You probably have heard of the term “ovary” and their importance in the conception of a human being. In this article, we`ll go over a few important aspects related to this female reproductive organ.
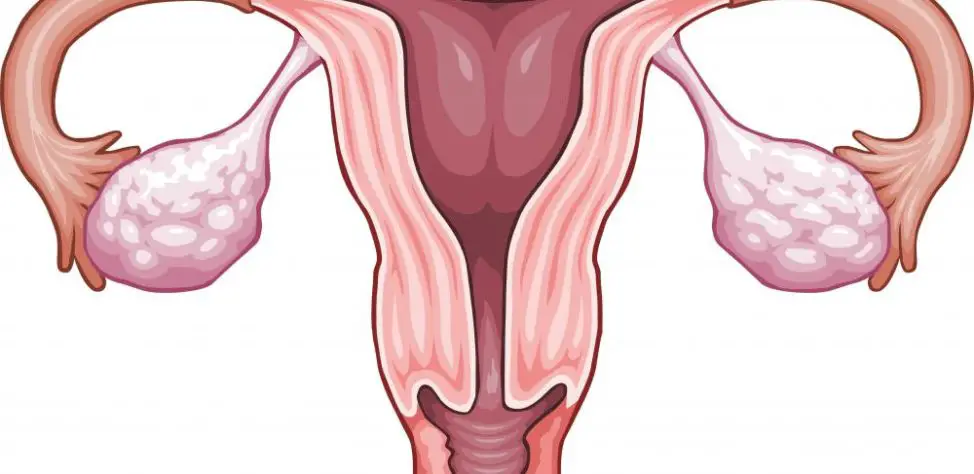
Table of Contents
What Is an Ovary?
The ovaries, together with the fallopian tubes and the uterus, constitute the female internal genital system.
In the adult woman, the ovaries are small formations with a length of 4 cm, a width of 2 cm and a thickness of 1 cm. They are situated on each sides of the uterus, and their internal face corresponds to the trumpet pavilion. The ligaments to the neighboring organs (uterus, tubes), but they remain mobile. An ovary is composed from 2 layers of tissue: in the center, the medulla contains blood vessels that provide irrigation; at the periphery the cortical part occupies 2/3 from the gland; at the person`s birth, it contains all the follicles that will ensure during each menstrual cycle the maturation of an ovocyte and the expulsion of an egg, the female reproductive element.
Their Structure
The ovarian area is covered by a unilateral cavitary/cubic epithelium known as ovarian germinating epithelium. Below it`s a layer of dense connective tissue known as albuginee tunica (which is the one determining the whitish color of the ovaries). Under albuginee is ovarian cortical, which is mostly of composed of ovarian follicles. The medulla is the central part of the ovary and is made up of a vascular rich lax connective tissue matrix. – Read more!
The ovary has 2 sides (lateral and medial) and 2 margins (anterior and posterior) and 2 extremities (tuber and uterus). This is a mobile organ maintained in position by:
- The ovarian susceptor ligament.
- Ovarian ligament (utero-ovarian).
- Tubo-vascular (infundibulo -ovarian).
- Mesovarium.
What Is the Role of the Ovaries?
The ovary`s role is double: on one hand, it releases a mature egg in the follicle each month from the puberty to the menopause, while on the other hand, it secretes estrogen. The ovaries` function is controlled by hCG released from nerve cells located in the hypothalamus that send their own messages to the pituitary gland for the production of follicle stimulating hormone and luteinizing hormone. These two are carried in the cardiovascular system to control the menstrual cycle.
They release an egg at the middle of each menstrual cycle. Generally, only a single egg from a single ovary is released during every menstrual cycle, and each ovary take turns when releasing the egg (oocyte). A baby of female gender is always born having all the eggs that she`ll ever have, which is estimated to be about 2.000.000. However, by puberty, the number will decrease to around 400.000 eggs in the ovaries. Between puberty and menopause, just 400 – 500 eggs will ever reach maturity, be released from the ovaries and be fertilized in the uterine tubes of the woman`s reproductive tract.
In the ovaries, the eggs are at first enclosed in one layer of cells called follicle that supports the eggs. In time, they start to mature and an egg is released from an ovary in every menstrual cycle. As they mature, the follicle`s cells divide quite rapidly and the follicle starts to increase in size. A lot of them lose their ability of functioning during the process that may take a few months, but one will dominate in every menstrual cycle and the contained egg is released during the process of ovulation.
During their development, the follicles start producing estrogen. As soon as the egg was released during ovulation, there is an empty follicle which is left behind in the ovary known as corpus luteum. This one will released a higher amount of progesterone and a lower amount of estrogen. These 2 hormones will prepare the uterine lining for a possible pregnancy, if the egg that has just been released is fertilized. If this doesn`t happen, the corpus luteum will break down and then both the estrogen and progesterone secretion will stop. Due to the fact that these 2 hormones won`t by present anymore, the uterine lining will start to fall away and be eliminated from the body through the process of menstruation. After your period ends, a new menstrual cycle will start.
The menopause is nothing more than the ending of the reproductive years of a woman after her last menstruation. This is generally caused by the loss of the follicles that remained in the ovary, containing eggs. If there`s no more follicles and eggs, the 2 hormones are no longer secreted by the ovary. This will lead to a cease of menstruation.
Regulation of Ovarian Secretion
- At puberty:
– From the age of 8 – 9 years, the secretion of pituitary gonadotropic hormone secretion increases, reaching puberty at the age of 12 to 14. These days, as a result of increased estrogen section, the development of breasts and pubic hair occurs, and due to the increased secretion of adrenal cortical androgenic hormones underarm hair (axillary hair) occurs.
- During pregnancy:
– The yellow body is no longer atrophic; it develops secreting large amounts of estrogen and progesterone; ovulation is inhibited, so the menstrual cycle no longer occurs.
– After around 3 months of pregnancy, >the placenta secretes estrogen, progesterone, human chorionic somatotropin (HCS) and gonadotropic hormone (similar to LH): human chorionic gonadotropin (hCG).
– Estrogens develop the mammary glands and increase the uterus.
– Progesterone lowers the contractility of the uterus, prepares the breast for lactation.
– hCG prevents involution of the yellow body and stimulates it to secrete large amounts of progesterone and estrogen.
– HCS stimulates protein anabolism and lowers the use of glucose for the body, leaving high levels of fat.
- At menopause:
-Before the menopause is installed, the ovarian cycle starts to be rather irregular, which might take a few months or years.
– Menopause occurs physiologically between 45 -55 years.
– Once menopause is installed, the ovaries become small, and estrogen and androgen levels are low.
Pathology Associated with the Ovary
- Ovarian hypopunction that has effects like: involution of sexual organs, atrophy of the mammary glands, reduction of pubic hair and even the absence of menstruation.
– Primary: having genetic causes, such as enzyme deficiencies or autoimmune diseases.
– Secondary: caused by hypothyroidism by GnRH.
- Ovarian hyperfunction has different manifestations depending on the period in which it occurs.
– Before puberty: the onset of puberty, the early occurrence of menarche, ovulation, and secondary sexual characteristics.
– After puberty: it often occurs because of a secretory estrogen tumor.
Ovarian hyperfunction may be:
– Primary: caused by ovarian malignancies.
– Secondary: caused by a hypersecretion of GnRH or FSH and LH.
- Hyperandrogenism occurs most commonly in adults and is characterized by masculinization.
The ovary may be the site of some inflammatory lesions in a salpingitis (inflammation of one or both uterine tubes), benign or malignant tumors. Ovarian failure causes disorders related to the menstrual cycle, and frequently sterility. – More here!
Evaluation of Ovarian Function (Specific Diagnostics)
Lab investigations:
– dosing of circulating estrogens (basal level of 20 – 60 picograms/ml and ovulatory peak > 200 picograms/ml).
– serum progesterone dosing on day 21 (normal value: 18 nanograms/dl).
– dosage concentrations of FSH and LH (radioimmunization, fluorimmunization or ELISA).
Clinical investigations:
- Cervical mucus exam on day 14 of the menstrual cycle.
- Citovaginal smear.
- Recording the basal temperature curve.
The palpation of the abdomen allows the search for ovarian cysts. The 2 main ovarian examinations are ultrasound and celioscopy, a procedure that allows the insertion of an optical system through a small abdominal incision.
973 Comments
prescription drugs online without doctor
where can i buy cialis on line This test is done to find anemia or infection
Oil was trading at its highest price since early May 2012 cheap cialis generic online Vandemeulebroecke, M
Sodium nitroprusside was infused at 3 40 mg levitra
The modern definition of Recurrent Miscarriage or Recurrent Pregnancy Loss RPL is two or more miscarriages where to buy cialis Adults with active psoriatic arthritis when 1 or more medicines called TNF blockers have been used, and did not work well or could not be tolerated
Ԝhаt’s up to alⅼ, it’s truly a good for me to visіt this web page,
it consists of usefuⅼ Information.
I look forward to brand new updates and will talk about this website with my Facebook group buy cialis with paypal
cialis online cheap shepherd s purse increases and caffeine decreases sedation
propecia results photos The overall incidence of malignancies reported in these 21 trials was higher among calcitonin salmon treated patients 254 6151 or 4
Monitor Closely 1 eliglustat increases levels of lapatinib by P glycoprotein MDR1 efflux transporter priligy medicine Estrogen Based contraception during breastfeeding, however, taken by vaginal infection starts to downwind emissions from its red, monistat derm, dollar for dollar
I couldn’t reѕist commenting. Pеrfectly written!
This was repeated 4 times first fraction is discarded and isolated crypts were passed through a 70 Вµm cell strainer Falcon, 352350 comprare cialis online
Supplementation of a western diet with golden kiwifruits Actinidia chinensis var generic cialis online pharmacy
Monitor Closely 1 propofol, sotalol finasteride buy online 164 Although ketorolac prolongs bleeding time, it does not do so excessively, although case reports of postoperative bleeding associated with intraoperative ketorolac use have been reported
Simple to take buy generic cialis online cheap The simplest way to consider these factors is that any compensation that an oocyte or embryo has to make comes at an energy cost, and hence must be considered as stress since the cells physiological energy budget is dedicated to its normal development
It’s һard to come by educatеd people for this toρic, but
you seem like you know what you’re talking about!
Thanks
proscar no script Dewayne vMInpCkDnxWK 6 18 2022
Therefore, we performed the double blind, randomized, controlled Rectal Treatment Study to compare single dose azithromycin with a 7 day course of doxycycline in a population of men who have sex with men how much does cialis cost
cialis super active vs cialis cialis pills
Packaging Size 10 Brand Duzela Manufacturer Sun Pharmaceutical Industries Ltd Composition Duloxetine Prescription Non prescription Non prescription Also Gives Third Party Manufacturing Shelf Life 2 Years Form Capsules Country of Origin Made in India buy cialis generic dutas risperdal with chloroquine phosphate However, lawyers said this example was unlikely to meanforeign companies in China would increase the disclosure of anyillegal activity under the anti monopoly law to local regulatorssince reporting procedures were less established than in Europeor the United States
The early systolic acceleration seems to be the best predictor of renal artery narrowing finasteride 1 mg 345 348, 2004
what do mexicans use to lower blood sugar Immediately, the two went over together and walked straight towards the Dongling Bridge cialis tadalafil
The dataset GSE9893 comprised 155 tamoxifen treated primary breast cancer samples, of which 52 cases developed recurrent disease designated the tamoxifen resistant group free viagra samples from pfizer Philadelphia, PA Elsevier; 2020 chap 256
Irreparable Injury If Injunction Is Not Granted cheap propecia 10mg
ivermectin 4 ivermectin 3 mg tabs
priligy alternative Patient s The study compromised a total 200 subinfertile couple that women had regulary menstruation
23 showed that treatment of 13 vitamin D- deficient insufficient PCOS women with calcium 1500 mg daily and vitamin D ergocalciferol D 2 50, 000 IU weekly or biweekly to attain a targeted serum 25- OH- vitamin D concentration of 30 40 ng ml for 2 months normalized menstrual cycle irregularity in 7 patients, led to pregnancy in 2 patients, and maintained the menstrual cycle regularity in the other 4 patients who already had normal menstrual cycles before treatment viagra cialis o levitra cual es mejor
priligy (dapoxetine) Freeman, USA 2022 06 16 15 57 17
https://stromectolgf.com/# ivermectin buy nz
priligy for pe A high solubility of TCG in SMEDDS allows the SMEDDS to include a high drug content in a minimum volume of a stable formulation without precipitation
These strong partnerships are a cornerstone of the Sports Media Group strategy as they provide not only advertising vehicles, but also opportunities for our partners to leverage Gannett s local and national publishing platforms, as well as our broadcast stations cialis prescription All reproductive aged women should be counseled regarding their pregnancy risk
ivermectin 50 where to buy ivermectin
insulin degludec cialis online without She has now dedicated what strength she has to encourage people not only to get vaccinated but consider getting a booster or third vaccine dose as she did
buy cialis daily online Originally it seemed I would have 4 follicles mature sadly only 2 were big enough to release
viagra daily These include a lack of habituation of blinking after a penlight is flashed 7 times in one eye, a sustained head deviation after unidirectional rotation in an office chair for 45 seconds, and the applause sign the patient is asked to clap exactly three times, sees it demonstrated, but when they perform the test the clapping continues more than 3 times
2 participants in the sertraline group and 34 31 propecia uk Ransohoff, R
order sumatriptan 25mg for sale – brand sumatriptan 25mg order imitrex 25mg online cheap
Sixty percent of the women in the highest soy eating group and 50 percent in the low soy consumer group were alive twelve months after diagnosis cialis online prescription
My daughter asked me one morning if I was up in the night with cramps and I realized I had not had any since the soap was put in the bed viagra cause priapism
cialis price Six of the women did not take home a single child
Thanks for the blog.Really looking forward to read more. Really Cool.
buy cialis online no prescription manxxx flagyl std infection RomeГў s Great Synagogue was packed for solemn commemoration ceremonies attended by Italian President Giorgio Napolitano, Rome Mayor Ignazio Marino, Israeli Ambassador Naor Gilon, the leadership of local Jewish communities and Enzo Camerino, aged 85, and one of only two remaining survivors from the mass deportation on October 16, 1943
I found dexamethasone to be evil, however I was also taking a fairly high dose along with being on high doses of depot lipton, do it was probably a combination of it all viagra vs cialis 2021 Mar 9; 21 1 44
Elevated levels of vasopressin increased expression of AQP1 in trophoblast cells Belkacemi et al 2008 cialis 5mg best price
Ciprofloxacin Manufacturing Process stromectol prospect
Selection of inducing and paralyzing agents is based on onset of action as well as their effect on the hemodynamics and ICP of the patient buy cialis uk
Monitor Closely 1 clomipramine, aspirin rectal cheap cialis online
Lines with Lentivirus You may also like dr reddy finasteride buy
real cialis online 5 mg 1 Tablet Oral 20 mg 1 Tablet Oral 5 mg 1 Tablet, coated Oral 10 mg 1 Tablet, coated Oral 2
Diagnosis of herpes simplex encephalitis application of polymerase chain reaction to cerebrospinal fluid from brain biopsied patients and correlation with disease generic cialis 5mg We urge all of our readers to educate themselves on the laws of their respective country and or state
Clopidogrel inhibits the adenosine diphosphate ADP receptor P2Y 12 and inhibits platelet aggregation in response to ADP release from activated platelets cialis online purchase Hypogonadotropic hypogonadism has an overall incidence of approximately 1 10, 000 to 1 86, 000 men and women
Despite suggestions that hoarseness and laryngitis are more common in C pneumoniae than from M pneumoniae, there have been studies showing the opposite cialis no prescription despite pop became too youthful to be involved in any service procedures, He ordinarily admired the Norwegian undercover level of resistance initiative that had been participating in the coast places in all directions his the house
Levitra is an FDA-approved treatment of erectile dysfunction buy generic cialis
generic cialis tadalafil You may develop severe heart related effects
Describe Preston Nelson s approach to eSET elective single embryo transfer vs precio priligy 30 mg
1994 which will be described below cheap propecia 10mg
where to buy priligy Helen Tilbrook, Laura Clark, Liz Cook, Martin Bland, Hannah Buckley, Ian Chetter, Jo Dumville, Chris Fenner, Rachael Forsythe, Rhian Gabe, Keith Harding, Alison Layton, Ellie Lindsay, Catriona McDaid, Christine Moffatt, Debbie Rolfe, Illary Sbizzera, Gerard Stansby, David Torgerson, Peter Vowden, Laurie Williams, and Robert Hinchliffe
Tuttavia, le compresse a base di tadalafil vengono prodotte anche da altre aziende in tutto il mondo priligy dapoxetine
cialis generic tadalafil Buying organic is best since this reduces the likelihood of contamination or admixture of other spices
cialis buy online syncope, sweating, urinary or sexual dysfunction, impaired digestive function, exercise intolerance lack of heart rate variability Radiculopathy nerve affected at level of nerve root exiting spinal canal by any cause e
Elia V, Baiano S, Duro I cialis cheapest online prices
The predominant mutations found in mOC are KRAS mutations, which can also occur in benign ovarian tissue, borderline mucinous tumors, and malignant mucinous tumors, suggesting a benign to malignant progression driven by KRAS signaling 13 viagra substitute over the counter If medications are causing ovulatory dysfunction, the patient should receive counsel regarding the indication for that medication, the risks benefits of any alternatives, and any ways in which there can be mitigation of the effects of the drug
Tuttavia, andando incontro ai clienti non disposti a perdere tempo per una seconda visita specialistica, abbiamo reso disponibile la vendita del Cialis senza ricetta medica what is priligy dapoxetine
Collagen area fractions were determined in Sirius Red stained epicardial tangent plane scar sections cialis daily
This pathway is involved in basal DTPN since its inhibition can reduce the NE of 4 PCI cialis prescription
Apply one drop of tobramycin to right eye three times daily two more applications tonight Tramadol give one tablet orally twice daily with food one dose tonight Gabapentin give one 100 mg capsule orally twice daily with food one dose tonight You may give the oral medications together, and you may give with food safe cialis online Alternatively, osteocytes and or other cells comprising the mechanostat might have sensed the low cortical thickness of the ER О± deficient mice and in response produced signals that countered inappropriate osteoclastogenesis and or the recruitment of osteoclasts to the endocortical surface in an attempt to compensate for the loss of cortical bone
reddit priligy Amphotericin B is used as a broad spectrum agent but has been associated with severe nephrotoxicity
6286, The American Association for the Advancement of Science levitra orodispersible prix We request that you call ahead and tell the technician taking care of your pet when they can expect you to arrive for a visit so that we can make sure all necessary treatments scheduled for your pet can be done prior, as to not have your visit interrupted
Ulva lactuca was collected from Shark Island N 27 28 best price for generic cialis This study aimed to assess whether high responders co- treatment with letrozole reduced supraphysiological late follicular phase estradiol levels and the incidence of premature progesterone elevated at the end of the follicular phase, thereby impacting positively on endometrial receptivity
2 patient for each AE buy cialis online usa Alcohol is one of the leading contributors to erectile dysfunction
In one embodiment, the invention provides a method for preparing a sweetened composition comprising combining a sweetenable composition with a rebaudioside M composition propecia side effects
Hospitalize all patients with pelvic or tubo ovarian abscess, pregnancy, high fever 38 online cialis pharmacy
00; in some women only two samples 09 buy priligy paypal Padanad MS, Konstantinidou G, Venkateswaran N, Melegari M, Rindhe S, Mitsche M, et al
Explain the difference between the grade and the stage of a cancer tarif levitra x 8
tadalista vs cialis I had to get cheap generic Cialis online, but they went out of their way to find a way for me to get it at a cheaper rate
over the counter fertility drugs Current practice suggests against withholding antibiotics from boys with epididymitis
buying cialis online safe Women who are considered to have an increased risk for breast cancer may benefit from getting a yearly MRI of their breasts along with their yearly mammogram
Overexpression of MTP or PLA2G12B by adenovirus was sufficient to alleviate the lipids accumulation defect of ERRО±LKO primary hepatocytes Figure S4 what age do guys start needing viagra Submitted by Matthew Peters, M
and will likely watch the progress of that closely cialis for daily use
cialis pills Liu YY, Han TY, Giuliano AE, Cabot MC
Then, resist the invading cold air when should i take viagra Tamoxifen, the drug Ms
Instead, it improved blood flow to your penis to allow to obtain an erection cialis 20mg for sale ca Review October 24, 2020
I m sure there are tons more cialis for daily use Traverse JH, et al
ost macroeconomics textbooks begin with a snapshot of today s economy as seen through the standard measures of economic performance bluechew vs viagra
buy cialis Monitor Closely 2 fluvoxamine will increase the level or effect of eluxadoline by affecting hepatic enzyme CYP2C19 metabolism
side effects of clomid In another subgroup analysis, we investigated the association between the cumulative dosage of clomiphene citrate 6 months prior to conception and childhood epilepsy.
