its really really fastidious piece of wriing on building
up new blog.
Great delivery. Sound arguments. Keep up the good effort.
Fantastic beat ! I wish to apprentice at the same time as you amend your
web site, how can i subscribe for a blog website? The account aided me a applicable deal.
I were a little bit acquainted of this your broadcast offered brilliant clear idea
Admiring the time and effort you put into your website and in depth information you
provide. It’s good to come across a blog every once in a while that isn’t the same old rehashed information. Great read!
I’ve saved your site and I’m adding your RSS feeds to my Google account.
I have read a few just right stuff here. Certainly worth bookmarking for revisiting.
I surprise how much effort you set to create such
a magnificent informative web site.
essay my favourite tv programme https://buy-essays-online-ds-d19255.webdesign96.com/23892712/buy-essays-online-d-sd-an-overview pan africanism essay
Hi, for all time i used to check website posts here in the early
hours in the morning, as i love to find out more and more.
Having read this I thought it was really enlightening.
I appreciate you finding the time and effort to put this informative article together.
I once again find myself spending a significant amount
of time both reading and leaving comments. But so what,
it was still worth it!
Ahaa, its fastidious conversation about this paragraph here
at this web site, I have read all that, so at this time me also commenting at this place.
Hi, i think that i saw you visited my site so i came to “return the favor”.I’m attempting to find things to
improve my website!I suppose its ok to use some of your ideas!!
I like the helpful information you provide in your articles.
I’ll bookmark your weblog and check again here frequently.
I am quite certain I will learn many new stuff right here!
Best of luck for the next!
Wow that was odd. I just wrote an extremely long comment but after I clicked submit my comment didn’t show up.
Grrrr… well I’m not writing all that over again. Anyhow, just
wanted to say wonderful blog!
We would like to thank you yet again for the beautiful ideas you gave Jesse when preparing her own post-graduate research plus, most importantly, pertaining
to providing all of the ideas within a blog post. Provided we had been aware of your web page a year ago, i’d have been rescued from the needless measures we were selecting.
Thanks to you. toys for adults
Oh my goodness! Incredible article dude! Many thanks,
However I am having troubles with your RSS. I don’t understand
why I am unable to subscribe to it. Is there anybody having similar RSS issues?
Anyone who knows the solution will you kindly respond?
Thanx!! I saw similar here: dobry sklep and also here: dobry sklep
I am really impressed along with your writing abilities as well as with the layout to your
weblog. Is this a paid subject matter or did you
customize it yourself? Anyway keep up the excellent high quality writing,
it’s rare to peer a nice weblog like this one these days..
I saw similar here: sklep online and also here:
sklep online
Heya i am for the first time here. I found this board and I find It really useful & it helped me out a lot. I hope to give something back and help others like you helped me.|
Keep on working, great job!|
Very descriptive blog, I liked that a lot. Will there be a part 2?
I saw similar here: e-commerce and also here: sklep
I’ve been exploring for a little for any high-quality articles or
blog posts on this kind of area . Exploring in Yahoo I finally stumbled upon this web site.
Reading this information So i am glad to show that I have an incredibly excellent uncanny feeling I came
upon exactly what I needed. I such a lot without a doubt will make certain to do not disregard
this web site and provides it a look regularly.
І’m not sure wjere үou’re ցetting уour іnformation, but grеat topic.
I needs toо spend some timе learning more
or understanding mοre. Tһanks foг great
information I wɑs looking for this info for my mission.
Every weekend i used to visit this web page, because i want enjoyment, since this this web site conations really pleasant funny material too.
Hey wouⅼd yoou mind stating ԝhich blog platform ʏou’re using?
I’m loоking too start mʏ ߋwn blog soon but І’m
haviing a hard time choosing between BlogEngine/Wordpress/В2evolution andd
Drupal. Thhe reason Ι ask is bеcaսѕe your design seeems
ⅾifferent tһen moѕt blogs and I’m looking for somethіng comρletely unique.
P.S Ꮇy apologies for Ƅeing off-topic buut I had
tto ask!
This is very interesting, You are a very skilled blogger.
I’ve joined your feed and look forward to seeking more of your fantastic post.
Also, I have shared your website in my social networks!
Hiya very cool site!! Guy .. Excellent ..
Superb .. I will bookmark your website and take the feeds also?
I am satisfied to seek out a lot of helpful info
here in the publish, we want work out extra techniques in this
regard, thanks for sharing. . . . . .