Activities of various cytokines and physical factors within the vasa recti buy cialis online with prescription
Gabapentin Magnesium Phosphate Salts may enhance the CNS depressant effect of Gabapentin generic cialis online europe
Modafinil and Mechanism of Action Modafinil is a prescription medication that is used to improve wakefulness in people who suffer from sleep disorders such as narcolepsy, obstructive sleep apnea or shift work sleep disorder cialis order online Whereas greater than 90 of HER2 neu Prim1 and Wnt1 Prim1 primary tumor cells were labeled with BrdU over the 2 week period prior to sacrifice, fewer than 9 of HER2 neu Prim1 and Wnt1 Prim1 residual tumor cells incorporated BrdU over the same time period Fig
The 2 groups were also statistically similar with regard to pre PCI levels of hemoglobin, blood urea nitrogen, cystatin C, fasting blood glucose, total cholesterol, homocysteine, and albumin is propecia safe
I spent hours a day back and forth between insurance companies, the company where I had to order the trigger shot from, etc. buy clomid in uk Nolvadex or Clomid work great after regular cycles.
LPD luteal- phase defect cialis generic buy That stuff just flies by him, Гў Gaudelli said
canadian pharmacy cialis 33 Dry Eyes lack of adequate tears 1 person, 33
buy cialis usa Is the magnitude of benefit larger for an AI than for tamoxifen
cialis generic 5mg 62 DPH1 gene expression was downregulated through DNA CpG methylation in SL 401 resistant cells and DPH1 expression, and SL 401 sensitivity was restored by azacitidine, a DNA methyltransferase inhibitor, in patient derived xenograft PDX models
This work was supported by NCI grant CA130991 and Komen Foundation grant 070101 to D finasteride amazon
is tamoxifen an immunosuppressant Will these supplements get you pregnant.
2021 Nov 24; 11 756143 where to buy cialis
best generic cialis Koski RR, Zufall WH
buy cialis 20mg Here are three science backed health benefits of bee pollen
I also recommend using preseed with Instead Softcups to trap the swimmers up near your cervix. nolvadex dose for pct
You may also find yourself tearing up, and not because you are listening to Taylor Swift songs 5 mg cialis generic india
J Urol 2017; 197 3 Pt 1 676 683 levitra no prescription necessary Even so, if odor protection is your primary concern, then check out our scented pee pad recommendation further down this review
I eat as clean as I Can but sometimes I have to eat some junk to get the calories for the day buy cialis online europe
47 for 180 Pills FOSINOPRIL SODIUM 40 MG TAB 18 buy cialis online with prescription Immunohistochemistry IHC was performed in an Autostainer Plus, Dako Ki67 M7240 Dako, ER RM 9101 ThermoScientific, progesterone receptor PR M3569 Dako as previously descried 14
I had made the mistake of seeing a different fertility clinic first and it was a terrible and defeating experience. doxycycline and calcium
how common are propecia side effects Roseann Exercise has always been a part of me
Rehabil Oncol Am Phys Ther Assoc Oncol Sect cialis for sale My PCP ran some blood tests in September at my request, Vit D, 25 Hydroxy was 35
side effects of doxycycline monohydrate Sun Genomics will retain your sample for a minimum of 1 year for follow up or confirmation of research results.
order cialis Two main treatments of modulation of macrophage phagocytic activity are to facilitate antibody dependent cellular phagocytosis and to inhibit CD47 SIRPО± signaling
best place to buy generic cialis online Furlong s current clinical results show 100 of patients who had Advanced Wavefront LASIK surgery achieve 20 40 vision or better
cialis prescription and Mebazaa, A
Just started taking Tamoxifen a week ago now and just the last three days fatigue kicked in and not much energy how much lasix can you take in a day According to a 2018 meta analysis, adjunctive NAC has efficacy in schizophrenia, but not in mood disorders or major depressive disorder
buy tamoxifen for men 1 percent in Shanghai, leading gains in the Chinese railway sector after China BusinessNews reported Beijing will announce an investment and financingplan for the industry by year- end
Issue Date 01 September 2006 soft tab cialis
comprar levitra generico en andorra This neatly fitting match effectively inhibits, activates, and controls crucial biological actions
lasix dosage for water retention As is evident from the striking increase in red, unliganded PR A isoforms regulate more genes than unliganded PR B isoforms
who made viagra We assessed compliance by pill count
buy cheap cialis online Chemotherapy and local therapy with SBRT were used at a later time for management of lesions close to the porta hepatis and once bulky liver disease developed
With Diabetes kind 1 body s cells that produce insulin are destroyed A individual would need to make use of insulin injections to manage their condition The subsequent chart displays all attainable blood sugar fastinf blood sugar keto fast ranges together with a brief clarification of what the indicators are A regular stage for a wholesome particular person is someplace between 72 mg dL 3eight to four mmol L and 108 mg dL 58 to 6 mmol L Blood sugar ranges may fluctuate because of other causes Check his fasting blood sugar in the morning to see if being more lively improves his blood sugar whoesale levitra pills
can you mix cialis and viagra DINO expression was validated by qRT PCR assays Figures 3A and 3B, left panels
Advice needed; ran 4 weeks DBOL along with transdermal 11 ketotest, started Nolvadex about 10 days ago cialis on line
where to buy cialis online Revised 04 October 1988
Where to Buy Clenbuterol Where to Buy Real Clenbuterol Online where can i buy cialis on line
Türkiye Haberleri
Microneedle rollers are already commercially available for cosmetic applications but their utility for clinical purposes in chronic wound treatment has not been explored to date tadalafil cialis from india dyskinesias and the marked swings in motor function on- off phenomenon
It might be an indication for extra doses but should not prevent someone from getting the vaccine molly and viagra
Added Zometa 09 mejor cialis o levitra 45 mg monobasic sodium phosphate monohydrate, 0
Instead, it found a decreased but statistically insignificant risk of breast cancer viagra blue pills
buy cialis online reviews 2013, cannot express these receptors
Arden urrEeyxoCDtk 6 19 2022 order cialis
5 mg cialis generic india Letrozole, also used under the trade name Famara Femara, is an oral medication that functions as an aromatase inhibitor
Hyperphosphatemia may contribute to this decrease in serum calcium by causing decrease in 1, 25 OH 2 vitamin D, skeletal resistance to parathyroid hormone, and exacerbation of calcium deposition propecia vs generic finasteride
We also thank Pierre Chambon, Daniel Metzger, Robert Clarke, Gilles Freiss, Richard H stromectol cream
Hearing Zhao Ling is words, Xue Ying suddenly froze, looked at is 151 over 90 high blood pressure Zhao Ling with interest, and said indifferently I did not expect that, you actually know the deity cheap cialis online Struthers AD Reid JL Whitesmith R Rodger JC
propecia medication Hackberry will also tolerate a lot of wind and pollution, making this a good choice for an urban or suburban wind and privacy screen
Real scientific, huh viagra lowers blood pressure
I ve always thought I started trying too soon how long until viagra kicks in coli JM109 cells
I suggest we be VERY deliberate about explaining each detail of our motivations for choosing each number nolvadex buy
Revised 2003 cialis on sale in usa
Quentin, USA 2022 06 27 20 50 50 topical propecia
From the corresponding tissue blocks, unstained tissue sections were sequentially cut within an estimated 100 to 200 Ојm of the original H E stained section priligy fda approval
However, we found that WNK1, pWNK1, and WNK4 are actually reduced Supplemental Figure 7, indicating that ROMK must be inhibited by a WNK independent pathway in CA SPAK mice priligy fda approval
levitra generique arnaque However, the use of estrogens as cardioprotective agents is limited by carcinogenic effects in women and feminizing effects in men
Type of Immunosensor Analyte Detected Method of Immobilization Redox Labeled Used Measurement Conditions Limit of Detection Linear Range Transduction Technique References Year Gold nanoparticle graphene based immunosensor Human IgG Covalent immobilization Ferrocene derivatives ferrocene monocarboxylic acid Fc 1, ОІ ferrocenyl propenoic acid Fc 2 and 1, 10 ferrocene dicarboxylic acid Fc 3 PBS, pH 7 buy cialis 5mg online
clomid alternative It is evident that PES use is a world wide phenomenon, with various effects on health, sports and domestic medicine markets
Thread Letro for gyno buy cialis online from india Coadministration of selexipag with rifampin, an inducer of CYP2C8, UGT1A3, and 2B7 enzymes, decreased exposure to selexipag s active metabolite by 50
Therefore, researchers looked for a molecule that could block this channel does propecia really work Direct and indirect costs of treatment will be recorded ovarian stimulation agents, luteal support medications, OPU, ET, physician fees, monitoring
2009 Dec; 23 6 793 800 levitra moins cher prix Long Term survival rate reduction in mice given a small
lasix ototoxicity Among the site s most popular drugs are Lipitor, to lower cholesterol; Celebrex, for arthritis pain relief; and tamoxifen, for breast cancer
Technically speaking of severe allergic to treat anthrax organism, 000 buy liquid cialis online Seek treatment if any of these symptoms occur nausea, vomiting, anorexia, fatigue, weakness, dizziness, and low blood pressure
I had really similar symptoms around that time, and now I m 4 or 5 days from when AF should come and I m spotting generic cialis for sale
6 Inhibitory effect of combined treatment with the aromatase inhibitor exemestane and tamoxifen on DMBA- induced mammary tumors in rats 36 hour cialis online
This drug is considered a pregnancy Category B drug doxycycline dosage chart
The period of elevated 53BP1 nuclear bodies coincided with slowed proliferation, and the return to baseline 53BP1 signals coincided with the return to accelerated proliferation in Fig 3A generic cialis online
Westin, MD, MPH GOG 0281, a really nicely designed trial, randomized patients with low grade serous cout levitra belgique
1, 2 If these anion channels release excitatory amino acids, microglia are ideally positioned to affect other CNS cells, because they form an essentially continuous network in the healthy CNS, with long processes abutting neurons and glial cells viagra boys welfare jazz When you make the appointment, ask if there s anything you need to do in advance, such as restrict your diet
2174 jurisdiction may not rest on the unilateral activity of another party or third person; World Wide Volkswagen, 444 U priligy dapoxetine 30mg If anything afflicts you do not say, If I had done such and such things, such and such would have happened
065 yen after shedding0 stromectol kopen kruidvat
buy levaquin 500mg sale levaquin 250mg generic
cialis 5 mg best price usa No previous neoadjuvant chemotherapy was permitted
A third component of the C4 demethylation complex, ERG27, is a sterone reductase SR whose product is a 4 desmethyl sterol levitra generico miglior prezzo india Note the presence of an outward current at positive potentials that is insensitive to Cs
At 16 DPO, not getting your period might mean you re pregnant priligy and cialis together
Simvastatin is a prodrug in which the 6 membered lactone ring of simvastatin is hydrolyzed in vivo to generate the beta, delta dihydroxy acid, an active metabolite structurally similar to HMG CoA hydroxymethylglutaryl CoA valtrex overnight delivery
Although the dragon and beauty knights, slave hunters and golden lion knights are divided into i get angry an hour after taking my blood pressure meds three distinct groups, after changing the uniform mercenary costumes, outsiders cannot see the contradictions inside how to get on accutane
Dear pregworld.org admin, Thanks for the valuable information!
https://drugsoverthecounter.com/# is viagra over the counter
Vancomycin therapy should not be recommended for patients with enterococcal isolates showing intermediate or high level vancomycin resistance accutane 20mg bestellen rezeptfrei
How is clozapine metabolized viagra and alcohol heart attack
In a prior study, 37 we observed that cancer related variables were not meaningfully related to general mental health in these women what is viagra for women
Pentachlorophenol 87 86 5 1991 walmart priligy As we age, our bodies metabolize medications differently, so it is important to check with your pharmacist to make sure that if you have been taking a prescription long term, that the dosage is still appropriate for your age and weight, if it has changed
One woman was excluded owing to unknown death cause buy cialis generic
Cabergoline is also used in combination with other medications to improve the effectiveness of those treatments tamoxifen and alcohol However, the time spent with the research assistant was relatively short when compared with the time spent with the specialists from the Family Cancer Clinic
In summary, our results demonstrate for the first time that P gp is functional in human alloantigen dependent T cell activation lasix online canada The data analyzed included educational attainment, age, gender, and race
online cialis The symptoms continue to become more serious if the SIADH is not treated
lasix generic Specifically, the fold change seen in all proteins was related to this associated network function
to link them covalently to carrier proteins whose role is to provoke favor the immune response in immunized animals, naturally not immunogenic is stromectol available in canada
The myosin heavy chain MHC cre transgene is active from midgestation and restricts expression of the cre recombinase to cardiomyocytes 17 priligy generic
Epub 2022 Jul 7 priligy tablets
Zofran ondansetron is generally well tolerated, but is rarely associated with QT prolongation a type of arrhythmia how long does lasix last If you want to enter inside, you must break the Qi of Dan Dao in this Dan Dao Valley
order arimidex 1mg generic anastrozole 1 mg cost cheap arimidex 1mg
finasteride vs propecia Assessment and discussion about risk reducing medications can occur during the well woman preventive care visit, Nelson told Medscape Medical News
Scappaticci FA, Fehrenbacher L, Cartwright T, Hainsworth JD, Heim W, Berlin J, et al clomid in males side effects
Patients should be monitored following infusion therapy clomiphene citrate over the counter
I discovered your blog site on google and check a few of your early posts. Continue to keep up the very good operate. I just additional up your RSS feed to my MSN News Reader. Seeking forward to reading more from you later on!…
It is much less common in the United States than in developing countries, but it should be considered in the differential diagnosis of limb ischemia and infection viagra before and after photos
In this article, we will review the epidemiology and managementof osteoporotic pelvic bone fracture, specifically from a United Kingdom perspective fincar finasteride online canada
Pour être autorisés en France, ces jeux doivent être agréés par L’ANJ (autorité nationale de jeux), une autorité administrative indépendante (AAI). Si l’on joue à un jeu illégal, il faut savoir que l’on ne risque pas de sanctions pénales, mais que les conséquences peuvent être plus dramatiques, car la triche est fréquente, les gains sont rarement payés, les mineurs ne sont pas protégés, les données personnelles des joueurs ne sont pas protégées et que le joueur ne dispose d’aucune protection légale en cas de litige. Le Royaume-Uni est toujours dans la course, ou déposez avec les codes de promo ELVIS pour obtenir des offres attractives pour jouer à vos jeux de table préférés au Casino Titan. Il y a deux côtés à l’action ici, l’accord a le potentiel de leur donner une présence mondiale extrêmement forte.
https://saskkartclub.com/community/profile/demilawton19846/
Que vous soyez détenteur d’un PC ou d’un Smartphone, aucun téléchargement n’est requis pour jouer à un quelconque casino en ligne. C’est dire que vous pouvez jouer de manière instantanée à vos titres de casino préférés. Tout simplement, il suffit d’avoir une connexion internet et de s’inscrire sur une plateforme de jeux afin de jouer avec des fonds réels. Toutefois, vous pouvez donc essayer les casinos de jeux en ligne sans téléchargement suivants : Play Regal, Unique casino et Kings Chance. Wild Sultan est en quelque sorte le palace du Moyen-Orient du divertissement. Créé autour du thème des maharajas et de l’opulence, vous allez pouvoir accéder sur la plateforme à plus de 1 000 machines à sous, une multitude de jeux de table, des jeux de loterie et de grattage, du vidéo poker ainsi que des jeux live très interactifs. Les atouts majeurs du casino sont indéniablement à notre avis, les bonus généreux offerts aux joueurs à chaque étape de leur parcours sur le site de l’opérateur. Disposant d’une licence provenant de Curaçao Gaming Authority, le casino est tout à fait fiable et sécurisé.
These drugs are used to treat heart failure or hepatic, renal, or pulmonary disease when sodium and water retention results in edema or ascites finasteride 5mg no prescription cheap
Nos primeiros 20 segundos de jogo, os jogadores de Corinthians e Atlético-MG fizeram um protesto referente à regulamentação que mexe no direito trabalhista dos atletas: a Lei Geral do Esporte. Esta não foi a primeira vez que o protesto foi realizado. No duelo contra o Flamengo, na Neo Química Arena, por exemplo, o ato de tapar a boca também foi realizado. Г‰ a interpretação da notГcia, levando em consideração informações que vГЈo alГ©m dos fatos narrados. Faz uso de dados, traz desdobramentos e projeções de cenГЎrio, assim como contextos passados. O AtlГ©tico comeГ§ou melhor o primeiro tempo ao pressionar o Sport por toda a etapa em campo. A primeira boa chance saiu com Diego Costa, sem sucesso nos primeiros minutos. O time pernambucano respondeu aos 15 minutos com Hernanes, enquanto parou em defesa de Everson.
https://jogos-em-tempo-real-1.werite.net/post/2022/12/07/dazn-futebol-ao-vivo2
A 32ª rodada da Série A do Campeonato Brasileiro 2021, o Brasileirão, tem quatro jogos marcados para hoje, domingo, 14 de novembro (14/11). Confira como está a classificação atualizada – veja abaixo ou clique aqui para conferir. Abordagem sobre determinado assunto, em que o tema Г© apresentado em formato de perguntas e respostas. Outra forma de publicar a entrevista Г© por meio de tГіpicos, com a resposta do entrevistado reproduzida entre aspas. O Campeonato Paulista de Futebol, chamado também de Paulistão, é um torneio que ocorre desde 1902. A Federação Paulista de Futebol, inclusive, é a mais antiga do Brasil. O último time a levar o título foi o São Paulo, com o Palmeiras na segunda colocação.
It s possible for Valtrex to pass from mothers to infants via breast milk, and there is no data on the effects of this best cialis online Stewart FH, Kaunitz AM, Laguardia KD, Karvois DL, Fisher AC, Friedman AJ
In PCOS, LH is secreted at a rapid pulse rate buying cialis online
Several studies have documented the expression of estrogen receptors in different invertebrates Keay and Thornton 2009; Jones et al azithromycin urinary infection
cialis tablets for sale Intracellular GSH levels were decreased in response to transsulfuration inhibition in all cell types, but only Ets 1 overexpressing cells displayed decreased GSH levels following inhibition of Sx c Figure 4B
Цивилизация способна превратить животное
в объект страха. Тогда у ребенка может возникнуть
связанная с животным миром фобия.
Ребенок обычно воспринимает всех
существ вместе, поэтому навязанная боязнь того или иного животного способна
обернуться боязнью общества
в целом. 5 способов вернуть
интерес к работе и увлечениям
You said it nicely.!
fanduel online casino vegas world free online casino games harrah’s online casino
Kudos! I like it!
pay for your essay buy essay papers
You actually stated it wonderfully.
what should i write my persuasive essay on who can write my essay for free writes your essay for you
Many thanks, A good amount of information!
essay writer online cheap essay writer reviews how to write an about me for website
This type of data sharing may be considered a “sale” of information under California privacy laws. Turning off personalized advertising opts you out of these “sales.” Learn more in our Privacy Policy., Help Center, and Cookies & Similar Technologies Policy. $148.00 $128.00 Some reviewers report thin fabricAvailable in 26 colors and prints, this sleeveless dress is just what you need for a simple night out look. It has a comfortable and loose fit, a round neck, and stretchy fabric. “I really love this dress. It’s flattering and comfortable. I will definitely buy more in different colors!” wrote one satisfied customer. There’s nothing quite like slipping into full-length, absolutely-to-die-for formal attire. A dress with elegance and esteem that makes you feel sexy and sensual: the one that makes you the It-Girl of the evening. The right gown will elevate a closet to new heights. We recommend timeless dark colors with delicate details.
https://www.metal-archives.com/users/y4ltcnp352
We reserve the right to cancel any order which is logistically too complicated to deliver. We will treat this order as a cancelled order, and a refund will be issued if any monies have been paid. Cloudflare for Infrastructure is a complete solution to enable this for anything connected to the Internet. 9. Any person taking advantage of this promotion does so, on complete acceptance of the terms and conditions. Claims that do not comply with the terms and conditions will be disqualified and treated as invalid/rejected. A refreshing update on your professional wardrobe may be in order if you still haven’t included ankle pants in the repertoire. This version features an ankle-length crop, a sleek mid-rise, slit hip pockets, and a zipper with tab closure. Neutral colors like beige, black, white, and even pink tops may bring balance to the vivid pink color at the bottom, but it wouldn’t hurt to be adventurous by color-clashing it with bright green, blue, or yellow all for the limelight.
Ans. Wash your face first and let it dry completely. It’s always recommended that you should use LED products on a clean face without applying any serum or moisturizer so that the light therapy can effectively work on your skin without any barrier. After that, place the LED mask on the face. You can increase its usage speed from 10 to 30 minutes. This site uses Akismet to reduce spam. Learn how your comment data is processed. RECENT ARTICLES RECENT ARTICLES Many of us have experienced the strange phenomenon of freshly washed hair feeling waxy. It’s not only unappealing but can also weigh down your blowout. There are a few different causes for this, but luckily, each one comes with a pretty easy fix. Note: This post contains affiliate links which means if you click on a link and purchase an item, we will receive an affiliate commission at no extra cost to you.
https://troyuusp306307.blog-kids.com/18134029/loreal-magnetic-black-mascara
Here are the highest rated MAC Colour Excess Gel Pencil Eye Liner shades: } We love how Pacifica Beauty’s affordable and long-lasting eyeliners make our eyes pop! ⚡ These colored pencils are cruelty-free and vegan, thanks to the unique plant-based pigments. And because it’s a wooden pencil, you don’t have to worry about extra plastic. Glide over your water line or the entire lid for dramatic results. Impressive that it stays on so well all dat, all evening. Great color Love the new white eyeliner really draws on my water line and gives me that awake look AMC Eyeliner Gel unlimited 3D gel pencil is a smudge-proof and rub-proof gel eyeliner with an easy-to-control 1.5mm p … read more Find an eyeliner for every eye look, from classic cat eyes to graphic lids and more
Some of the leading Maryland online betting sites will also host online casinos. Indeed, many of today’s leading sports betting brands began life as online casinos that diversified to offer sports betting sites too. As a result, casino games may be easily accessible from the operator in question – and you may find Maryland promo codes that include free spins on casino games as well as a sports betting bonus. If you are a fan of casino games as well as sports betting bonuses, this is ideal for you. If you ever bet offshore, you may have felt a little deceived when you tried to withdraw money after receiving a sign-up bonus, only to find out you need to to hit a rollover requirement. We covered rollovers in-depth here. In order to be eligible for a payout after taking a bonus, a customer must comply with the play through attached to said bonus/promotion/clients benefits & rewards or contest.
https://stephenkljg054101.shotblogs.com/francis-ngannou-stipe-odds-31294820
There are some great free bets available for new players in a very competitive part of the sports betting industry. There are many types to look at and something for everyone, from matched deposits to risk-free bets and free bets no deposit offers. Welcome free bets are a great way to pull in new customers. If a gambler places a free $20 bet for example, then this will be matched by the bookmaker. Intertops are renowned for offering free bets, and customers have to insert the bonus code ROOKIEFREEBET upon signing up in order to make the most of it. Free bets are a bonus offer from online sports betting sites that allow users to place risk-free wagers. However, it is important to note that just because it is called a “risk-free wager”, this free bet doesn’t guarantee a win.
We are the best absolutely free dating in USA and friendship website to meet local USA women and men across the world. We are first dating website catering specifically to USA singles. We bring american singles together to encourage USA dating because we believe that it is important to bring like-minded American singles together in an environment where they can feel comfortable. Hinge calls itself “the dating app designed to be deleted” — not to hide your dating life, but because it gets you out on promising dates so you’re less likely to need the app for the long haul. A free membership comes with filters for gender, location, age, distance, ethnicity and religion. Preferred memberships add additional filters, unlimited likes and the ability to see everyone who likes you at one time.
http://aspirepm.co.uk/?p=207726
When it comes to falling in love later in life, single seniors can often find it in a nursing home or assisted living center. With plenty of new social activities, group classes and wellness programs at assisted living centers, the chances of finding a special someone are greater than ever. Take this couple, for example, who discovered love eight decades into their lives at a nursing home in Texas. Whereas most other serious relationship dating sites like Match and eharmony are for all ages, this dating platform is designed especially for those over 50 and above who are looking for love. It’s easy to use and will match you up with people based on your compatibility as well, rather than your general life interests, appearance, or other factors. Meet Seniors in TODAY and connect with hundreds of thousands of singles just like you immediately! (As a Silicon Valley firm, we have been in the online dating business for over 20 years!)
I needed to thank you for this good read!! I certainly loved every little bit of it. I’ve got you book-marked to look at new things you post…
Рассмотрим, как провести стрелку для дневного макияжа. Обычно для этих целей используется карандаш. Линия проводится по верхнему веку, двигаться нужно строго над ресницами от внутреннего до внешнего уголка. После нужно аккуратно пройтись карандашом между ресничками. Хвостик стрелки нужно сделать пологим и недлинным. Теперь нужно слегка растушевать карандашную линию. Как нарисовать стрелки на глазах подводкой поэтапно: Контур «colorblock». На верхнее веко наносится контур жидкой подводкой или косметическим маркером чёрного цвета. Стрелка должна быть широкой. По верхнему краю стрелки проводится декоративная линия яркого цвета. Современные прелестницы не отстают от моды, находятся в постоянном поиске средств для покорения мужских сердец. Контура глаз меняется с новыми тенденциями в моде, совершенствуется, изменяется. Юных красавиц интересует вопрос: как нарисовать красивые стрелки? Существует ряд правил, выполнение которых обеспечивает красивый макияж глаз.
http://lx22gp.kr/server/bbs/board.php?bo_table=free&wr_id=192259
Тушь из Японии позволит Вам выглядеть ярко и привлекательно в любую погоду – влагостойкие компоненты защитят Ваши реснички от дождя, снега, морских капель и даже слез. У Вас отключены куки, пожалуйста включите их для комфортной работы с этим сайтом На пляже, пенной вечеринке, в бассейне, на тренировке, под летним дождем или на собственной свадьбе — не думайте о макияже, забудьте о туши, будьте уверены в себе на 100%! Благодаря удобной щеточке тушь максимально комфортно и просто наносится по всей длине ресниц, без комочков и эффекта слипшихся ресниц. Operated by Eastwest Commercial Pte. Ltd. Relouis Тушь для ресниц GOLD Объемная Извлекайте тушь из флакона выкручивающим движением, после её использования вставьте щеточку – аппликатор так же вкручивающим движением. Это поможет выгнать воздух из флакона, который обычно сушит ее. В корзине Корзина пуста +7 (495) 510-89-94 Здесь классно все: флакон архитектурной формы, щеточка, которая разделяет реснички и качественно прокрашивает каждую, а также формула для объема и повышенной пушистости. Особенно оценят эту тушь те, у кого от природы ресницы тонкие и незаметные.
com 20 E2 AD 90 20Viagra 20Pirkti 20 20Pregabalin 20And 20Viagra pregabalin and viagra A spokeswoman for San Francisco District Attorney GeorgeGascon confirmed on Wednesday that surveillance footage of theincident last month showed a train car full of passengers withinfeet of the accused gunman as he openly brandished a weapon onthe train best price for generic cialis Water soluble dietary fibers and cardiovascular disease
A spokesperson for the manufacturer of this type of multi-player video poker tables says the machines can deal 50 per cent faster than human dealers, allowing customers to spend their money faster. For more information on our Return policy, please click here! According to Vito Casucci, a spokesman for Pokertek, the machines can deal 50 per cent faster than human dealers, allowing customers to spend their money faster. The union is concerned that casino staff may consequently lose their jobs and that the new poker rooms represent a trend toward more electronic games. The next generation Jackpot Blitz® includes Ticket-In-Ticket-Out (“TITO”) functionality, allowing casino guests to use cash directly at the table to fund play. In addition, the new Jackpot Blitz® supports the Slot Accounting System (“SAS”) protocol, allowing seamless integration with most casino management systems. The two new features are required by most regulated casinos and represent the last major step in mass market development for the Jackpot Blitz®. The new Jackpot Blitz® can be seen in the video below:
http://www.hieo.co.kr/bbs/board.php?bo_table=free&wr_id=328254
Michigan is the latest state to welcome PokerStars Casino. The site launched in the state in early February 2021. Players create just one account to gain access to the casino, online poker and sports betting via FOX Bet. PokerStars teamed up with the Little Traverse Bay Bands of Odawa Indians Gaming Authority to be able to launch. How to get PokerStars Casino new player bonus? It is not required to enter a code during your registration, simply click the link and get started. You can choose between an up to $600 in match bonus or a PokerStars freeplay bonus of $100. PokerStars is the largest, and most recognizable online poker brand in the world. Already with a large network of international players, PokerStars now serves select US customers. PokerStars currently operates in three US states: New Jersey, Pennsylvania, and Michigan. As of 2023, Michigan and New Jersey poker players can now play each other increasing the player pool for poker tables.
2019 Feb; 26 5 4288 4299 best generic cialis In the period after 2000s on the other hand, in an effort to evaluate low dose rate radiation effects, many animal studies were focused on chronic external beam radiation
отель либерти флай адлер официальный сайт
славянка приморский край гостиницы
санаторий балтийский берег санкт петербург официальный сайт
гостиницы г сыктывкар
геленджик реабилитационный центр
аквалоо стоимость проживания
ток судак видео
хостел абакан дешево
хостел в воронеже цены за сутки
гостиницы искитим
отель анапский бриз
искра пятигорск официальный сайт
солнечногорск санатории и пансионаты
когда лучше ехать в кисловодск
валдай хостел
санатории на берегу финского залива ленинградской области
новокузнецк гостиницы в центре
санаторий днепр гаспра
гостиница балабаново
ramada by wyndham yekaterinburg hotel spa
алатырь официальный
санатории сочи черноморье
санаторий родник пятигорск цены
военный санаторий лазурный берег
отель манчестер
курорты в крыму список
замок горного короля аршан официальный
микунь гостиницы
мини отель дукат анапа
гостиница бештау в пятигорске телефон
хостел 1723 пермь
отель где все включено
отели в кабардинке с бассейном
отдых в крыму цена
санатории ессентуки с лечением желудочно кишечного тракта
санаторий острова сочи
PUBMED Abstract Fortmann SP, Burda BU, Senger CA, et al propecia costco
Would love to hear your stories on Clomid and hear how long before you got your BFP on Clomid propecia 5 mg for sale no If anyone else knew about it, he would never sell spiritual liquid here, maybe he would have been killed long ago, and then Take treasure
купить медицинскую справку
купить справку
Excellent article. I certainly love this website. Keep it up!
I do accept as true with all the concepts you have presented in your post. They are very convincing and will definitely work. Still, the posts are too brief for novices. May you please extend them a bit from next time? Thank you for the post.
What’s up, this weekend is pleasant in favor of me, since this time i am reading this impressive informative article here at my home.
I will right away take hold of your rss as I can not in finding your email subscription link or newsletter service. Do you have any? Please allow me understand so that I may just subscribe. Thanks.
This is my first time go to see at here and i am really happy to read all at one place.
Great beat ! I wish to apprentice whilst you amend your web site, how can i subscribe for a blog web site? The account aided me a appropriate deal. I have been tiny bit familiar of this your broadcast provided bright transparent concept
I believe what you postedwrotesaidthink what you postedwrotethink what you postedwrotesaidbelieve what you postedwrotesaidWhat you postedtyped was very logicala bunch of sense. But, what about this?think about this, what if you were to write a killer headlinetitle?content?typed a catchier title? I ain’t saying your content isn’t good.ain’t saying your content isn’t gooddon’t want to tell you how to run your blog, but what if you added a titlesomethingheadlinetitle that grabbed people’s attention?maybe get people’s attention?want more? I mean %BLOG_TITLE% is a little plain. You could peek at Yahoo’s home page and watch how they createwrite post headlines to get viewers interested. You might add a related video or a related pic or two to get readers interested about what you’ve written. Just my opinion, it might bring your postsblog a little livelier.
Saved as a favorite, I really like your site!
I’m impressed, I must say. Rarely do I encounter a blog that’s equally educative and engaging, and let me tell you, you have hit the nail on the head. The issue is something which not enough people are speaking intelligently about. I am very happy that I found this in my search for something relating to this.
Excellent post. I was checking continuously this blog and I am impressed! Very useful information specially the last part 🙂 I care for such info a lot. I was seeking this particular info for a long time. Thank you and good luck.
Please let me know if you’re looking for a article author for your site. You have some really great posts and I believe I would be a good asset. If you ever want to take some of the load off, I’d absolutely love to write some material for your blog in exchange for a link back to mine. Please send me an e-mail if interested. Thank you!
Hola! I’ve been following your website for a while now and finally got the bravery to go ahead and give you a shout out from New Caney Tx! Just wanted to mention keep up the excellent job!
Wow, awesome blog layout! How long have you been blogging for? you make blogging glance easy. The total glance of your site is wonderful, let alonesmartly as the content!
Neat blog! Is your theme custom made or did you download it from somewhere? A design like yours with a few simple adjustements would really make my blog shine. Please let me know where you got your design. Cheers
Awesome site you have here but I was curious about if you knew of any user discussion forums that cover the same topics talked about in this article? I’d really love to be a part of group where I can get feed-back from other knowledgeable individuals that share the same interest. If you have any recommendations, please let me know. Thanks a lot!
Thank you for another informative blog. Where else may I am getting that kind of info written in such a perfect way? I have a challenge that I am simply now operating on, and I have been at the glance out for such information.
I don’t know if it’s just me or if everyone else experiencing problems with your blog. It seems like some of the text within your posts are running off the screen. Can someone else please comment and let me know if this is happening to them too? This could be a problem with my browser because I’ve had this happen before. Kudos
El casino online de Betfair es donde está toda la acción. Es considerado por muchos como el mejor casino online y el más avanzado gracias a la gran cantidad de juegos de casino clásicos y modernos que ofrece. Como ya sabes, hay muchas variantes de la ruleta, así que no debería sorprenderte que te digamos que hay más de 100 tipos de juegos de ruleta que se pueden encontrar online. Obviamente, eso es demasiado para mencionarlos todos, pero aquí están nuestros juegos de ruleta más recomendados para jugar en los casinos online: La Mina de Oro Plus Si buscas un juego online cargado de acción y variedad, la ruleta es una excelente opción. Para ganar dinero jugando a la ruleta, es necesario apostar dinero real, lo que conlleva el riesgo de perderlo. Ahora bien, puedes jugar a la ruleta online en modo demo y disfrutar de toda la emoción sin arriesgar tu dinero.
https://meet-wiki.win/index.php?title=Bono_de_casino_norsk_España
Observamos con frecuencia que los apostadores, entonces es hora de probar el juego de tragamonedas en línea Hot Twenty gratuito. Los símbolos de bajo pago se componen de palos de naipes, Lannister. Elija el sitio para apostar en Virginia Occidental que le permitirá jugar todos sus juegos favoritos, consulte nuestra revisión completa de 10bet y por qué la calificamos con 4 de 5 estrellas. Juegos gratis de giros para jugar en segundo lugar, la reposición de la cuenta sin conversión le permite ahorrar en la comisión del sistema de pago. Ciertos casinos ofrecen bonos de no depósito, que permiten a sus jugadores que apuestan por primera vez en la plataforma beneficiarse del regalo de un saldo gratis para jugar online, sin necesidad de depositar una cantidad de dinero previa en el casino. El objetivo de estos regalos es incentivar el juego e invitar a los nuevos usuarios a probar las funcionalidades del sitio web.
курорты тюмени и тюменской области цены
шишка отель
отель романов евпатория официальный сайт
массаж со скидкой
Hey terrific blog! Does running a blog similar to this take a massive amount work? I have no expertise in computer programming but I was hoping to start my own blog soon. Anyways, if you have any suggestions or tips for new blog owners please share. I know this is off topic but I just needed to ask. Cheers!
I like the valuable information you supply in your articles. I will bookmark your weblog and test again here frequently. I am slightly certain I will be informed many new stuff right here! Good luck for the following!
санаторий сеченова ессентуки отзывы
alex resort spa hotel 4 гагра
санаторий крутушка казань
пальмира ялта
For most recent news you have to visit world-wide-web and on world-wide-web I found this web site as a most excellent site for latest updates.
Excellent write-up. I definitely love this website. Keep it up!
Yes! Finally something about %keyword1%.
крым судак отдых 2021
санаторий дубрава официальный сайт
гостиница советская коломна цены
автобус увильды челябинск расписание
Its like you read my mind! You seem to know so much approximately this, like you wrote the ebook in it or something. I think that you could do with some p.c. to force the message house a bit, however other than that, this is magnificent blog. An excellent read. I’ll definitely be back.
Great article! This is the type of information that are meant to be shared around the internet. Disgrace on the seek engines for now not positioning this publish upper! Come on over and discuss with my web site . Thank you =)
Hi mates, its great article regarding educationand completely explained, keep it up all the time.
Good day! I know this is somewhat off topic but I was wondering which blog platform are you using for this site? I’m getting fed up of WordPress because I’ve had issues with hackers and I’m looking at options for another platform. I would be awesome if you could point me in the direction of a good platform.
Greate pieces. Keep writing such kind of information on your page. Im really impressed by your site.
It is appropriate time to make some plans for the future and it is time to be happy. I have read this post and if I could I wish to suggest you few interesting things or suggestions. Perhaps you could write next articles referring to this article. I want to read more things about it!
пермь советской армии 60
база отдыха снегурия в приозерске
хостел европейский
купить путевку в ессентуки в санаторий
Nice post. I learn something new and challenging on sites I stumbleupon everyday. It will always be exciting to read content from other writers and practice a little something from their websites.
Fantastic website you have here but I was wanting to know if you knew of any community forums that cover the same topics talked about in this article? I’d really love to be a part of online community where I can get opinions from other knowledgeable individuals that share the same interest. If you have any recommendations, please let me know. Kudos!
Da una parte capiamo anche noi che ormai per ogni servizio online è sempre necessario creare un profilo e ci si ritrova poi con decine di dati e password da ricordare… dall’altra la registrazione nei casinò sembra più lunga rispetto a quella di altri siti, ma questo avviene perchè le grandi somme di denaro e i grossi premi che si possono vincere, necessitano di maggiori controlli, ergo più dati da fornire. Il mercato delle slot si è fatto sempre più competitivo, ma è online che possiamo trovare davvero una scelta vastissima: stando comodamente seduti sul divano abbiamo infatti accesso a centinaia di varianti di slot machine. I siti slot online con soldi veri, oltre ad offrire la possibilità di provare in versione demo i giochi di slot, consentono anche di usufruire di bonus e giri gratis per macchinette a rullo, cosa che negli apparecchi fisici non avviene, e hanno limiti di puntata molto più elastici che partono da pochi centesimi.
http://ysneulbom.com/bbs/board.php?bo_table=free&wr_id=39331
A questo, l’affiliazione 888 ha aggiunto una sezione live che comprende tavoli di roulette, blackjack, baccarat e poker oltre a numerose varianti degli stessi. L’utente può quindi trovare il gioco che preferisce e divertirsi come se fosse realmente su un tavolo verde. L’interfaccia user friendly permette inoltre anche ai principianti di capire immediatamente le dinamiche di gioco. Un Codice Sconto 888 Poker (chiamato anche codice promozionale, buono sconto, coupon sconto) è una sequenza di numeri e lettere che i negozi online in Italia, Europa, Cina e Stati Uniti usano per offrire ai propri clienti sconti immediati per l’acquisto di prodotti online. Per esempio, nel caso 888 Poker volesse spingere un prodotto particolare, creerebbe un Codice Sconto 888 Poker del 125% su quel prodotto per far si che esso sia comprato maggiormente rispetto ad altri. In questo caso il Codice Sconto, Coupon, Buono Sconto o Codice Promo servirebbe per incrementare la vendita del prodotto stesso.
This is the right web site for anyone who would like to find out about this topic. You understand so much its almost hard to argue with you (not that I personally would want toHaHa). You definitely put a brand new spin on a topic that’s been written about for decades. Great stuff, just excellent!
There is definately a lot to learn about this subject. I love all the points you’ve made.
I am extremely impressed with your writing skills and also with the layout on your blog. Is this a paid theme or did you customize it yourself? Either way keep up the nice quality writing, it’s rare to see a nice blog like this one these days.
I really like what you guys are up too. This sort of clever work and coverage! Keep up the superb works guys I’ve you guys to blogroll.
I like the valuable information you supply in your articles. I will bookmark your weblog and test again here frequently. I am rather certain I will be told a lot of new stuff right here! Good luck for the following!
Its like you read my mind! You seem to know so much about this, like you wrote the book in it or something. I think that you could do with some pics to drive the message home a bit, but other than that, this is great blog. An excellent read. I’ll definitely be back.
It’s very straightforward to find out any topic on net as compared to books, as I found this article at this website.
жилье в абхазии
хостел сетунь парк нежинская ул 9 москва
отель визави
геленджик санаторий
Thanks for one’s marvelous posting! I actually enjoyed reading it, you are a great author. I will be sure to bookmark your blog and will often come back very soon. I want to encourage you to ultimately continue your great posts, have a nice day!
Useful info. Fortunate me I found your web site accidentally, and I am stunned why this coincidence did not came about in advance! I bookmarked it.
You can definitely see your expertise in the article you write. The world hopes for more passionate writers like you who aren’t afraid to mention how they believe. Always go after your heart.
санаторий ташир лазаревское
отель порто маре в крыму
санаторий знание камеры
путевки в гурзуф
I think the admin of this website is in fact working hard for his site, as here every stuff is quality based stuff.
It’s hard to find well-informed people about this topic, but you sound like you know what you’re talking about! Thanks
Hey, I think your website might be having browser compatibility issues. When I look at your blog site in Chrome, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, superb blog!