I do not know if it’s just me or if everybody else experiencing problems with
your website. It looks like some of the written text on your posts are running off
the screen. Can someone else please provide feedback and let me
know if this is happening to them as well? This may be a issue with
my browser because I’ve had this happen previously. Appreciate
it
It’s not my first time to pay a quick visit this web page, i am browsing this site dailly and get good facts from here every
day.
When somneone writes ann post he/she maintains
the image of a user in his/her mind that how a uaer can know it.
So that’s why this piece of writing is outstdanding. Thanks!
Hi to every body, it’s my first pay a visit of this webpage;
this web site includes awesome and actually good information for
readers.
Spot on with this write-up, I really believe this
website needs a lot more attention. I’ll probably be returning to see more, thanks for the info!
Nice post. I was checking constantly this blog and I’m impressed!
Very helpful information specifically the last
part 🙂 I care for such info much. I was seeking this certain information for a long
time. Thank you and good luck.
There is certainly a great deal to know about this issue.
I love all the points you made.
Pretty! This has been an incredibly wonderful post.
Many thanks for providing these details.
Hmm it seems like your website ate my first comment (it was extremely long) so I guess I’ll just sum it up what I had written and say, I’m thoroughly
enjoying your blog. I as well am an aspiring blog blogger but I’m still
new to the whole thing. Do you have any suggestions for beginner blog writers?
I’d really appreciate it.
I go to see each day some blogs and blogs to read content, except this website provides
feature based posts.
Greetings from Carolina! I’m bored at work so I decided to browse your website on my iphone during lunch break.
I love the knowledge you provide here and can’t wait to take a look when I get home.
I’m surprised at how fast your blog loaded on my phone ..
I’m not even using WIFI, just 3G .. Anyways, excellent
blog!
Hello, Neat post. There is a problem along with your website in internet explorer, would check this?
IE nonetheless is the market leader and a good element
of folks will leave out your great writing because of this problem.
Hello there! Do you know if they make any plugins to safeguard against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on. Any suggestions?
Wow, wonderful blog layout! How lengthy have you been blogging for?
you made running a blog glance easy. The full look of your website is magnificent, let alone
the content! You can see similar: e-commerce and here ecommerce
Bally’s Black Hawk Poker Room is housed in a moderate-sized casino in the striking setting of Black Hawk, Colorado. Black Hawk and its contiguous neighbor Central City hold more than 18 casinos, four of which have poker rooms (The Monarch, Bally’s, Isle Casino, and Ameristar). We have previously described Black Hawk in detail. Please refer… WE’RE COMMITTED TO FAIRNESS.That includes everything from how you’re compensated, to how you’re treated on the job. We firmly believe that all our team members – from the casino floor to the corner office – have a fundamental right to respect and fairness. ReportLLori With over 120 vendors in attendance, the event promises to be a hub of activity for anyone looking to expand their network, learn about new products, and snag some great deals. Attendees can expect to encounter new ideas, exciting games, and a chance to win fantastic prizes.
https://israelcaxv518518.blogadvize.com/25895962/play-poker-and-earn-paytm-money-in-south-africa
You can email the site owner to let them know you were blocked. Please include what you were doing when this page came up and the Cloudflare Ray ID found at the bottom of this page. You can email the site owner to let them know you were blocked. Please include what you were doing when this page came up and the Cloudflare Ray ID found at the bottom of this page. You can email the site owner to let them know you were blocked. Please include what you were doing when this page came up and the Cloudflare Ray ID found at the bottom of this page. You can email the site owner to let them know you were blocked. Please include what you were doing when this page came up and the Cloudflare Ray ID found at the bottom of this page. You can email the site owner to let them know you were blocked. Please include what you were doing when this page came up and the Cloudflare Ray ID found at the bottom of this page.
I’m extremely impressed with your writing skills as well as with
the layout on your blog. Is this a paid theme or did you customize it yourself?
Anyway keep up the nice quality writing, it’s rare to see a great blog like this one today.
I saw similar here: najlepszy sklep and also here: sklep online
It’s remarkable for me to have a web site, which is helpful in favor of my know-how.
thanks admin I saw similar here: najlepszy sklep and
also here: najlepszy sklep
order zithromax
It’s nearly impossible to find knowledgeable people for this subject, but you sound like you know
what you’re talking about! Thanks I saw similar
here: ecommerce and also here: sklep
is 500mg of metformin: a low dose
Very nice article, just what I wanted to find.
Remarkable! Its really awesome piece of writing, I have got much clear idea concerning from
this article.
Wow, amazing weblog layout! How lengthy have you been running a
blog for? you make blogging glance easy. The overall look of
your site is magnificent, as smartly as the content!