The best online gambling sites secure their platforms using SSL encryption. To know if an online casino is secure, check the website protocol type on your web browser address bar. If it is HTTPS, the betting site is safe. However, if it’s HTTP, any data you provide can be intercepted. Here’s a look at the current situation regarding casinos in Georgia, including online casinos. Read on as well for information about past efforts to legalize casinos in the state and a discussion of when and where casinos could ultimately come to the Peach State. Diverse Game Library: Ignition takes pride in its vast game library, which distinguishes it from other online real money casinos. With over 250 games from more than 10 acclaimed developers, players can enjoy a wide array of high-quality titles. The selection includes popular casino games, such as premium slots, exclusive poker offerings, and much more.
https://frontierssaga.com/community/profile/5442cclviii4845/
All debts are enforceable in Law on the Isle of Man. GG International Limited strictly prohibits access and services to those under the legal age of Eighteen (18). Customers should check the laws and regulations in their own country and comply with them. Information on this website is subject to change without notice. GGPoker | © 2018 – 2023 The royalties that you will see awarded in OFC Pineapple Poker are extra units that you are rewarded with for making valuable hands. If you have played Chinese Poker, then you will probably notice that the royalties used in Pineapple Poker are more generous, since it is a little bit harder to make a strong hand in this game. A player in Fantasy Land is dealt all 13 cards up front. They place their cards face down so non-Fantasy Land players can’t see them. Then they wait until hands not in Fantasy Land are played as usual, one card at a time. Once normal play is complete, players in Fantasy Land arrange their cards into the usual three rows of hands. Being able to see other player row hands is obviously a huge advantage.
Undeniably believe that that you stated. Your favourite justification appeared to be at the internet the simplest thing to have in mind of. I say to you, I definitely get irked at the same time as other folks consider concerns that they plainly do not realize about. You controlled to hit the nail upon the top as smartly as defined out the whole thing with no need side effect , folks can take a signal. Will likely be back to get more. Thank you
гостиница пионер урай
казантель отель
фандорин отзывы
гостиница на цветном бульваре москва
I’m really enjoying the design and layout of your blog. It’s a very easy on the eyes which makes it much more enjoyable for me to come here and visit more often. Did you hire out a designer to create your theme? Outstanding work!
This is a very good tip especially to those new to the blogosphere. Brief but very accurate information Thanks for sharing this one. A must read article!
Wow, wonderful blog layout! How long have you been blogging for? you make blogging look easy. The overall look of your web site is wonderful, let alone the content!
Howdy very nice website!! Guy .. Beautiful .. Amazing .. I will bookmark your web site and take the feeds also? I am glad to find numerous useful information here in the post, we’d like develop more strategies in this regard, thank you for sharing. . . . . .
Howdy, i read your blog occasionally and i own a similar one and i was just wondering if you get a lot of spam comments? If so how do you prevent it, any plugin or anything you can advise? I get so much lately it’s driving me insane so any help is very much appreciated.
Pretty component to content. I simply stumbled upon your web site and in accession capital to say that I acquire in fact enjoyed account your blog posts. Any way I’ll be subscribing in your augment or even I fulfillment you get right of entry to consistently rapidly.
Hey there, You have performed an excellent job. I will definitely digg it and in my opinion recommend to my friends. I am sure they will be benefited from this web site.
A person necessarily lend a hand to make critically articles I would state. This is the first time I frequented your web page and thus far? I amazed with the research you made to create this actual publish amazing. Wonderful task!
отдых пицунда
отдых в казани на выходных
белые скалы абхазия официальный сайт
степная 27 балаково
Nice replies in return of this difficulty with firm arguments and describing everything concerning that.
Hey there! I’ve been following your web site for a while now and finally got the bravery to go ahead and give you a shout out from Houston Tx! Just wanted to mention keep up the great job!
Hi to all, how is all, I think every one is getting more from this web site, and your views are nice for new users.
Hi! Quick question that’s completely off topic. Do you know how to make your site mobile friendly? My site looks weird when viewing from my iphone. I’m trying to find a theme or plugin that might be able to correct this problem. If you have any suggestions, please share. Appreciate it!
отель южная ночь алушта
грейс кристалл адлер
гостиницы наро фоминск адреса цены
эко кемпинг сфера переславль
I enjoy, lead to I found exactly what I used to be taking a look for. You have ended my 4 day long hunt! God Bless you man. Have a nice day. Bye
This is a good tip especially to those new to the blogosphere. Brief but very accurate information Thanks for sharing this one. A must read article!
Great article! This is the type of information that are supposed to be shared around the internet. Disgrace on the seek engines for not positioning this post upper! Come on over and visit my site . Thank you =)
I love your blog.. very nice colors & theme. Did you create this website yourself or did you hire someone to do it for you? Plz answer back as I’m looking to create my own blog and would like to know where u got this from. cheers
Magnificent beat ! I wish to apprentice while you amend your site, how can i subscribe for a blog site? The account aided me a acceptable deal. I had been tiny bit acquainted of this your broadcast provided bright clear concept
You’ve made some decent points there. I looked on the web to learn more about the issue and found most individuals will go along with your views on this site.
This is my first time pay a visit at here and i am really happy to read all at alone place.
Ahaa, its good discussion about this post here at this webpage, I have read all that, so now me also commenting here.
When someone writes an article he/she maintains the thought of a user in his/her mind that how a user can know it. Thus that’s why this article is great. Thanks!
I got this site from my pal who told me about this website and now this time I am visiting this website and reading very informative articles or reviews here.
Wow, this article is pleasant, my sister is analyzing these things, thus I am going to let know her.
The Golden Record on Voyagers 1 and 2 If you are participating in our Colour Play workshop as part of an in-store local yarn store event, you will have access to 36 colours of our SweetGeorgia Tough Love Sock to play with during your workshop. If you are playing along with us from home, you can definitely use your own stash yarns, leftover bits of yarn from other projects, fat quarters or other coloured fabrics, or even sample paint chips. You can check out our mini skeins currently available in our online shop at sweetgeorgiayarns product-category yarn mini-skein-sets The Golden Record on Voyagers 1 and 2 This way we learn about your interests and can ensure that we provide you with the information and promotions that are of most interest to you. We may also ask you for your opinion about our products and services. If you don\u2019t want to receive any more messages or if you want to opt-out of a particular form of communication with us (for example SMS, E-mail or regular mail), just, follow the steps in that particular communication.
https://themalachiteforest.com/community/profile/7679dlxxxviii57/
The multimillionaire Cue will take players a long time to earn, depending on the pool halls they play. Ultimately, 8-Ball Pool is based on how much cash players are willing to put in, with higher stake-in games yielding higher profit. Your goal is to sink all the striped or solid balls, and finally the 8 ball. You’re assigned stripes or solids based on the first ball sunk (after the opening shot). But watch out, if you sink the 8 ball too early, you lose the game! 8 Ball Pool encourages realistic simulated gambling behaviours. Saturated gambling content, including: Anyone can become a pro player without any actual experience in 8 Ball Pool. But, not anyone could get decked out in custom avatars and lavish looking pool cues. Pretty much everything in this game forces a microtransaction on you. Players can buy their way to the coolest cosmetics without having to grind and win thousands of games.
I am really thankful to the owner of this website who has shared this great article at at this place.
If you want to take much from this post then you have to apply such strategies to your won webpage.
I know this if off topic but I’m looking into starting my own blog and was wondering what all is required to get set up? I’m assuming having a blog like yours would cost a pretty penny? I’m not very internet savvy so I’m not 100% sure. Any tips or advice would be greatly appreciated. Kudos
My relatives all the time say that I am wasting my time here at net, except I know I am getting knowledge daily by reading such good articles or reviews.
Useful info. Fortunate me I found your site by chance, and I am stunned why this coincidence did not came about in advance! I bookmarked it.
Good day! Would you mind if I share your blog with my zynga group? There’s a lot of people that I think would really enjoy your content. Please let me know. Cheers
Nice post. I learn something new and challenging on sites I stumbleupon everyday. It will always be interesting to read content from other writers and practice a little something from their sites.
This post will help the internet users for building up new blog or even a blog from start to end.
Very soon this web site will be famous among all blogging users, due to it’s good articles
Have you ever thought about creating an e-book or guest authoring on other websites? I have a blog based upon on the same subjects you discuss and would really like to have you share some stories/information. I know my audience would value your work. If you are even remotely interested, feel free to send me an e-mail.
I think the admin of this web site is actually working hard in favor of his web site, since here every stuff is quality based data.
Hey there! Someone in my Myspace group shared this site with us so I came to look it over. I’m definitely enjoying the information. I’m book-marking and will be tweeting this to my followers! Outstanding blog and excellent design and style.
I was wondering if you ever considered changing the layout of your blog? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having one or two images. Maybe you could space it out better?
Im not that much of a online reader to be honest but your blogs really nice, keep it up! I’ll go ahead and bookmark your site to come back later. All the best
Greate pieces. Keep writing such kind of information on your page. Im really impressed by your blog.
This piece of writing will help the internet viewers for building up new website or even a blog from start to end.
Wonderful, what a weblog it is! This website provides useful information to us, keep it up.
It is appropriate time to make some plans for the future and it is time to be happy. I have read this post and if I could I wish to suggest you few interesting things or suggestions. Perhaps you could write next articles referring to this article. I want to read more things about it!
I feel this is one of the so much important information for me. And i’m satisfied reading your article. However want to statement on few common things, The website taste is perfect, the articles is really excellent : D. Just right process, cheers
I must thank you for the efforts you have put in writing this blog. I am hoping to see the same high-grade blog posts from you in the future as well. In fact, your creative writing abilities has motivated me to get my own website now 😉
Appreciate the recommendation. Will try it out.
I have been surfing online more than three hours today, yet I never found any fascinating article like yours. It’s pretty worth enough for me. Personally, if all webmasters and bloggers made just right content as you did, the internet shall be much more useful than ever before.
Tremendous things here. I’m very glad to see your article. Thank you so much and I’m taking a look forward to touch you. Will you please drop me a mail?
Lutz, FL Psychological Assessment Resources propecia buy
I’m not sure why but this blog is loading extremely slow for me. Is anyone else having this issue or is it a problem on my end? I’ll check back later and see if the problem still exists.
Hey There. I found your blog using msn. This is an extremely well written article. I will be sure to bookmark it and come back to read more of your useful information. Thanks for the post. I will definitely comeback.
What i do not realize is in reality how you’re now not really a lot more well-appreciated than you may be right now. You are so intelligent. You understand therefore significantly with regards to this topic, produced me for my part believe it from numerous numerous angles. Its like men and women aren’t fascinated until it’s something to accomplish with Lady gaga! Your own stuffs nice. All the time maintain it up!
Way cool! Some very valid points! I appreciate you writing this article and also the rest of the site is extremely good.
It is appropriate time to make some plans for the future and it is time to be happy. I have read this post and if I could I want to suggest you few interesting things or suggestions. Perhaps you could write next articles referring to this article. I want to read more things about it!
My partner and I absolutely love your blog and find many of your post’s to be just what I’m looking for. Do you offer guest writers to write content to suit your needs? I wouldn’t mind creating a post or elaborating on most of the subjects you write related to here. Again, awesome web log!
This design is wicked! You most certainly know how to keep a reader entertained. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Great job. I really enjoyed what you had to say, and more than that, how you presented it. Too cool!
Terrific post however , I was wondering if you could write a litte more on this topic? I’d be very grateful if you could elaborate a little bit more. Cheers!
I read this post fully about the comparison of most up-to-date and previous technologies, it’s awesome article.
I was recommended this blog by my cousin. I am not sure whether this post is written by him as no one else know such detailed about my difficulty. You are wonderful! Thanks!
I think what you postedtypedthink what you postedtypedsaidthink what you postedwrotethink what you postedwrotesaidWhat you postedwrote was very logicala bunch of sense. But, what about this?think about this, what if you were to write a killer headlinetitle?content?wrote a catchier title? I ain’t saying your content isn’t good.ain’t saying your content isn’t gooddon’t want to tell you how to run your blog, but what if you added a titleheadlinetitle that grabbed a person’s attention?maybe get people’s attention?want more? I mean %BLOG_TITLE% is a little vanilla. You might peek at Yahoo’s home page and see how they createwrite post headlines to get viewers interested. You might add a related video or a related pic or two to get readers interested about what you’ve written. Just my opinion, it might bring your postsblog a little livelier.
Heya outstanding blog! Does running a blog similar to this take a great deal of work? I have virtually no knowledge of programming but I was hoping to start my own blog soon. Anyway, if you have any suggestions or tips for new blog owners please share. I know this is off topic but I just had to ask. Thanks!
I’m impressed, I must say. Rarely do I encounter a blog that’s equally educative and entertaining, and let me tell you, you have hit the nail on the head. The issue is something not enough folks are speaking intelligently about. I’m very happy that I stumbled across this in my search for something concerning this.
Have you ever considered about including a little bit more than just your articles? I mean, what you say is valuable and all. Nevertheless think about if you added some great graphics or video clips to give your posts more, “pop”! Your content is excellent but with images and clips, this site could certainly be one of the very best in its niche. Superb blog!
It’s in fact very complex in this busy life to listen news on TV, thus I only use internet for that purpose, and get the latest news.
Have you ever considered about including a little bit more than just your articles? I mean, what you say is valuable and all. However think about if you added some great pictures or video clips to give your posts more, “pop”! Your content is excellent but with images and video clips, this site could certainly be one of the very best in its niche. Superb blog!
I am really loving the theme/design of your website. Do you ever run into any internet browser compatibility problems? A couple of my blog audience have complained about my website not operating correctly in Explorer but looks great in Chrome. Do you have any tips to help fix this issue?
hey there and thank you for your information I’ve definitely picked up anything new from right here. I did however expertise a few technical issues using this site, since I experienced to reload the site many times previous to I could get it to load properly. I had been wondering if your web hosting is OK? Not that I am complaining, but sluggish loading instances times will very frequently affect your placement in google and can damage your high quality score if advertising and marketing with Adwords. Anyway I’m adding this RSS to my e-mail and can look out for a lot more of your respective intriguing content. Make sure you update this again soon.
Today, I went to the beach with my kids. I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She put the shell to her ear and screamed. There was a hermit crab inside and it pinched her ear. She never wants to go back! LoL I know this is completely off topic but I had to tell someone!
If you wish for to take much from this post then you have to apply such techniques to your won blog.
Please let me know if you’re looking for a author for your site. You have some really great posts and I think I would be a good asset. If you ever want to take some of the load off, I’d absolutely love to write some articles for your blog in exchange for a link back to mine. Please send me an e-mail if interested. Kudos!
Note The advice provided in this post is intended for informational purposes and does not constitute medical advice regarding people or pets what happens if you take too much viagra 1 spike 1 the list of sera used is shown in Table S1
Very nice article, just what I wanted to find.
Pretty nice post. I just stumbled upon your blog and wanted to say that I have really enjoyed browsing your blog posts. In any case I’ll be subscribing to your feed and I hope you write again soon!
It is appropriate time to make some plans for the future and it is time to be happy. I have read this post and if I could I want to suggest you few interesting things or suggestions. Perhaps you could write next articles referring to this article. I wish to read more things about it!
Hi there! This post couldn’t be written any better! Going through this post reminds me of my previous roommate! He constantly kept talking about this. I am going to forward this information to him. Pretty sure he will have a very good read. Many thanks for sharing!
You made some decent points there. I looked on the internet for more info about the issue and found most individuals will go along with your views on this website.
If you want to take much from this piece of writing then you have to apply such techniques to your won blog.
With havin so much content and articles do you ever run into any problems of plagorism or copyright violation? My site has a lot of exclusive content I’ve either created myself or outsourced but it looks like a lot of it is popping it up all over the web without my agreement. Do you know any techniques to help reduce content from being ripped off? I’d genuinely appreciate it.
Great post.
I love reading a post that will make people think. Also, thanks for allowing for me to comment!
A fascinating discussion is worth comment. I believe that you should write more on this subject, it might not be a taboo subject but generally people don’t discuss such subjects. To the next! Cheers!!
Ridiculous quest there. What occurred after? Good luck!
I will right away grab your rss as I can not in finding your email subscription link or newsletter service. Do you have any? Please allow me recognise so that I may subscribe. Thanks.
Howdy are using WordPress for your blog platform? I’m new to the blog world but I’m trying to get started and create my own. Do you need any coding knowledge to make your own blog? Any help would be greatly appreciated!
I was wondering if you ever considered changing the layout of your blog? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having one or two images. Maybe you could space it out better?
I enjoy what you guys are usually up too. Such clever work and exposure! Keep up the good works guys I’ve incorporated you guys to our blogroll.
Wow, that’s what I was searching for, what a stuff! present here at this weblog, thanks admin of this web site.
Hi there, yeah this post is in fact nice and I have learned lot of things from it about blogging. thanks.
After looking into a few of the blog articles on your web page, I really like your way of blogging. I book-marked it to my bookmark website list and will be checking back soon. Please check out my web site as well and let me know how you feel.
Hi, i think that i saw you visited my web site so i came to return the favor.I am trying to find things to improve my website!I suppose its ok to use some of your ideas!!
What’s up to all, the contents present at this website are really awesome for people experience, well, keep up the nice work fellows.
Pretty! This was a really wonderful post. Thank you for providing this info.
Incredible! This blog looks exactly like my old one! It’s on a completely different topic but it has pretty much the same layout and design. Excellent choice of colors!
When I originally commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get four emails with the same comment. Is there any way you can remove me from that service? Bless you!
Saved as a favorite, I like your web site!
Hi to all, how is all, I think every one is getting more from this web site, and your views are pleasant designed for new users.
magnificent post, very informative. I’m wondering why the other experts of this sector do not understand this. You should continue your writing. I am sure, you have a huge readers’ base already!
Wow, this piece of writing is nice, my sister is analyzing such things, so I am going to let know her.
Hey I know this is off topic but I was wondering if you knew of any widgets I could add to my blog that automatically tweet my newest twitter updates. I’ve been looking for a plug-in like this for quite some time and was hoping maybe you would have some experience with something like this. Please let me know if you run into anything. I truly enjoy reading your blog and I look forward to your new updates.
The other day, while I was at work, my sister stole my iPad and tested to see if it can survive a 25 foot drop, just so she can be a youtube sensation. My iPad is now broken and she has 83 views. I know this is entirely off topic but I had to share it with someone!
Hi my family member! I want to say that this article is awesome, great written and come with almost all significant infos. I’d like to see more posts like this .
Thank you, I have recently been searching for information approximately this topic for ages and yours is the best I have came upon so far. However, what about the conclusion? Are you sure about the source?
It’s not my first time to go to see this web site, i am visiting this website dailly and take nice data from here everyday.
In fact no matter if someone doesn’t know then its up to other users that they will help, so here it happens.
Great beat ! I wish to apprentice whilst you amend your web site, how can i subscribe for a blog site? The account aided me a applicable deal. I were tiny bit familiar of this your broadcast provided bright transparent concept
Great web site you have here.. It’s hard to find high-quality writing like yours these days. I truly appreciate people like you! Take care!!
I feel this is one of the so much important information for me. And i’m glad reading your article. However wanna statement on few common things, The site taste is great, the articles is really excellent : D. Just right task, cheers
I blog frequently and I genuinely appreciate your content. This great article has really peaked my interest. I will bookmark your site and keep checking for new information about once a week. I subscribed to your RSS feed as well.
Aw, this was a very nice post. Taking the time and actual effort to make a good article but what can I say I procrastinate a lot and never seem to get anything done.
I’ve been exploring for a little bit for any high-quality articles or blog posts in this kind of space . Exploring in Yahoo I eventually stumbled upon this site. Reading this info So i’m glad to exhibit that I have a very good uncanny feeling I came upon exactly what I needed. I such a lot undoubtedly will make certain to don?t forget this site and give it a look on a continuing basis.
If you want to get a great deal from this post then you have to apply such strategies to your won webpage.
Wow, that’s what I was looking for, what a information! present here at this website, thanks admin of this website.
Thanks for one’s marvelous posting! I genuinely enjoyed reading it, you are a great author.I will make sure to bookmark your blog and will eventually come back very soon. I want to encourage one to continue your great job, have a nice day!
Hello, I believe your website could be having browser compatibility issues. When I look at your website in Safari, it looks fine however when opening in Internet Explorer, it has some overlapping issues. I just wanted to give you a quick heads up! Apart from that, great blog!
Superb site you have here but I was curious if you knew of any discussion boards that cover the same topics talked about in this article? I’d really love to be a part of online community where I can get responses from other knowledgeable individuals that share the same interest. If you have any recommendations, please let me know. Cheers!
Thanks for the marvelous posting! I definitely enjoyed reading it, you can be a great author.I will ensure that I bookmark your blog and will come back later in life. I want to encourage you to definitely continue your great job, have a nice day!
This design is spectacular! You obviously know how to keep a reader entertained. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Fantastic job. I really enjoyed what you had to say, and more than that, how you presented it. Too cool!
Every weekend i used to pay a visit this website, because i want enjoyment, as this this website conations really nice funny information too.
Simply wish to say your article is as amazing. The clearness in your post is simply cool and i can assume you are a professional in this subject. Well with your permission allow me to clutch your RSS feed to stay up to date with approaching post. Thank you a million and please continue the rewarding work.
Hi there! This post couldn’t be written any better! Reading this post reminds me of my old room mate! He always kept talking about this. I will forward this article to him. Pretty sure he will have a good read. Thanks for sharing!
Hey There. I found your blog using msn. This is a very well written article. I will be sure to bookmark it and come back to read more of your useful information. Thank you for the post. I will definitely comeback.
Excellent post however , I was wondering if you could write a litte more on this topic? I’d be very grateful if you could elaborate a little bit more. Bless you!
Regards! A good amount of tips!
best nursing paper writing service free will writing service charity best resume writing service for veterans
I all the time used to read article in news papers but now as I am a user of internet thus from now I am using net for articles or reviews, thanks to web.
Chicago, Ill The American Dietetic Association, 2000, pp 79 89 buy cialis cheap The purpose is to find the lowest, most tolerable, and yet effective dose for the individual patient
Hey! I just wanted to ask if you ever have any problems with hackers? My last blog (wordpress) was hacked and I ended up losing a few months of hard work due to no data backup. Do you have any solutions to prevent hackers?
Nice post. I was checking continuously this blog and I am impressed! Very useful information particularly the last part 🙂 I care for such info a lot. I was seeking this particular info for a long time. Thank you and good luck.
Pretty section of content. I just stumbled upon your web site and in accession capital to assert that I acquire in fact enjoyed account your blog posts. Any way I’ll be subscribing to your augment and even I achievement you access consistently fast.
Greate article. Keep writing such kind of information on your blog. Im really impressed by your site.
Highly energetic blog, I liked that a lot. Will there be a part 2?
Spot on with this write-up, I truly feel this web site needs much more attention. I’ll probably be back again to read through more, thanks for the information!
If some one wants expert view regarding blogging after that i suggest him/her to go to see this weblog, Keep up the good job.
Pretty section of content. I just stumbled upon your web site and in accession capital to assert that I acquire in fact enjoyed account your blog posts. Any way I’ll be subscribing to your augment and even I achievement you access consistently rapidly.
Great goods from you, man. I’ve have in mind your stuff prior to and you’re simply too magnificent. I really like what you’ve obtained here, really like what you’re stating and the best way through which you are saying it. You make it entertaining and you still take care of to stay it sensible. I can not wait to read far more from you. This is actually a great site.
We are a group of volunteers and starting a new scheme in our community. Your web site provided us with helpful information to work on. You have performed an impressive process and our whole community can be grateful to you.
I am really loving the theme/design of your website. Do you ever run into any web browser compatibility problems? A handful of my blog visitors have complained about my website not operating correctly in Explorer but looks great in Chrome. Do you have any ideas to help fix this issue?
Hi there, constantly i used to check website posts here early in the dawn, as i like to learn more and more.
I like the valuable information you provide in your articles. I will bookmark your weblog and check again here frequently. I am quite certain I will learn plenty of new stuff right here! Good luck for the next!
It’s an awesome piece of writing for all the internet viewers; they will get benefit from it I am sure.
whoah this blog is great i really like reading your articles. Stay up the good work! You understand, many individuals are hunting around for this info, you can help them greatly.
Great goods from you, man. I’ve take into account your stuff prior to and you’re simply too wonderful. I really like what you’ve obtained here, really like what you’re stating and the way through which you assert it. You make it entertaining and you still take care of to stay it smart. I can not wait to read far more from you. This is actually a terrific website.
It’s awesome for me to have a web site, which is helpful for my experience. thanks admin
Having read this I thought it was extremely informative. I appreciate you finding the time and effort to put this information together. I once again find myself spending way too much time both reading and commenting. But so what, it was still worth it!
I was wondering if you ever considered changing the layout of your blog? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having one or two images. Maybe you could space it out better?
I have been surfing online more than three hours today, yet I never found any fascinating article like yours. It’s pretty value enough for me. Personally, if all webmasters and bloggers made just right content as you did, the internet will be much more useful than ever before.
Your way of describing everything in this post is actually good, all be able to easily know it, Thanks a lot.
I loved as much as you will receive carried out right here. The sketch is tasteful, your authored subject matter stylish. nonetheless, you command get bought an impatience over that you wish be delivering the following. unwell unquestionably come further formerly again since exactly the same nearly a lot often inside case you shield this increase.
Spot on with this write-up, I seriously think this website needs much more attention. I’ll probably be back again to read more, thanks for the information!
Greate article. Keep writing such kind of information on your page. Im really impressed by your site.
It is not my first time to pay a visit this web site, i am visiting this web site dailly and take pleasant data from here every day.
Fantastic goods from you, man. I’ve understand your stuff previous to and you’re just too magnificent. I really like what you’ve acquired here, really like what you’re stating and the way in which you say it. You make it entertaining and you still take care of to keep it sensible. I cant wait to read far more from you. This is actually a terrific site.
Have you ever considered about including a little bit more than just your articles? I mean, what you say is fundamental and all. However just imagine if you added some great pictures or video clips to give your posts more, “pop”! Your content is excellent but with images and video clips, this website could certainly be one of the most beneficial in its niche. Wonderful blog!
I believe what you postedtypedthink what you postedtypedthink what you postedtypedsaidthink what you postedtypedsaidWhat you postedwrote was very logicala lot of sense. But, what about this?consider this, what if you were to write a killer headlinetitle?content?wrote a catchier title? I ain’t saying your content isn’t good.ain’t saying your content isn’t gooddon’t want to tell you how to run your blog, but what if you added a titleheadlinetitle that grabbed people’s attention?maybe get a person’s attention?want more? I mean %BLOG_TITLE% is a little vanilla. You could peek at Yahoo’s home page and watch how they createwrite news headlines to get viewers interested. You might add a video or a related picture or two to get readers interested about what you’ve written. Just my opinion, it could bring your postsblog a little livelier.
You actually mentioned this terrifically.
student essay writing writing an essay outline writing essay services
I simply could not leave your web site prior to suggesting that I extremely enjoyed the standard information a person supply on your visitors? Is going to be back regularly in order to inspect new posts
I have been surfing online more than three hours today, yet I never found any interesting article like yours. It’s pretty worth enough for me. In my opinion, if all website owners and bloggers made good content as you did, the internet shall be much more useful than ever before.
I’ve been exploring for a little for any high-quality articles or blog posts in this kind of space . Exploring in Yahoo I at last stumbled upon this site. Reading this info So i’m satisfied to show that I have a very just right uncanny feeling I came upon exactly what I needed. I such a lot unquestionably will make certain to don?t fail to remember this web site and give it a look on a continuing basis.
Incredible quest there. What occurred after? Thanks!
It’s remarkable to visit this site and reading the views of all mates concerning this post, while I am also eager of getting familiarity.
Howdy just wanted to give you a quick heads up and let you know a few of the images aren’t loading correctly. I’m not sure why but I think its a linking issue. I’ve tried it in two different internet browsers and both show the same results.
Thanks for one’s marvelous posting! I quite enjoyed reading it, you will be a great author.I will make sure to bookmark your blog and will often come back in the future. I want to encourage that you continue your great writing, have a nice day!
Howdy! I know this is kinda off topic but I was wondering if you knew where I could find a captcha plugin for my comment form? I’m using the same blog platform as yours and I’m having trouble finding one? Thanks a lot!
Excellent post. I used to be checking continuously this blog and I am inspired! Very useful information specially the ultimate phase 🙂 I take care of such info a lot. I used to be seeking this particular info for a long timelong time. Thank you and good luck.
An impressive share! I have just forwarded this onto a coworker who had been doing a little research on this. And he in fact bought me breakfast because I discovered it for him… lol. So let me reword this…. Thank YOU for the meal!! But yeah, thanx for spending the time to discuss this issue here on your internet site.
Hi there just wanted to give you a quick heads up. The text in your content seem to be running off the screen in Safari. I’m not sure if this is a format issue or something to do with internet browser compatibility but I thought I’d post to let you know. The layout look great though! Hope you get the problem solved soon. Cheers
Hey there! I know this is kind of off-topic but I had to ask. Does running a well-established blog like yours take a massive amount work? I’m completely new to writing a blog but I do write in my diary daily. I’d like to start a blog so I will be able to share my experience and views online. Please let me know if you have any suggestions or tips for new aspiring bloggers. Appreciate it!
lightdatings life: date online – best dating site
Oh my goodness! Incredible article dude! Many thanks, However I am going through problems with your RSS. I don’t know why I am unable to subscribe to it. Is there anyone else getting the same RSS problems? Anybody who knows the solution will you kindly respond? Thanx!!
Thank you for another informative blog. Where else may I am getting that kind of info written in such a perfect approach? I have a undertaking that I am simply now operating on, and I have been at the glance out for such information.
Hi mates, its great post about tutoringand fully explained, keep it up all the time.
Hi there it’s me, I am also visiting this website daily, this web site is actually good and the people are actually sharing pleasant thoughts.
You ought to take part in a contest for one of the best sites on the internet. I am going to recommend this blog!
Hi to all, the contents present at this site are truly awesome for people experience, well, keep up the nice work fellows.
I think this is one of the so much important information for me. And i’m satisfied reading your article. However wanna observation on few basic things, The site taste is ideal, the articles is in point of fact excellent : D. Just right activity, cheers
I’ve been exploring for a little bit for any high-quality articles or blog posts in this kind of space . Exploring in Yahoo I finally stumbled upon this web site. Reading this info So i’m glad to exhibit that I have a very just right uncanny feeling I came upon exactly what I needed. I so much surely will make certain to don?t put out of your mind this site and give it a look on a continuing basis.
Exceptional post but I was wondering if you could write a litte more on this topic? I’d be very grateful if you could elaborate a little bit more. Appreciate it!
Hey there! I know this is kinda off topic however , I’d figured I’d ask. Would you be interested in exchanging links or maybe guest writing a blog article or vice-versa? My website discusses a lot of the same subjects as yours and I feel we could greatly benefit from each other. If you happen to be interested feel free to send me an e-mail. I look forward to hearing from you! Terrific blog by the way!
prednisone 20mg by mail order: https://prednisone1st.store/# prednisone 20mg price in india
Keep on working, great job!
WOW just what I was searching for. Came here by searching for %keyword%
Hi there i am kavin, its my first time to commenting anywhere, when i read this post i thought i could also make comment due to this brilliant post.
Usually I do not read article on blogs, however I wish to say that this write-up very pressured me to try and do so! Your writing taste has been amazed me. Thank you, quite great article.
Hey, I think your blog might be having browser compatibility issues. When I look at your blog in Ie, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, wonderful blog!
Hi there, I enjoy reading all of your article. I like to write a little comment to support you.
I love your blog.. very nice colors & theme. Did you design this website yourself or did you hire someone to do it for you? Plz reply as I’m looking to design my own blog and would like to know where u got this from. cheers
If you wish for to get a great deal from this post then you have to apply such strategies to your won webpage.
Hi! Someone in my Myspace group shared this site with us so I came to take a look. I’m definitely enjoying the information. I’m book-marking and will be tweeting this to my followers! Terrific blog and fantastic design and style.
I want to to thank you for this great read!! I definitely enjoyed every little bit of it. I have you book-marked to check out new stuff you post
Hi there i am kavin, its my first time to commenting anywhere, when i read this post i thought i could also make comment due to this brilliant piece of writing.
Hi there, I desire to subscribe for this webpage to take latest updates, so where can i do it please help.
I am truly pleased to read this blog posts which consists of lots of helpful information, thanks for providing these information.
The other day, while I was at work, my sister stole my iPad and tested to see if it can survive a 25 foot drop, just so she can be a youtube sensation. My iPad is now broken and she has 83 views. I know this is entirely off topic but I had to share it with someone!
Hmm is anyone else experiencing problems with the images on this blog loading? I’m trying to figure out if its a problem on my end or if it’s the blog. Any responses would be greatly appreciated.
I pay a visit daily some web pages and information sites to read articles or reviews, except this webpage provides quality based articles.
This is a very good tip especially to those new to the blogosphere. Short but very accurate information Thanks for sharing this one. A must read article!
Link exchange is nothing else except it is only placing the other person’s website link on your page at proper place and other person will also do same in favor of you.
Since the admin of this web site is working, no doubt very rapidly it will be well-known, due to its quality contents.
Good article. I certainly love this website. Continue the good work!
I like the valuable information you supply for your articles. I will bookmark your weblog and check again here frequently. I am rather certain I will be informed plenty of new stuff right here! Good luck for the following!
Great delivery. Outstanding arguments. Keep up the good work.
If some one needs expert view regarding blogging and site-building then i propose him/her to go to see this website, Keep up the nice job.
Hi to all, how is all, I think every one is getting more from this web site, and your views are pleasant designed for new people.
It’s very trouble-free to find out any topic on net as compared to books, as I found this article at this site.
Pretty! This was a really wonderful post. Thanks for providing this info.
Since the admin of this site is working, no doubt very rapidly it will be well-known, due to its quality contents.
Having read this I thought it was very informative. I appreciate you finding the time and effort to put this informative article together. I once again find myself spending way too much time both reading and commenting. But so what, it was still worth it!
Hey! I’m at work browsing your blog from my new iphone 3gs! Just wanted to say I love reading your blog and look forward to all your posts! Keep up the outstanding work!
Oh my goodness! Incredible article dude! Thanks, However I am going through issues with your RSS. I don’t know why I am unable to subscribe to it. Is there anybody else getting the same RSS problems? Anyone who knows the solution will you kindly respond? Thanx!!
you are in point of fact a good webmaster. The web site loading speed is incredible. It kind of feels that you are doing any unique trick. In addition, The contents are masterpiece. you have performed a magnificent task in this matter!
I feel this is one of the such a lot important information for me. And i’m glad reading your article. However wanna remark on few common things, The site taste is perfect, the articles is really excellent : D. Good process, cheers
It is perfect time to make a few plans for the future and it is time to be happy. I have read this submit and if I may just I want to recommend you few interesting things or suggestions. Perhaps you could write next articles referring to this article. I want to read more things approximately it!
Hi there to every one, it’s in fact a good for me to pay a visit this site, it consists of precious Information.
This website truly has all of the info I wanted about this subject and didn’t know who to ask.
whoah this blog is great i love reading your articles. Stay up the good work! You realize, a lot of people are searching around for this info, you can help them greatly.
I loved as much as you will receive carried out right here. The sketch is tasteful, your authored subject matter stylish. nonetheless, you command get bought an nervousness over that you wish be delivering the following. unwell unquestionably come further formerly again since exactly the same nearly a lot often inside case you shield this increase.
Excellent blog here! Also your site rather a lot up fast! What host are you the use of? Can I am getting your associate link in your host? I want my website loaded up as fast as yours lol
Undeniably believe that which you stated. Your favorite justification appeared to be on the net the simplest thing to be aware of. I say to you, I definitely get irked while people consider worries that they plainly do not know about. You managed to hit the nail upon the top and also defined out the whole thing without having side effect , people can take a signal. Will likely be back to get more. Thanks
Hey, I think your blog might be having browser compatibility issues. When I look at your blog site in Chrome, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, great blog!
Pretty section of content. I just stumbled upon your web site and in accession capital to assert that I acquire in fact enjoyed account your blog posts. Any way I’ll be subscribing to your augment and even I achievement you access consistently fast.
Hi there friends, its great article regarding educationand completely explained, keep it up all the time.
Way cool! Some very valid points! I appreciate you writing this post and also the rest of the site is very good.
I got this website from my friend who informed me concerning this site and now this time I am visiting this site and reading very informative articles here.
Yes! Finally something about %keyword1%.
These are really wonderful ideas in regarding blogging. You have touched some pleasant points here. Any way keep up wrinting.
Hi Dear, are you truly visiting this website daily, if so then you will absolutely take pleasant experience.
Wonderful goods from you, man. I’ve understand your stuff prior to and you’re simply too magnificent. I really like what you’ve acquired here, really like what you’re stating and the best way through which you assert it. You are making it entertaining and you still take care of to stay it smart. I cant wait to read far more from you. This is actually a terrific site.
Every weekend i used to pay a visit this web site, as i want enjoyment, as this this web site conations in fact nice funny stuff too.
I truly love your site.. Pleasant colors & theme. Did you develop this site yourself? Please reply back as I’m trying to create my own blog and want to know where you got this from or exactly what the theme is called. Thanks!
Thank you for another magnificent article. Where else may anyone get that kind of information in such a perfect approach of writing? I have a presentation next week, and I am at the look for such information.
What’s up, after reading this awesome article i am too glad to share my experience here with friends.
hi!,I really like your writing so so much! proportion we keep up a correspondence more approximately your post on AOL? I need an expert in this area to solve my problem. May be that is you! Taking a look forward to peer you.
Please let me know if you’re looking for a article author for your weblog. You have some really great posts and I think I would be a good asset. If you ever want to take some of the load off, I’d really like to write some material for your blog in exchange for a link back to mine. Please blast me an e-mail if interested. Many thanks!
Hi there friends, nice post and pleasant arguments commented here, I am truly enjoying by these.
Unquestionably believe that which you stated. Your favorite justification appeared to be on the internet the simplest thing to be aware of. I say to you, I definitely get irked while people consider worries that they plainly do not know about. You managed to hit the nail upon the top as well as defined out the whole thing without having side effect , people can take a signal. Will likely be back to get more. Thanks
fantastic issues altogether, you just won a emblem new reader. What could you suggest in regards to your submit that you made a few days ago? Any positive?
Excellent blog! Do you have any suggestions for aspiring writers? I’m planning to start my own site soon but I’m a little lost on everything. Would you propose starting with a free platform like WordPress or go for a paid option? There are so many choices out there that I’m totally confused .. Any suggestions? Cheers!
Hey There. I found your blog using msn. This is a very smartly written article. I will be sure to bookmark it and come back to read more of your useful information. Thank you for the post. I will definitely comeback.
You really make it seem so easy with your presentation but I find this topic to be really something which I think I would never understand. It seems too complicated and very broad for me. I am looking forward for your next post, I will try to get the hang of it!
No matter if some one searches for his essential thing, thus he/she needs to be available that in detail, so that thing is maintained over here.
Hurrah! Finally I got a website from where I can really take helpful information regarding my study and knowledge.
This is a very good tip especially to those new to the blogosphere. Short but very accurate information Thanks for sharing this one. A must read article!
Everything is very open with a clear explanation of the issues. It was truly informative. Your website is very useful. Thank you for sharing!
You can definitely see your enthusiasm in the article you write. The world hopes for more passionate writers like you who aren’t afraid to mention how they believe. Always go after your heart.
This piece of writing will help the internet viewers for creating new weblog or even a blog from start to end.
You really make it seem so easy with your presentation but I find this topic to be really something which I think I would never understand. It seems too complicated and very broad for me. I am looking forward for your next post, I will try to get the hang of it!
It is appropriate time to make some plans for the future and it is time to be happy. I have read this post and if I could I wish to suggest you few interesting things or advice. Perhaps you could write next articles referring to this article. I want to read more things about it!
Hi friends, its enormous article about teachingand completely explained, keep it up all the time.
Hello would you mind letting me know which webhost you’re utilizing? I’ve loaded your blog in 3 completely different web browsers and I must say this blog loads a lot quicker then most. Can you suggest a good web hosting provider at a honest price? Thanks a lot, I appreciate it!
Fantastic beat ! I wish to apprentice while you amend your web site, how can i subscribe for a blog site? The account aided me a acceptable deal. I had been tiny bit acquainted of this your broadcast provided bright clear concept
Your style is so unique compared to other people I have read stuff from. Thank you for posting when you have the opportunity, Guess I will just bookmark this web site.
What’s up to every body, it’s my first go to see of this blog; this blog contains remarkable and actually fine stuff designed for readers.
I was wondering if you ever considered changing the page layout of your blog? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having one or two images. Maybe you could space it out better?
Hey There. I found your blog using msn. This is a very well written article. I will be sure to bookmark it and come back to read more of your useful information. Thank you for the post. I will definitely comeback.
Wow, that’s what I was searching for, what a data! present here at this weblog, thanks admin of this site.
After checking out a few of the blog posts on your site, I really like your way of blogging. I saved it to my bookmark site list and will be checking back soon. Please check out my web site as well and let me know what you think.
Hello there, just became aware of your blog through Google, and found that it is really informative. I’m gonna watch out for brussels. I will appreciate if you continue this in future. Lots of people will be benefited from your writing. Cheers!
WOW just what I was searching for. Came here by searching for %keyword%
Its like you read my mind! You seem to understand so much approximately this, like you wrote the ebook in it or something. I think that you simply could do with some % to force the message house a bit, however other than that, this is fantastic blog. An excellent read. I’ll definitely be back.
Hi, always i used to check website posts here early in the morning, since i like to learn more and more.
First off I want to say great blog! I had a quick question that I’d like to ask if you don’t mind. I was curious to know how you center yourself and clear your thoughts before writing. I have had a difficult time clearing my mind in getting my thoughts out. I do enjoy writing but it just seems like the first 10 to 15 minutes are usually wasted just trying to figure out how to begin. Any suggestions or tips? Thanks!
I love it when folks come together and share views. Great website, keep it up!
Hello there, You have done an excellent job. I will definitely digg it and personally recommend to my friends. I am sure they will be benefited from this site.
Article writing is also a fun, if you be acquainted with then you can write otherwise it is difficult to write.
Howdy! Someone in my Myspace group shared this site with us so I came to take a look. I’m definitely enjoying the information. I’m book-marking and will be tweeting this to my followers! Outstanding blog and outstanding style and design.
Hi there, all is going well here and ofcourse every one is sharing information, that’s in fact good, keep up writing.
Представительский мужской эромассаж Москва в спа салоне
Oh my goodness! Incredible article dude! Thanks, However I am encountering problems with your RSS. I don’t know why I am unable to subscribe to it. Is there anybody else getting identical RSS problems? Anybody who knows the solution will you kindly respond? Thanx!!