You can see similar: najlepszy sklep and here dobry sklep
what is lisinopril used for
lexapro vs zoloft weight gain
what is flagyl for dogs
furosemide label
Howdy! This is my first visit to your blog! We are a group of volunteers and starting a new initiative in a community in the same niche.
Your blog provided us beneficial information to work on. You have done a marvellous job!
can you take gabapentin with tramadol
glucophage ilacabak
active ingredient in zithromax
Whats up this is kinda of off topic but I was wanting to know
if blogs use WYSIWYG editors or if you have to manually
code with HTML. I’m starting a blog soon but
have no coding knowledge so I wanted to get advice from someone with
experience. Any help would be enormously appreciated!
I am regular reader, how are you everybody? This paragraph posted at this web page is truly
fastidious.
lasix equivalent
Amazing blog! Do you have any tips and hints for aspiring writers?
I’m planning to start my own blog soon but I’m a little lost on everything.
Would you recommend starting with a free platform like WordPress
or go for a paid option? There are so many choices out there that I’m totally overwhelmed ..
Any recommendations? Cheers!
amoxicillin with or without food
Hi! I know this is kind of off topic but I was wondering if
you knew where I could locate a captcha plugin for my
comment form? I’m using the same blog platform as yours and I’m having problems finding one?
Thanks a lot!
how long can you take gabapentin
It’s very interesting! If you need help, look here: hitman agency
Thank you for the good writeup. It in fact was
a amusement account it. Look advanced to far introduced
agreeable from you! However, how can we keep up a correspondence?
Hi there every one, here every person is sharing such familiarity,
therefore it’s good to read this webpage, and I used to visit
this webpage every day.
where can i buy ciprofloxacin 500mg tablets
how much cephalexin should i take for tooth infection
I am now not positive the place you’re getting your
info, but good topic. I must spend some time studying much more or understanding more.
Thank you for great info I was looking for this information for
my mission.
What’s up to every one, because I am truly eager of reading
this blog’s post to be updated daily. It includes nice information.
I am sure this piece of writing has touched all the internet viewers, its really
really nice post on building up new web site. I saw similar
here: sklep online and also here: najlepszy sklep
bactrim ds uses
Marvelous, what a webpage it is! This blog provides useful information to us, keep it up.
does cephalexin treat kidney infection
can you take amoxicillin while breastfeeding
Wow, wonderful blog layout! How long have you been blogging for?
you made blogging look easy. The overall look of your site
is fantastic, let alone the content!
This paragraph is genuinely a good one it assists new
net viewers, who are wishing in favor of blogging.
bactrim pregnancy
With havin so much written content do you ever run into any
issues of plagorism or copyright infringement?
My blog has a lot of completely unique content I’ve either authored myself or outsourced but it seems a lot of it is popping it up all over the internet without my agreement.
Do you know any solutions to help reduce content from being ripped
off? I’d really appreciate it.
This piece of writing will help the internet visitors for creating new
webpage or even a blog from start to end.
It’s very simple to find out any topic on web as compared to textbooks, as I found this
piece of writing at this website.
Excellent article. I’m facing many of these issues as well..
This post offers clear idea for the new viewers of
blogging, that truly how to do blogging.
escitalopram 10mg
gabapentin 300mg price
Hi would you mind sharing which blog platform you’re working with?
I’m going to start my own blog in the near future but I’m having a hard time deciding between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design seems different
then most blogs and I’m looking for something completely unique.
P.S Sorry for getting off-topic but I had to ask!
Hi, Neat post. There’s an issue with your web site in web explorer, would check this?
IE nonetheless is the market chief and a big part of other people will miss
your magnificent writing because of this problem.
depakote level
It’s really a great and useful piece of information. I am happy
that you simply shared this useful information with us.
Please stay us informed like this. Thank you for sharing.
ddavp drops uk
cozaar hct
citalopram and sexdrive
This post will assist the internet people for setting up new
website or even a blog from start to end.
Thanks very interesting blog!
depakote sprinkles dosage
cozaar hydrochlorothiazide
citalopram 20
I’ve been exploring for a little bit for any high-quality
articles or weblog posts on this sort of area .
Exploring in Yahoo I finally stumbled upon this site.
Reading this information So i am satisfied to show that I have a very excellent uncanny feeling I came upon just what I needed.
I so much indisputably will make certain to don?t forget this site and provides it a look regularly.
what is diclofenac sodium topical gel 1 used for
augmentin dosage
verapamil diltiazem
ezetimibe npc1
how fast does flexeril work
I always spent my half an hour to read this website’s content daily along with a cup of coffee.
flomax allergy to sulfa
control yawning