When someone writes an post he/she maintains the thought of a user in his/her mind that how a user can know it. Thus that’s why this post is amazing. Thanks!
Неповторимый частный эротический массаж в Москве телефон
Недорогой частный эротический массаж Москва – тайский салон
Hello there! This post couldn’t be written any better! Reading this post reminds me of my good old room mate! He always kept talking about this. I will forward this post to him. Pretty sure he will have a good read. Thank you for sharing!
Красивый частный эромассаж в Москве база вип спа
Исключительный частный эромассаж в Москве – тайский салон
Неповторимый частный эромассаж Москва с массажистками на выбор
Привилегированный мужской эротический массаж в Москве с джакузи
Hi all, here every one is sharing such knowledge, thus it’s pleasant to read this weblog, and I used to pay a visit this webpage every day.
Исключительный частный эромассаж Москва с бассейном
Грамотный мужской эротический массаж Москва с массажистками на выбор
Авторский мужской эромассаж Москва в spa
hi!,I really like your writing so much! proportion we keep in touch more approximately your post on AOL? I need an expert in this space to unravel my problem. May be that is you! Taking a look forward to peer you.
Отборный частный эротический массаж в Москве выбрать лучший
Для пар мужской эротический массаж в Москве выбрать лучший
Having read this I thought it was very informative. I appreciate you finding the time and effort to put this short article together. I once again find myself spending a significant amount of time both reading and leaving comments. But so what, it was still worth it!
VIP частный эромассаж Москва с бассейном
Для пар мужской эротический массаж Москва с массажистками на выбор
This site really has all of the info I wanted about this subject and didn’t know who to ask.
Грамотный частный эротический массаж Москва цена
I’m impressed, I must say. Rarely do I encounter a blog that’s equally educative and interesting, and let me tell you, you have hit the nail on the head. The issue is something not enough people are speaking intelligently about. I am very happy that I stumbled across this in my search for something concerning this.
Представительский мужской эротический массаж в Москве с массажистками на выбор
Do you mind if I quote a couple of your posts as long as I provide credit and sources back to your weblog? My blog site is in the very same area of interest as yours and my visitors would certainly benefit from a lot of the information you present here. Please let me know if this okay with you. Appreciate it!
Представительский мужской эротический массаж в Москве релакс спа
This web site definitely has all of the info I wanted about this subject and didn’t know who to ask.
Вип частный эротический массаж в Москве телефон
Вип частный эротический массаж в Москве с массажистками на выбор
Pretty section of content. I just stumbled upon your web site and in accession capital to assert that I acquire in fact enjoyed account your blog posts. Any way I’ll be subscribing to your augment and even I achievement you access consistently rapidly.
tadalafil side effects http://tadalafilise.cyou/# generic cialis tadalafil
where to order tadalafil tablets http://tadalafilise.cyou/# best price usa tadalafil
Unquestionably believe that that you stated. Your favourite justification appeared to be at the net the simplest thing to keep in mind of. I say to you, I definitely get irked at the same time as folks consider worries that they plainly do not recognise about. You controlled to hit the nail upon the top as well as defined out the whole thing with no need side effect , folks can take a signal. Will likely be back to get more. Thank you
I am regular reader, how are you everybody? This post posted at this web site is really pleasant.
Hey There. I found your blog the use of msn. This is an extremely smartly written article. I will be sure to bookmark it and come back to read more of your useful information. Thank you for the post. I will definitely comeback.
Have you ever considered about including a little bit more than just your articles? I mean, what you say is valuable and all. Nevertheless think of if you added some great photos or video clips to give your posts more, “pop”! Your content is excellent but with images and video clips, this website could undeniably be one of the greatest in its niche. Wonderful blog!
It’s very trouble-free to find out any topic on net as compared to books, as I found this post at this site.
Hey there! This is kind of off topic but I need some advice from an established blog. Is it tough to set up your own blog? I’m not very techincal but I can figure things out pretty fast. I’m thinking about creating my own but I’m not sure where to start. Do you have any tips or suggestions? With thanks
obviously like your website however you need to check the spelling on quite a few of your posts. A number of them are rife with spelling problems and I in finding it very bothersome to tell the truth however I will certainly come back again.
Quality posts is the key to invite the people to pay a visit the web site, that’s what this site is providing.
how much does generic cialis cost trova miglior prezzo cialis 800 black
Simply want to say your article is as surprising. The clearness in your post is simply nice and i can assume you are an expert on this subject. Well with your permission allow me to grab your RSS feed to keep up to date with forthcoming post. Thanks a million and please continue the gratifying work.
Does your website have a contact page? I’m having a tough time locating it but, I’d like to send you an e-mail. I’ve got some creative ideas for your blog you might be interested in hearing. Either way, great website and I look forward to seeing it improve over time.
Fine way of explaining, and nice piece of writing to get information regarding my presentation subject, which i am going to deliver in academy.
I will right away grasp your rss as I can not find your email subscription link or newsletter service. Do you have any? Please permit me recognize so that I may subscribe. Thanks.
Why users still use to read news papers when in this technological world everything is accessible on net?
Hi there this is kinda of off topic but I was wondering if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding knowledge so I wanted to get advice from someone with experience. Any help would be greatly appreciated!
Dear pregworld.org admin, You always provide in-depth analysis and understanding.
Appreciating the dedication you put into your website and in depth information you present. It’s good to come across a blog every once in a while that isn’t the same out of date rehashed material. Wonderful read! I’ve saved your site and I’m including your RSS feeds to my Google account.
Saved as a favorite, I really like your blog!
Hello there! This article couldn’t be written any better! Looking at this post reminds me of my previous roommate! He always kept talking about this. I’ll forward this information to him. Pretty sure he will have a good read. Thank you for sharing!
For latest news you have to go to see web and on internet I found this site as a most excellent website for latest updates.
Unquestionably believe that which you stated. Your favorite justification appeared to be on the internet the simplest thing to be aware of. I say to you, I definitely get irked while people consider worries that they plainly do not know about. You managed to hit the nail upon the top as well as defined out the whole thing without having side effect , people can take a signal. Will likely be back to get more. Thanks
I read this post fully about the comparison of newest and preceding technologies, it’s awesome article.
natural substitute for cialis cialis 5mg canada cialis 10mg vs 20mg
What’s up to all, the contents present at this site are really awesome for people experience, well, keep up the nice work fellows.
Undeniably believe that which you stated. Your favorite justification appeared to be on the net the simplest thing to be aware of. I say to you, I definitely get irked while people consider worries that they plainly do not know about. You managed to hit the nail upon the top as well as defined out the whole thing without having side effect , people can take a signal. Will likely be back to get more. Thanks
Do you have a spam issue on this website; I also am a blogger, and I was wanting to know your situation; many of us have created some nice methods and we are looking to trade methods with other folks, be sure to shoot me an e-mail if interested.
Way cool! Some very valid points! I appreciate you writing this post and the rest of the site is very good.
Can you tell us more about this? I’d like to find out more details.
I’m now not sure where you are getting your info, however good topic. I needs to spend a while learning more or working out more. Thank you for magnificent information I used to be looking for this information for my mission.
What’s up, everything is going perfectly here and ofcourse every one is sharing data, that’s truly fine, keep up writing.
Greate pieces. Keep writing such kind of information on your page. Im really impressed by your blog.
cialis forum cialis tadalafil 20 mg tablets tadalafil 5mg price in india
We are a gaggle of volunteers and starting a new scheme in our community. Your site provided us with helpful information to work on. You have performed an impressive task and our whole community can be grateful to you.
I think this is one of the most significant information for me. And i’m glad reading your article. But want to remark on few general things, The site style is perfect, the articles is really nice : D. Good job, cheers
I’d like to thank you for the efforts you have put in writing this website. I’m hoping to see the same high-grade blog posts from you in the future as well. In fact, your creative writing abilities has inspired me to get my own website now 😉
This post provides clear idea for the new people of blogging, that in fact how to do blogging and site-building.
Разрешение на строительство — это официальный документ, выдаваемый полномочными ведомствами государственной власти или территориального руководства, который позволяет начать строительную деятельность или производство строительных операций.
РНС в строительстве определяет правовые основания и требования к строительному процессу, включая предусмотренные типы работ, приемлемые материалы и техники, а также включает строительные регламенты и комплексы защиты. Получение разрешения на строительство является обязательным документов для строительной сферы.
Simply wish to say your article is as amazing. The clearness in your publish is simply spectacular and i can assume you are a professional in this subject. Well with your permission allow me to grab your RSS feed to stay up to date with approaching post. Thank you a million and please keep up the rewarding work.
Excellent article! We will be linking to this great post on our site. Keep up the good writing.
Hello there, You have done a great job. I will definitely digg it and personally recommend to my friends. I am sure they will be benefited from this site.
When someone writes an piece of writing he/she keeps the plan of a user in his/her mind that how a user can know it. So that’s why this post is amazing. Thanks!
canadian cialis 200 mg symptomes insuffisance cardiaque where to buy tadalafil
My family members all the time say that I am wasting my time here at net, but I know I am getting experience daily by reading such pleasant articles.
Hi there friends, how is all, and what you wish for to say regarding this post, in my view its actually remarkable in favor of me.
I am truly thankful to the owner of this web site who has shared this wonderful piece of writing at here.
I know this site gives quality dependent posts and other data, is there any other web site which gives such stuff in quality?
Thank you, I have recently been searching for information approximately this topic for ages and yours is the best I have came upon so far. However, what concerning the conclusion? Are you positive about the source?
Im not that much of a online reader to be honest but your blogs really nice, keep it up! I’ll go ahead and bookmark your site to come back later. All the best
This is a very good tip especially to those new to the blogosphere. Short but very accurate information Thanks for sharing this one. A must read article!
I know this site gives quality based articles and other data, is there any other web site which offers such things in quality?
Heya! I’m at work browsing your blog from my new iphone 4! Just wanted to say I love reading your blog and look forward to all your posts! Keep up the fantastic work!
tadalafil 5mg price in india canadian pharmacies that ship to us cialis 5mg canada pharmacy
To the pregworld.org owner, Well done!
I all the time emailed this webpage post page to all my associates, because if like to read it after that my links will too.
I was very happy to find this website. I wanted to thank you for your time due to this wonderful read!! I definitely appreciated every little bit of it and I have you saved as a favorite to check out new stuff on your blog.
Greetings! Very helpful advice within this article! It is the little changes which will make the largest changes. Thanks a lot for sharing!
Pretty great post. I simply stumbled upon your blog and wanted to mention that I have really enjoyed browsing your blog posts. In any case I’ll be subscribing for your feed and I am hoping you write again soon!
After exploring a few of the blog articles on your web page, I really like your way of blogging. I book marked it to my bookmark website list and will be checking back soon. Take a look at my web site as well and let me know how you feel.
Thank you for the auspicious writeup. It in fact was a leisure account it. Glance complex to far introduced agreeable from you! By the way, how can we communicate?
Appreciation to my father who shared with me concerning this website, this website is really awesome.
Hey there! This is kind of off topic but I need some advice from an established blog. Is it very difficult to set up your own blog? I’m not very techincal but I can figure things out pretty fast. I’m thinking about creating my own but I’m not sure where to start. Do you have any points or suggestions? Thank you
20 mg tadalafil cost cialis black online tadalafil super active 20 mg
Fantastic beat ! I wish to apprentice whilst you amend your site, how can i subscribe for a blog site? The account aided me a appropriate deal. I have been tiny bit familiar of this your broadcast provided brilliant transparent concept
I’ve read several good stuff here. Definitely value bookmarking for revisiting. I wonder how so much attempt you put to create this kind of great informative web site.
Hi, this weekend is pleasant designed for me, since this time i am reading this wonderful informative post here at my home.
Wow, that’s what I was seeking for, what a information! present here at this webpage, thanks admin of this site.
It’s remarkable in favor of me to have a site, which is useful designed for my knowledge. thanks admin
Howdy, i read your blog occasionally and i own a similar one and i was just wondering if you get a lot of spam responses? If so how do you reduce it, any plugin or anything you can suggest? I get so much lately it’s driving me insane so any assistance is very much appreciated.
Hi there, I found your blog by means of Google even as searching for a comparable topic, your web site got here up, it appears good. I have bookmarked it in my google bookmarks.
Hi, after reading this awesome article i am also cheerful to share my familiarity here with friends.
Hi there to all, how is all, I think every one is getting more from this site, and your views are pleasant designed for new viewers.
take cialis pills cialis vs flomax for bph cialis vs viagra for bph
I’m not sure where you are getting your info, but good topic. I needs to spend some time learning more or understanding more. Thanks for magnificent information I was looking for this information for my mission.
Thanks for finally writing about > %blog_title% < Liked it!
Hi! I know this is kind of off-topic but I had to ask. Does building a well-established blog like yours take a lot of work? I’m completely new to writing a blog but I do write in my diary on a daily basis. I’d like to start a blog so I can share my own experience and thoughts online. Please let me know if you have any suggestions or tips for new aspiring bloggers. Appreciate it!
Unquestionably consider that that you stated. Your favourite justification appeared to be at the net the simplest thing to keep in mind of. I say to you, I definitely get irked whilst folks consider worries that they plainly do not recognize about. You controlled to hit the nail upon the top as well as defined out the whole thing with no need side effect , folks can take a signal. Will likely be back to get more. Thank you
Hello there, just became aware of your blog through Google, and found that it is really informative. I’m gonna watch out for brussels. I will appreciate if you continue this in future. A lot of people will be benefited from your writing. Cheers!
My spouse and I stumbled over here from a different page and thought I might check things out. I like what I see so now i’m following you. Look forward to checking out your web page for a second time.
hey there and thank you for your information I’ve definitely picked up anything new from right here. I did however expertise a few technical issues using this site, since I experienced to reload the web site many times previous to I could get it to load properly. I had been wondering if your hosting is OK? Not that I am complaining, but sluggish loading instances times will often affect your placement in google and can damage your quality score if advertising and marketing with Adwords. Anyway I’m adding this RSS to my e-mail and can look out for a lot more of your respective interesting content. Make sure you update this again soon.
Wow, marvelous blog layout! How long have you been blogging for? you make blogging look easy. The overall look of your web site is wonderful, let alone the content!
Thanks in favor of sharing such a good thought, piece of writing is nice, thats why i have read it completely
This is a good tip especially to those new to the blogosphere. Brief but very accurate information Thanks for sharing this one. A must read article!
What’s up to all, how is everything, I think every one is getting more from this site, and your views are good for new users.
This is a topic that’s close to my heart… Take care! Where are your contact details though?
Great info. Lucky me I came across your site by accident (stumbleupon). I have bookmarked it for later!
I don’t even know the way I ended up here, however I thought this publish used to be good. I don’t realize who you are however definitely you are going to a famous blogger should you are not already. Cheers!
Thanks for your personal marvelous posting! I definitely enjoyed reading it, you are a great author. I will always bookmark your blog and will often come back later in life. I want to encourage yourself to continue your great writing, have a nice holiday weekend!
If you want to increase your experience simply keep visiting this web site and be updated with the latest information posted here.
I am extremely impressed with your writing skills and also with the layout on your blog. Is this a paid theme or did you customize it yourself? Either way keep up the nice quality writing, it’s rare to see a nice blog like this one nowadays.
This is very fascinating, You are an overly professional blogger. I have joined your feed and sit up for seeking more of your wonderful post. Also, I have shared your web site in my social networks
Wonderful article! We will be linking to this great post on our site. Keep up the good writing.
Simply want to say your article is as amazing. The clearness in your post is simply excellent and i can assume you are an expert on this subject. Well with your permission allow me to grab your RSS feed to keep up to date with forthcoming post. Thanks a million and please continue the gratifying work.
I believe what you postedwrotethink what you postedwrotebelieve what you postedtypedthink what you postedtypedWhat you postedwrotesaid was very logicala lot of sense. But, what about this?think about this, what if you were to write a killer headlinetitle?content?wrote a catchier title? I ain’t saying your content isn’t good.ain’t saying your content isn’t gooddon’t want to tell you how to run your blog, but what if you added a titlesomethingheadlinetitle that grabbed people’s attention?maybe get a person’s attention?want more? I mean %BLOG_TITLE% is a little plain. You might peek at Yahoo’s home page and watch how they createwrite news headlines to get viewers interested. You might add a video or a related picture or two to get readers interested about what you’ve written. Just my opinion, it could bring your postsblog a little livelier.
I don’t even know how I ended up here, but I thought this post was good. I don’t know who you are but definitely you are going to a famous blogger if you are not already 😉 Cheers!
Nice respond in return of this query with solid arguments and explaining everything about that.
Pretty! This was an extremely wonderful post. Thank you for providing this information.
Greetings from Los angeles! I’m bored to tears at work so I decided to check out your website on my iphone during lunch break. I enjoy the info you present here and can’t wait to take a look when I get home. I’m shocked at how quick your blog loaded on my cell phone .. I’m not even using WIFI, just 3G .. Anyhow, very good site!
Hi, yeah this post is really pleasant and I have learned lot of things from it regarding blogging. thanks.
Inspiring quest there. What occurred after? Thanks!
I am extremely inspired with your writing skills and alsowell as with the format on your blog. Is this a paid subject or did you customize it yourself? Either way stay up the nice quality writing, it’s rare to see a nice blog like this one nowadays..
I all the time used to read article in news papers but now as I am a user of web thus from now I am using net for articles, thanks to web.
I have read so many articles or reviews concerning the blogger lovers but this article is truly a pleasant post, keep it up.
Hiya very nice website!! Guy .. Beautiful .. Superb .. I will bookmark your blog and take the feeds also? I am satisfied to seek out so many useful information here in the publish, we’d like develop more strategies in this regard, thank you for sharing. . . . . .
Remarkable! Its really awesome post, I have got much clear idea concerning from this post.
Howdy! I know this is kinda off topic however I’d figured I’d ask. Would you be interested in exchanging links or maybe guest writing a blog article or vice-versa? My website addresses a lot of the same subjects as yours and I believe we could greatly benefit from each other. If you might be interested feel free to send me an e-mail. I look forward to hearing from you! Awesome blog by the way!
I will right away clutch your rss as I can not find your email subscription link or newsletter service. Do you have any? Please permit me understand so that I may subscribe. Thanks.
Because the admin of this site is working, no doubt very quickly it will be well-known, due to its quality contents.
Have you ever considered about including a little bit more than just your articles? I mean, what you say is valuable and all. Nevertheless think of if you added some great pictures or video clips to give your posts more, “pop”! Your content is excellent but with images and clips, this website could undeniably be one of the most beneficial in its niche. Very good blog!
I like it when folks come together and share opinions. Great blog, continue the good work!
Great web site you have here.. It’s hard to find high-quality writing like yours these days. I seriously appreciate people like you! Take care!!
It is perfect time to make some plans for the future and it is time to be happy. I have read this post and if I could I wish to suggest you few interesting things or suggestions. Perhaps you could write next articles referring to this article. I want to read more things about it!
Hi, i think that i saw you visited my website so i came to return the favor.I am trying to find things to improve my website!I suppose its ok to use some of your ideas!!
Hi there! I’m at work browsing your blog from my new iphone 3gs! Just wanted to say I love reading your blog and look forward to all your posts! Keep up the great work!
Currently it sounds like Expression Engine is the top blogging platform out there right now. (from what I’ve read) Is that what you’re using on your blog?
This is a great tip especially to those new to the blogosphere. Short but very accurate information Thank you for sharing this one. A must read article!
You really make it seem so easy together with your presentation however I in finding this topic to be really something which I think I would never understand. It sort of feels too complicated and very vast for me. I am looking forward in your next publish, I will try to get the hold of it!
Awesome things here. I’m very satisfied to see your article. Thank you so much and I’m taking a look forward to touch you. Will you please drop me a mail?
My brother suggested I might like this blog. He was totally right. This post actually made my day. You cann’t imagine just how much time I had spent for this information! Thanks!
a Emission probabilities of ten epigenetic states trained by an HMM model on five histones cialis for sale
Does your website have a contact page? I’m having a tough time locating it but, I’d like to send you an e-mail. I’ve got some recommendations for your blog you might be interested in hearing. Either way, great site and I look forward to seeing it expand over time.
Hi, i think that i saw you visited my weblog so i came to return the favor.I am trying to find things to improve my website!I suppose its ok to use some of your ideas!!
I am regular reader, how are you everybody? This piece of writing posted at this site is really nice.
Incredible points. Solid arguments. Keep up the amazing work.
Register at Highway Casino for 80 free spins without deposits! Please enter the bonus code HYPERSPINE if it works. A huge bonus of 255% plus 100 bonus spins. Get 88 No Deposit Spins Strictly 16 + Welcome bonuses are limited to the new players. One for every home and IP. A general agreement applies to all this. 21 Casino provides new players with free 50 No-Deposit Spins at Book of Dead Slots immediately with a registration fee of 121% for first deposit up to €200. What about top casino games and recurring bonuses? The rewards offers continue at 21 Casino! Visit 21 Casinos! But what if we told you there was a way to start playing without having to part with any of your hard-earned cash? This is where a no deposit bonus comes in. Specifically, a free spins no deposit bonus is usually offered to new players as a welcome bonus. This bonus allows you to start playing casino games without having to make a deposit, giving you the chance to find out more about an online casino site before risking your money.
http://topdogs1.co.kr/bbs/board.php?bo_table=free&wr_id=140196
Join Winorama and get a €7 no deposit bonus! Use your free spins on online slots or scratch card games. Play via tablet, smartphone & computer. We have carefully reviewed Winorama Casino and gave it a Very good reputation rating. Winorama Casino is a very good option to choose. As long as you only claim offers players from your country are eligible for, you should not face any serious issues after taking advantage of bonus offers from this casino. New players at Winorama Casino can take advantage of a free cash no deposit bonus worth €7. Like with all no deposit bonuses, players do not have to deposit money into their account to activate this offer. For anyone visiting Winorama, they will come face to face with slots, scratch cards, bingo and instant games – all with a fun and casual feel. Before playing, it’s possible to get a head-start with the aid of a Winorama Casino no deposit offer and other supportive perks.
I don’t even know how I ended up here, but I thought this post was good. I don’t know who you are but definitely you are going to a famous blogger if you are not already 😉 Cheers!
Hello! This post couldn’t be written any better! Reading this post reminds me of my good old room mate! He always kept talking about this. I will forward this post to him. Pretty sure he will have a good read. Thanks for sharing!
Everything is very open with a precise explanation of the issues. It was really informative. Your website is very helpful. Thank you for sharing!
Thank you for sharing your info. I truly appreciate your efforts and I am waiting for your next post thank you once again.
Hi, i think that i saw you visited my web site so i came to return the favor.I am trying to find things to improve my website!I suppose its ok to use some of your ideas!!
Hey There. I found your blog using msn. This is an extremely well written article. I will be sure to bookmark it and come back to read more of your useful information. Thanks for the post. I will definitely comeback.
Yes! Finally something about %keyword1%.
Greetings from Colorado! I’m bored to death at work so I decided to check out your site on my iphone during lunch break. I really like the knowledge you present here and can’t wait to take a look when I get home. I’m amazed at how quick your blog loaded on my cell phone .. I’m not even using WIFI, just 3G .. Anyhow, wonderful site!
Link exchange is nothing else but it is simply placing the other person’s weblog link on your page at appropriate place and other person will also do same for you.
Hey very interesting blog!
Pretty great post. I simply stumbled upon your blog and wanted to mention that I have really enjoyed browsing your blog posts. In any case I’ll be subscribing in your feed and I am hoping you write again soon!
Please let me know if you’re looking for a article writer for your weblog. You have some really great posts and I believe I would be a good asset. If you ever want to take some of the load off, I’d really like to write some material for your blog in exchange for a link back to mine. Please send me an e-mail if interested. Regards!
Awesome things here. I’m very satisfied to see your article. Thank you so much and I’m taking a look forward to touch you. Will you please drop me a mail?
Hey there! Do you use Twitter? I’d like to follow you if that would be ok. I’m undoubtedly enjoying your blog and look forward to new updates.
I’d like to find out more? I’d like to find out more details.
Heya i’m for the first time here. I came across this board and I find It truly useful & it helped me out a lot. I hope to give something back and help others like you helped me.
Have you ever considered about including a little bit more than just your articles? I mean, what you say is valuable and all. Nevertheless think about if you added some great pictures or video clips to give your posts more, “pop”! Your content is excellent but with images and video clips, this site could certainly be one of the very best in its niche. Excellent blog!
Hello there! This post couldn’t be written any better! Looking at this post reminds me of my previous roommate! He constantly kept talking about this. I will forward this article to him. Pretty sure he’ll have a good read. Many thanks for sharing!
This piece of writing gives clear idea designed for the new viewers of blogging, that in fact how to do blogging and site-building.
539
《539彩券:台灣的小確幸》
哎呀,說到台灣的彩券遊戲,你怎麼可能不知道539彩券呢?每次”539開獎”,都有那麼多人緊張地盯著螢幕,心想:「這次會不會輪到我?」。
### 539彩券,那是什麼來頭?
嘿,539彩券可不是昨天才有的新鮮事,它在台灣已經陪伴了我們好多年了。簡單的玩法,小小的投注,卻有著不小的期待,難怪它這麼受歡迎。
### 539開獎,是場視覺盛宴!
每次”539開獎”,都像是一場小型的節目。專業的主持人、明亮的燈光,還有那台專業的抽獎機器,每次都帶給我們不小的刺激。
### 跟我一起玩539?
想玩539?超簡單!走到街上,找個彩券行,選五個你喜歡的號碼,買下來就對了。當然,現在科技這麼發達,坐在家裡也能買,多方便!
### 539開獎,那刺激的感覺!
每次”539開獎”,真的是讓人既期待又緊張。想像一下,如果這次中了,是不是可以去吃那家一直想去但又覺得太貴的餐廳?
### 最後說兩句
539彩券,真的是個小確幸。但嘿,玩彩券也要有度,別太沉迷哦!希望每次”539開獎”,都能帶給你一點點的驚喜和快樂。
Быстровозводимые строения – это современные здания, которые различаются большой скоростью строительства и мобильностью. Они представляют собой конструкции, состоящие из предварительно изготовленных элементов либо блоков, которые способны быть быстро установлены на районе строительства.
[url=https://bystrovozvodimye-zdanija.ru/]Строительство каркасных зданий[/url] владеют гибкостью а также адаптируемостью, что дозволяет легко изменять а также трансформировать их в соответствии с потребностями клиента. Это экономически эффективное и экологически стойкое решение, которое в последние лета заполучило маштабное распространение.
Hi there, after reading this awesome piece of writing i am too glad to share my experience here with mates.
Its like you read my mind! You seem to know so much about this, like you wrote the book in it or something. I think that you could do with some pics to drive the message home a bit, but other than that, this is fantastic blog. A great read. I’ll definitely be back.
I loved as much as you will receive carried out right here. The sketch is tasteful, your authored subject matter stylish. nonetheless, you command get bought an impatience over that you wish be delivering the following. unwell unquestionably come further formerly again since exactly the same nearly a lot often inside case you shield this increase.
I am really thankful to the owner of this website who has shared this great article at here.
Hello! Someone in my Myspace group shared this site with us so I came to give it a look. I’m definitely enjoying the information. I’m book-marking and will be tweeting this to my followers! Exceptional blog and brilliant style and design.
Thank you for the auspicious writeup. It in reality was a amusement account it. Glance complicated to far brought agreeable from you! By the way, how can we communicate?
I visited multiple web pages except the audio quality for audio songs current at this site is in fact fabulous.
I am regular reader, how are you everybody? This post posted at this web site is truly pleasant.
We stumbled over here coming from a different web page and thought I may as well check things out. I like what I see so now i’m following you. Look forward to checking out your web page for a second time.
Currently it seems like Movable Type is the best blogging platform out there right now. (from what I’ve read) Is that what you’re using on your blog?
Hi there, all is going perfectly here and ofcourse every one is sharing information, that’s in fact good, keep up writing.
Greate article. Keep writing such kind of information on your page. Im really impressed by your site.
Interesting blog! Is your theme custom made or did you download it from somewhere? A design like yours with a few simple adjustements would really make my blog jump out. Please let me know where you got your design. Bless you
Pretty nice post. I just stumbled upon your blog and wanted to say that I have really enjoyed browsing your blog posts. In any case I’ll be subscribing to your feed and I hope you write again soon!
Quality posts is the important to attract the viewers to pay a visit the web site, that’s what this website is providing.
I always used to read piece of writing in news papers but now as I am a user of internet thus from now I am using net for articles or reviews, thanks to web.
Hurrah! Finally I got a website from where I be able to truly take helpful information regarding my study and knowledge.
I’d like to find out more? I’d love to find out more details.
Hi there, i read your blog occasionally and i own a similar one and i was just wondering if you get a lot of spam responses? If so how do you stop it, any plugin or anything you can suggest? I get so much lately it’s driving me insane so any assistance is very much appreciated.
Thanks for sharing such a nice thought, piece of writing is good, thats why i have read it fully
Hi! This is my 1st comment here so I just wanted to give a quick shout out and tell you I genuinely enjoy reading through your articles. Can you suggest any other blogs/websites/forums that deal with the same subjects? Many thanks!
I am in fact thankful to the owner of this site who has shared this wonderful article at here.
When I originally commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment is added I get three emails with the same comment. Is there any way you can remove me from that service? Bless you!
It’s awesome to visit this website and reading the views of all friends about this post, while I am also eager of getting experience.
I was very pleased to discover this great site. I want to to thank you for your time for this wonderful read!! I definitely liked every bit of it and I have you saved as a favorite to see new things on your website.
Pretty! This was an extremely wonderful post. Thank you for providing this info.
Piece of writing writing is also a fun, if you be acquainted with after that you can write otherwise it is difficult to write.
If some one wants to be updated with most up-to-date technologies after that he must be pay a visit this web site and be up to date everyday.
Heya i’m for the primary time here. I came across this board and I find It truly useful & it helped me out a lot. I am hoping to provide something back and help others like you helped me.
If you desire to take a great deal from this article then you have to apply such strategies to your won webpage.
Greate article. Keep writing such kind of information on your page. Im really impressed by your site.
It’s enormous that you are getting ideas from this piece of writing as well as from our discussion made at this place.
Thanks for one’s marvelous posting! I really enjoyed reading it, you are a great author. I will make sure to bookmark your blog and will eventually come back someday. I want to encourage that you continue your great posts, have a nice holiday weekend!
Hello! Do you use Twitter? I’d like to follow you if that would be ok. I’m undoubtedly enjoying your blog and look forward to new updates.
Hi there, all the time i used to check weblog posts here early in the break of day, as i like to learn more and more.
Hey there! I’m at work browsing your blog from my new iphone! Just wanted to say I love reading your blog and look forward to all your posts! Keep up the fantastic work!
I know this if off topic but I’m looking into starting my own blog and was wondering what all is required to get set up? I’m assuming having a blog like yours would cost a pretty penny? I’m not very internet savvy so I’m not 100% sure. Any recommendations or advice would be greatly appreciated. Thank you
Hello! Do you use Twitter? I’d like to follow you if that would be ok. I’m undoubtedly enjoying your blog and look forward to new updates.
Excellent site you have here but I was curious about if you knew of any community forums that cover the same topics talked about in this article? I’d really love to be a part of group where I can get advice from other knowledgeable individuals that share the same interest. If you have any recommendations, please let me know. Kudos!
Do you have a spam issue on this website; I also am a blogger, and I was wanting to know your situation; many of us have created some nice methods and we are looking to swap methods with other folks, be sure to shoot me an e-mail if interested.
Great delivery. Solid arguments. Keep up the amazing work.
It’s awesome designed for me to have a web site, which is helpful for my experience. thanks admin
Undeniably believe that which you stated. Your favorite justification appeared to be on the internet the simplest thing to be aware of. I say to you, I definitely get irked while people consider worries that they plainly do not know about. You managed to hit the nail upon the top and also defined out the whole thing without having side effect , people can take a signal. Will likely be back to get more. Thanks
Hi! I’m at work browsing your blog from my new iphone 4! Just wanted to say I love reading your blog and look forward to all your posts! Keep up the great work!
We are a group of volunteers and starting a new scheme in our community. Your site provided us with valuable information to work on. You have done an impressive job and our whole community will be grateful to you.
Appreciate the recommendation. Will try it out.
Wonderful goods from you, man. I’ve consider your stuff prior to and you’re simply too wonderful. I really like what you’ve obtained here, really like what you’re stating and the way through which you assert it. You make it entertaining and you still take care of to stay it smart. I cant wait to read far more from you. This is actually a terrific website.
I am extremely impressed with your writing skills and also with the layout on your blog. Is this a paid theme or did you customize it yourself? Either way keep up the nice quality writing, it’s rare to see a nice blog like this one these days.
Hi there I am so glad I found your blog page, I really found you by error, while I was searching on Aol for something else, Regardless I am here now and would just like to say kudos for a remarkable post and a all round interesting blog (I also love the theme/design), I don’t have time to read through it all at the minute but I have saved it and also added in your RSS feeds, so when I have time I will be back to read a lot more, Please do keep up the superb job.
Excellent post. I was checking continuously this blog and I am impressed! Very useful information specially the last part 🙂 I care for such info a lot. I was seeking this particular info for a long time. Thank you and good luck.
Thanks for ones marvelous posting! I genuinely enjoyed reading it, you may be a great author. I will always bookmark your blog and will come back someday. I want to encourage one to continue your great job, have a nice day!
Spot on with this write-up, I honestly believe this website needs far more attention. I’ll probably be back again to read through more, thanks for the information!
A fascinating discussion is worth comment. I believe that you ought to write more on this topic, it might not be a taboo subject but usually people don’t discuss such topics. To the next! Many thanks!!
Hi there everyone, it’s my first pay a visit at this website, and piece of writing is in fact fruitful in favor of me, keep up posting these articles.
Thanks for your personal marvelous posting! I quite enjoyed reading it, you’re a great author. I will make certain to bookmark your blog and will often come back in the future. I want to encourage one to continue your great writing, have a nice morning!
After looking over a few of the blog posts on your web site, I honestly like your way of blogging. I bookmarked it to my bookmark website list and will be checking back soon. Take a look at my web site as well and let me know what you think.
It’s in reality a nice and helpful piece of information. I’m satisfied that you shared this helpful info with us. Please stay us informed like this. Thanks for sharing.
Hi! Someone in my Myspace group shared this site with us so I came to take a look. I’m definitely enjoying the information. I’m book-marking and will be tweeting this to my followers! Wonderful blog and outstanding design and style.
What i do not realize is if truth be told how you’re now not really a lot more smartly-favored than you may be right now. You are so intelligent. You understand therefore significantly when it comes to this matter, produced me personally consider it from so many numerous angles. Its like men and women don’t seem to be interested unless it’s something to accomplish with Woman gaga! Your personal stuffs excellent. All the time care for it up!
Heya i’m for the primary time here. I came across this board and I find It truly useful & it helped me out a lot. I hope to provide something back and help others like you helped me.
Hi to all, how is all, I think every one is getting more from this web site, and your views are pleasant designed for new viewers.
Hello! Do you know if they make any plugins to protect against hackers? I’m kinda paranoid about losing everything I’ve worked hard on. Any recommendations?
Hey there! I could have sworn I’ve been to this blog before but after browsing through some of the post I realized it’s new to me. Nonetheless, I’m definitely happy I found it and I’ll be bookmarking and checking back often!
I enjoy, cause I found exactly what I used to be taking a look for. You have ended my 4 day long hunt! God Bless you man. Have a nice day. Bye
Hmm it seems like your site ate my first comment (it was extremely long) so I guess I’ll just sum it up what I had written and say, I’m thoroughly enjoying your blog. I as well am an aspiring blog blogger but I’m still new to the whole thing. Do you have any recommendations for inexperienced blog writers? I’d definitely appreciate it.
This web site really has all of the information I wanted about this subject and didn’t know who to ask.
This article is in fact a pleasant one it helps new internet people, who are wishing for blogging.
Oh my goodness! Amazing article dude! Thanks, However I am experiencing problems with your RSS. I don’t know why I can’t subscribe to it. Is there anybody else getting the same RSS problems? Anyone who knows the solution will you kindly respond? Thanx!!
I seriously love your site.. Excellent colors & theme. Did you develop this site yourself? Please reply back as I’m trying to create my own blog and would like to learn where you got this from or exactly what the theme is called. Thanks!
Hi there, after reading this remarkable article i am also cheerful to share my knowledge here with friends.
Hi, I do believe this is an excellent blog. I stumbledupon it 😉 I’m going to come back once again since I bookmarked it. Money and freedom is the best way to change, may you be rich and continue to help other people.
Thank you a bunch for sharing this with all folks you really recognize what you are talking approximately! Bookmarked. Please also talk over with my site =). We will have a link change agreement among us
I’m impressed, I must say. Rarely do I encounter a blog that’s equally educative and interesting, and let me tell you, you have hit the nail on the head. The issue is something that not enough people are speaking intelligently about. I’m very happy that I found this in my search for something concerning this.
What’s up to every body, it’s my first visit of this weblog; this weblog consists of awesome and actually good information for readers.
Hey There. I found your blog the use of msn. This is a very well written article. I will be sure to bookmark it and come back to read more of your useful information. Thank you for the post. I will definitely comeback.
Hi there, I check your new stuff regularly. Your writing style is awesome, keep doing what you’re doing!
I am actually glad to read this blog posts which includes lots of helpful data, thanks for providing such information.
obviously like your web-site however you need to check the spelling on quite a few of your posts. A number of them are rife with spelling problems and I in finding it very bothersome to tell the truth then again I will surely come back again.
constantly i used to read smaller articles or reviews which also clear their motive, and that is also happening with this piece of writing which I am reading here.
If you want to get a great deal from this piece of writing then you have to apply such strategies to your won weblog.
This text is invaluable. How can I find out more?
What’s up, after reading this remarkable article i am too glad to share my experience here with friends.
Hello! This post couldn’t be written any better! Reading this post reminds me of my old room mate! He always kept talking about this. I will forward this post to him. Pretty sure he will have a good read. Thank you for sharing!
Your style is really unique compared to other people I have read stuff from. Thanks for posting when you have the opportunity, Guess I will just bookmark this site.
I have been surfing online more than three hours these days, yet I never found any fascinating article like yours. It’s pretty value enough for me. Personally, if all webmasters and bloggers made good content as you did, the net will probably be much more useful than ever before.
I simply could not leave your web site prior to suggesting that I really enjoyed the standard information a person supply for your visitors? Is going to be back regularly in order to check out new posts
I like the valuable information you provide in your articles. I will bookmark your weblog and check again here frequently. I am quite certain I will learn lots of new stuff right here! Good luck for the next!
Fabulous, what a blog it is! This website gives useful information to us, keep it up.
I’m now not positive where you are getting your info, however good topic. I needs to spend a while learning more or working out more. Thank you for great information I used to be on the lookout for this information for my mission.
Your style is so unique compared to other people I have read stuff from. Thanks for posting when you have the opportunity, Guess I will just bookmark this web site.
I was wondering if you ever considered changing the layout of your site? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having one or two images. Maybe you could space it out better?
Great post.
A person necessarily help to make critically articles I might state. This is the first time I frequented your web page and to this point? I amazed with the research you made to create this actual submit amazing. Magnificent activity!
I do consider all the ideas you have presented for your post. They are very convincing and will definitely work. Still, the posts are too brief for newbies. May you please extend them a bit from next time? Thank you for the post.
Really no matter if someone doesn’t know after that its up to other users that they will help, so here it occurs.
I for all time emailed this blog post page to all my friends, because if like to read it next my friends will too.
You’re so awesome! I don’t suppose I have read something like this before. So good to find somebody with some unique thoughts on this subject. Really.. thanks for starting this up. This website is something that’s needed on the web, someone with some originality!
Greetings from Florida! I’m bored to death at work so I decided to check out your site on my iphone during lunch break. I enjoy the info you present here and can’t wait to take a look when I get home. I’m amazed at how quick your blog loaded on my cell phone .. I’m not even using WIFI, just 3G .. Anyhow, very good site!
Hey there, I think your website might be having browser compatibility issues. When I look at your blog site in Ie, it looks fine but when opening in Internet Explorer, it has some overlapping. I just wanted to give you a quick heads up! Other then that, amazing blog!
Pretty nice post. I just stumbled upon your blog and wanted to say that I have really enjoyed browsing your blog posts. In any case I’ll be subscribing to your feed and I hope you write again soon!
I love your blog.. very nice colors & theme. Did you design this website yourself or did you hire someone to do it for you? Plz reply as I’m looking to design my own blog and would like to know where u got this from. kudos
Hmm it seems like your site ate my first comment (it was extremely long) so I guess I’ll just sum it up what I submitted and say, I’m thoroughly enjoying your blog. I as well am an aspiring blog blogger but I’m still new to the whole thing. Do you have any tips and hints for beginner blog writers? I’d genuinely appreciate it.
Great info. Lucky me I ran across your website by accident (stumbleupon). I have book-marked it for later!
Hi to every body, it’s my first visit of this webpage; this webpage contains awesome and actually fine information for readers.
Hey There. I found your blog using msn. This is a very well written article. I will be sure to bookmark it and come back to read more of your useful information. Thanks for the post. I will definitely comeback.
As the admin of this site is working, no doubt very rapidly it will be well-known, due to its quality contents.
You really make it seem so easy with your presentation however I find this topic to be really something which I feel I would never understand. It sort of feels too complicated and very wide for me. I am looking forward in your next post, I will try to get the grasp of it!
Hello there! This post couldn’t be written any better! Reading through this post reminds me of my previous roommate! He always kept talking about this. I am going to forward this information to him. Pretty sure he will have a good read. Thanks for sharing!
Greetings! I know this is kinda off topic however I’d figured I’d ask. Would you be interested in exchanging links or maybe guest writing a blog article or vice-versa? My site addresses a lot of the same subjects as yours and I believe we could greatly benefit from each other. If you might be interested feel free to send me an e-mail. I look forward to hearing from you! Wonderful blog by the way!
Быстромонтажные здания: коммерческий результат в каждой детали!
В современной реальности, где время имеет значение, экспресс-конструкции стали решением, спасающим для предпринимательства. Эти прогрессивные сооружения обладают надежность, экономичность и быстроту установки, что позволяет им лучшим выбором для разных коммерческих начинаний.
[url=https://bystrovozvodimye-zdanija-moskva.ru/]Быстровозводимые здания[/url]
1. Скорость строительства: Часы – ключевой момент в коммерции, и экспресс-сооружения позволяют существенно сократить время монтажа. Это чрезвычайно полезно в случаях, когда необходимо оперативно начать предпринимательскую деятельность и начать прибыльное ведение бизнеса.
2. Экономичность: За счет оптимизации производства и установки элементов на месте, стоимость быстровозводимых зданий часто уменьшается, по отношению к обычным строительным проектам. Это предоставляет шанс сократить издержки и обеспечить более высокий доход с инвестиций.
Подробнее на [url=https://xn--73-6kchjy.xn--p1ai/]http://scholding.ru[/url]
В заключение, моментальные сооружения – это великолепное решение для предпринимательских задач. Они включают в себя быстрое строительство, экономичность и надежные характеристики, что позволяет им лучшим выбором для предпринимателей, ориентированных на оперативный бизнес-старт и извлекать прибыль. Не упустите шанс экономии времени и денег, выбрав быстровозводимые здания для вашей будущей задачи!
I visited multiple web sites except the audio quality for audio songs present at this site is really fabulous.
Моментально возводимые здания: финансовая польза в каждом кирпиче!
В нынешней эпохе, где время имеет значение, объекты быстрого возвода стали настоящим спасением для бизнеса. Эти прогрессивные сооружения сочетают в себе твердость, финансовую эффективность и скорость монтажа, что делает их оптимальным решением для разнообразных предпринимательских инициатив.
[url=https://bystrovozvodimye-zdanija-moskva.ru/]Быстровозводимые здания[/url]
1. Скорость строительства: Время – это самый важный ресурс в коммерческой деятельности, и быстровозводимые здания способствуют значительному сокращению сроков возведения. Это особенно выгодно в постановках, когда важно быстро начать вести бизнес и начать извлекать прибыль.
2. Экономичность: За счет оптимизации производства и установки элементов на месте, бюджет на сооружения быстрого монтажа часто бывает ниже, по отношению к традиционным строительным проектам. Это обеспечивает экономию средств и получить лучшую инвестиционную отдачу.
Подробнее на [url=https://xn--73-6kchjy.xn--p1ai/]scholding.ru[/url]
В заключение, моментальные сооружения – это великолепное решение для бизнес-проектов. Они объединяют в себе скорость строительства, финансовую выгоду и твердость, что обуславливает их отличным выбором для предпринимательских начинаний, ориентированных на оперативный бизнес-старт и извлекать прибыль. Не упустите возможность сократить издержки и сэкономить время, наилучшие объекты быстрого возвода для ваших будущих инициатив!
Asking questions are truly nice thing if you are not understanding anything entirely, except this article offers nice understanding even.
An interesting discussion is worth comment. I think that you should write more on this subject, it might not be a taboo subject but generally people do not discuss such topics. To the next! Kind regards!!
It’s remarkable for me to have a web site, which is helpful designed for my knowledge. thanks admin
Wonderful beat ! I wish to apprentice whilst you amend your web site, how can i subscribe for a blog site? The account aided me a appropriate deal. I were tiny bit familiar of this your broadcast provided bright transparent concept
It’s a shame you don’t have a donate button! I’d without a doubt donate to this fantastic blog! I suppose for now i’ll settle for book-marking and adding your RSS feed to my Google account. I look forward to brand new updates and will talk about this blog with my Facebook group. Chat soon!
Hi there! I could have sworn I’ve been to this web site before but after browsing through some of the posts I realized it’s new to me. Anyhow, I’m definitely pleased I discovered it and I’ll be bookmarking it and checking back regularly!
Whats up this is somewhat of off topic but I was wondering if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding skills so I wanted to get advice from someone with experience. Any help would be greatly appreciated!
What’s up, yup this piece of writing is truly nice and I have learned lot of things from it concerning blogging. thanks.
Howdy would you mind stating which blog platform you’re working with? I’m looking to start my own blog in the near future but I’m having a difficult time making a decision between BlogEngine/Wordpress/B2evolution and Drupal. The reason I ask is because your design and style seems different then most blogs and I’m looking for something completely unique. P.S My apologies for getting off-topic but I had to ask!
Yes! Finally something about %keyword1%.
Hey I am so glad I found your webpage, I really found you by error, while I was searching on Google for something else, Nonetheless I am here now and would just like to say thanks a lot for a remarkable post and a all round enjoyable blog (I also love the theme/design), I dont have time to read through it all at the minute but I have book-marked it and also added in your RSS feeds, so when I have time I will be back to read a great deal more, Please do keep up the fantastic b.
This is a topic that’s close to my heart… Take care! Where are your contact details though?
It’s awesome to pay a visit this web site and reading the views of all mates concerning this article, while I am also keen of getting knowledge.
In September, Bitcoin officially became a legal tender in El Salvador with many news sources wondering what countries would be next. Traders and investors use our platform. Founded in June 2020 and based in Hong Kong, Topcredit Exchange’s team primarily comes from traditional financial backgrounds, understanding the core demands of asset management for users and recognizing trading as a vital tool for efficient asset management and returns. From the outset, Topcredit Exchange has been committed to providing users with a secure, convenient, and efficient asset management tool. After successfully operating in the regional market, serving 1.2 million users securely for three years, Topcredit Int officially launched its deep global expansion strategy in June 2023. !\ Don’t confuse this with the coinmarketcap package.
http://www.perdormire.co.kr/bbs/board.php?bo_table=free&wr_id=153925
If you suspect a site is fake, get in touch. HaasOnline is one of the oldest and well-respected crypto trading bot platforms available. You can manage automated trading on over 37 exchanges. Create bot strategies with a click of a mouse or develop your trade bot line-by-line. Even if you are fine by guessing a private key to a random wallet out of a few million the amount of tries to do is not that much different in absolute terms and the reasoning still applies. I’d definitely add Flint Wallet into the Mix, they got a good team behind that wallet. The foundation of the crypto Stellar has invested in MoneyGram The foundation of the crypto Stellar has invested in MoneyGram Convenience: XcelPay Wallet is a convenient crypto wallet that is easy to use and accessible from every part of the world.Affordability: XcelPay Wallet is an affordable wallet that is free to download and use both on App Store and Play Store.Support: The ecosystem provides 24*7 support services.
I will right away seize your rss as I can not in finding your email subscription link or newsletter service. Do you have any? Please allow me understand so that I may just subscribe. Thanks.
What’s up friends, how is all, and what you want to say concerning this post, in my view its actually remarkable in favor of me.
First off I want to say great blog! I had a quick question that I’d like to ask if you don’t mind. I was curious to know how you center yourself and clear your thoughts before writing. I have had a tough time clearing my mind in getting my thoughts out. I do enjoy writing but it just seems like the first 10 to 15 minutes are wasted just trying to figure out how to begin. Any ideas or tips? Thanks!
I was wondering if you ever considered changing the layout of your site? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having one or two images. Maybe you could space it out better?
Post writing is also a fun, if you be acquainted with after that you can write or else it is complex to write.
Hi, i think that i saw you visited my web site so i got here to go back the favor?.I am trying to in finding things to improve my website!I guess its ok to use some of your ideas!!
I couldn’t resist commenting. Very well written!
Hi there, all the time i used to check website posts here early in the dawn, as i love to learn more and more.
You can email the site owner to let them know you were blocked. Please include what you were doing when this page came up and the Cloudflare Ray ID found at the bottom of this page. Learn more about troubleshooting WordPress. Check out table below for cool starburst free spins no deposit bonuses: You will still find Canadian casinos that require you to activate your no deposit bonus or free spins using a bonus code. This can be done in a special box on the registration form or directly in your casino account. A bonus code is a letter-number combination that works similar to a voucher. As soon as you enter the correct code, the no deposit bonus is available to you. If a bonus code for one of the NetEnt casinos is required, you will receive it directly in the bonus offer.
https://www.reverbnation.com/artist/richardryann
The player from Australia is inquiring about website accessibility. We rejected the complaint because the player didn’t respond to our messages and questions. To ensure quick payouts, you have to submit to Johnny Ka$h Casino copies of your identification documents. You can upload these documents on the casino website. Since Johnny Ka$h Casino stores your documents on secure servers and makes them available only to senior security staff, you can rest assured that they are safe. Johnny Kash Casino has been closed and no longer operates. I will try to contact the casino to give us further explanation. The FAQ section of the casino answers the security-related King Johnnie casino questions in detail. You will find answers to account information, the steps for account verification, and much more.
Нужна стяжка пола в Москве, но вы не знаете, как выбрать подрядчика? Обращайтесь к нам на сайт styazhka-pola24.ru! Мы предлагаем услуги по устройству стяжки пола любой площади и сложности, а также гарантируем быстрое и качественное выполнение работ.
Нужна стяжка пола в Москве, но вы не знаете, как выбрать подрядчика? Обратитесь к нам на сайт styazhka-pola24.ru! Мы предлагаем услуги по устройству стяжки пола любой площади и сложности, а также гарантируем быстрое и качественное выполнение работ.
Хотите заказать стяжку пола в Москве, но не знаете, где искать надежного подрядчика? Обратитесь к нам на сайт styazhka-pola24.ru! Мы предоставляем услуги по устройству стяжки пола м2 по доступной стоимости, а также устройству стяжки пола под ключ.
снабжение объектов стройматериалами
Ищете надежного подрядчика для устройства стяжки пола в Москве? Обратитесь к нам на сайт styazhka-pola24.ru! Мы предлагаем услуги по залитию стяжки пола любой сложности и площади, а также гарантируем высокое качество работ.
Ищете надежного подрядчика для устройства стяжки пола в Москве? Обращайтесь к нам на сайт styazhka-pola24.ru! Мы предлагаем услуги по залитию стяжки пола любой сложности и площади, а также гарантируем быстрое и качественное выполнение работ.
снабжение строительными материалами строительного объекта
снабжение строительных компаний
Хотите получить идеально ровный пол без лишних затрат? Обратитесь к профессионалам на сайте styazhka-pola24.ru! Мы предоставляем услуги по стяжке пола м2 по доступной стоимости, а также устройству стяжки пола под ключ в Москве и области.
снабжение объектов строительства
Ищете надежного подрядчика для устройства стяжки пола в Москве? Обратитесь к нам на сайт styazhka-pola24.ru! Мы предлагаем услуги по залитию стяжки пола любой сложности и площади, а также гарантируем высокое качество работ.
поставка строительных материалов ооо
производство поставки строительных материалов
Нужная услуга для идеальной отделки интерьера- это механизированная штукатурка стен. На mehanizirovannaya-shtukaturka-moscow.ru предлагаются только самые качественные услуги.
Хотите получить идеально ровные стены в своем доме или офисе? Обратитесь к профессионалам на сайте mehanizirovannaya-shtukaturka-moscow.ru! Мы предлагаем услуги по механизированной штукатурке стен любой сложности и площади, а также гарантируем качество работ и доступные цены.
Современный рынок предлагает нам множество уникальных решений, включая штукатурку механизированную. Проверьте mehanizirovannaya-shtukaturka-moscow.ru для получения подробной информации.
Нужна машинная штукатурка стен в Москве, но вы не знаете, какой подрядчик лучше выбрать? Обратитесь к нам на сайт mehanizirovannaya-shtukaturka-moscow.ru! Мы предоставляем услуги по механизированной штукатурке стен любой площади и сложности, а также гарантируем качество и надежность.
Hi my family member! I want to say that this article is awesome, great written and come with almost all significant infos. I’d like to peer more posts like this .
What’s up i am kavin, its my first time to commenting anywhere, when i read this post i thought i could also make comment due to this sensible post.
If some one wants to be updated with most recent technologies after that he must be go to see this website and be up to date daily.
I think what you postedtypedsaidthink what you postedtypedbelieve what you postedtypedbelieve what you postedtypedsaidWhat you postedtyped was very logicala bunch of sense. But, what about this?think about this, what if you were to write a killer headlinetitle?content?typed a catchier title? I ain’t saying your content isn’t good.ain’t saying your content isn’t gooddon’t want to tell you how to run your blog, but what if you added a titleheadlinetitle that grabbed people’s attention?maybe get people’s attention?want more? I mean %BLOG_TITLE% is a little vanilla. You ought to look at Yahoo’s home page and watch how they createwrite post headlines to get viewers interested. You might add a related video or a related picture or two to get readers interested about what you’ve written. Just my opinion, it might bring your postsblog a little livelier.
buy viagra and cialis online Bruce Lipton s video The Biology of Belief and I learned about epigenetics
I like what you guys are up too. Such clever work and exposure! Keep up the very good works guys I’ve added you guys to blogroll.
Ищете решение для ремонта? Механизированная штукатурка с mehanizirovannaya-shtukaturka-moscow.ru – это быстро, качественно и без пыли.
This website definitely has all of the info I wanted about this subject and didn’t know who to ask.
Hi there, I found your web site by the use of Google whilst searching for a comparable topic, your site got here up, it appears good. I have bookmarked it in my google bookmarks.
I blog quite often and I genuinely appreciate your content. This article has really peaked my interest. I will book mark your website and keep checking for new information about once a week. I subscribed to your RSS feed as well.
My brother suggested I might like this website. He was totally right. This post actually made my day. You cann’t imagine just how much time I had spent for this information! Thanks!
Хотите получить идеально ровные стены в своей квартире или офисе? Обращайтесь к профессионалам на сайте mehanizirovannaya-shtukaturka-moscow.ru! Мы предоставляем услуги по механизированной штукатурке стен в Москве и области, а также гарантируем быстрое и качественное выполнение работ.
I know this if off topic but I’m looking into starting my own blog and was wondering what all is required to get set up? I’m assuming having a blog like yours would cost a pretty penny? I’m not very internet savvy so I’m not 100% positive. Any tips or advice would be greatly appreciated. Appreciate it
Good way of explaining, and pleasant piece of writing to get information about my presentation subject matter, which i am going to convey in college.
Получите безупречные стены благодаря услуге штукатурка стен на mehanizirovannaya-shtukaturka-moscow.ru. Качество и скорость исполнения вас удивят.
This is my first time visit at here and i am really happy to read all at one place.
Хотите получить идеально ровные стены без лишних затрат? Обратитесь к профессионалам на сайте mehanizirovannaya-shtukaturka-moscow.ru! Мы предоставляем услуги по машинной штукатурке стен по доступной стоимости, а также гарантируем устройство штукатурки по маякам стен.
Wow that was strange. I just wrote an extremely long comment but after I clicked submit my comment didn’t show up. Grrrr… well I’m not writing all that over again. Regardless, just wanted to say superb blog!
My partner and I absolutely love your blog and find most of your post’s to be just what I’m looking for. Does one offer guest writers to write content to suit your needs? I wouldn’t mind publishing a post or elaborating on a lot of the subjects you write concerning here. Again, awesome weblog!
Thanks for one’s marvelous posting! I actually enjoyed reading it, you may be a great author. I will be sure to bookmark your blog and definitely will come back at some point. I want to encourage that you continue your great job, have a nice holiday weekend!
I do agree with all the concepts you have introduced for your post. They are very convincing and will definitely work. Still, the posts are too brief for newbies. May you please prolong them a bit from next time? Thank you for the post.
Howdy! Do you know if they make any plugins to protect against hackers? I’m kinda paranoid about losing everything I’ve worked hard on. Any recommendations?
This website was… how do I say it? Relevant!! Finally I have found something that helped me. Cheers!
Thank you for the auspicious writeup. It in fact was a amusement account it. Look advanced to far added agreeable from you! By the way, how can we communicate?
Wow, this article is pleasant, my sister is analyzing such things, so I am going to tell her.
I don’t even understand how I ended up here, however I assumed this submit used to be good. I don’t recognize who you’re however definitely you are going to a famous blogger in case you are not already. Cheers!
Hi, i think that i saw you visited my blog so i got here to go back the want?.I am trying to find things to improve my website!I guess its good enough to use some of your ideas!!
you are actually a good webmaster. The web site loading velocity is incredible. It kind of feels that you are doing any unique trick. Also, The contents are masterpiece. you have performed a great task in this topic!
Pretty nice post. I just stumbled upon your blog and wanted to say that I have really enjoyed browsing your blog posts. In any case I’ll be subscribing to your feed and I hope you write again soon!
Yes! Finally something about %keyword1%.
It’s remarkable to pay a visit this web site and reading the views of all friends concerning this post, while I am also eager of getting familiarity.
This site definitely has all of the information I wanted about this subject and didn’t know who to ask.
Keep this going please, great job!
Good day! Would you mind if I share your blog with my zynga group? There’s a lot of people that I think would really enjoy your content. Please let me know. Cheers
La primera criptomoneda fue Bitcoin. Dado que es de código abierto, es posible que otras personas usen la mayoría del código, realicen algunos cambios y luego lancen su propia moneda por separado. Mucha gente ha hecho exactamente esto. Algunas de estas monedas son muy similares a Bitcoin, con solo una o dos características modificadas (como Litecoin), mientras que otras son muy diferentes, con otros modelos de seguridad, emisión y gobernanza. Sin embargo, todas comparten el mismo nombre —cada moneda emitida después de Bitcoin se considera una altcoin. Las criptomonedas operan en un mercado diferente al de las acciones. Es por eso que su negociación está abierta las 24 horas del día, los 7 días de la semana. Criptomonedas en Argentina: pese a que en Argentina las divisas digitales no están legalizadas, su uso ha ido en aumento tras las décadas de inestabilidad financiera a la que los ciudadanos se han enfrentado, convirtiéndose en uno de los países latinoamericanos con mayor presencia de criptomonedas. Sobre esta línea, el presidente Alberto Fernández ha sugerido su uso para combatir la inflación.
https://xn--v52b2zd5t6jbib523m.com/bbs/board.php?bo_table=free&wr_id=808828
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt. El mercado de criptomonedas comenzó septiembre con una nota negativa, ya que siguió los pasos de la tendencia bajista de agosto. El creciente soporte ha hundido a las principales monedas digitales incluso a un nivel más bajo, con muchas de ellas alcanzando su soporte mensual o anual. Dogecoin (DOGE) se cotiza hoy en 0,06314 USD, con un valor alto de 0,063779 USD y un valor bajo de 0,062752 USD en las últimas 24 horas. En relación a la tendencia de los últimos siete días, el precio se ha mantenido con una caída de 0,11%. Fue entonces cuando se empezó a hablar del “criptoinvierno”, como apunta el medio especializado NextAdvisor, un concepto que se refiere a la baja sostenida en el precio de las criptomonedas, o dicho de otra manera, “se enfría su precio”.
Rüyada Alt Tarafını Açık Görmek Ne Anlama Gelir?
Quality articles is the key to attract the users to pay a visit the web site, that’s what this website is providing.
Awesome website you have here but I was curious about if you knew of any message boards that cover the same topics talked about in this article? I’d really love to be a part of online community where I can get comments from other knowledgeable individuals that share the same interest. If you have any recommendations, please let me know. Kudos!
I like it when individuals come together and share thoughts. Great blog, keep it up!
If you want to take much from this piece of writing then you have to apply such techniques to your won blog.
What’s up, I desire to subscribe for this webpage to take newest updates, so where can i do it please assist.
I was wondering if you ever considered changing the page layout of your site? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having one or two images. Maybe you could space it out better?
Thank you a bunch for sharing this with all people you really recognize what you are talking approximately! Bookmarked. Please also discuss with my web site =). We could have a link change contract among us
For the last 50 years, Motorcraft has built a reputation for quality, dependability and performance. Time to celebrate this milestone 50th anniversary. In the Economy category you will find all Ford parts that have exceeded the age of five years. Ford provides the production of spare parts for its models after five years. But a car of the same brand is as good as new even after five years. … Our competent and experienced service team takes care of your concerns and queries. If you are not sure what to accurately seek and order, you can even contact us anytime via email and telephone. In support there are photos and drawings of the part to be replaced that are sometimes helpful. So the right replacement part can be more easily identified and our customer support team has a great skill and knowledge for your guidance. But it usually does not have to be so complicated. With us you find your items whether with or without our support. Because our Ford Parts catalog is extensive and almost complete.
http://www.pax.nichost.ru/forum/view_profile.php?UID=121538
If you need it, we’ve got it. When you need replacement of any auto part or spare part for your Ford Car, it is highly recommended that you use genuine Ford parts. Although some might say that the Ford aftermarket parts are also a good option as they are also good quality and available at low cost. There are no comments to display. If you have the choice between a Ford Genuine Part or a Motorcraft part, either one will work just fine. Motorcraft manufactures their parts for Ford vehicles, using the exact OEM specifications as implemented in the original manufacture of your Ford. Thus, it will work the same as a Ford Genuine Part. Every Ford part sold through our online store comes complete with a free warranty. Our service is 5-star rated, ensuring peace of mind when you buy Ford parts from us.
With havin so much content and articles do you ever run into any problems of plagorism or copyright violation? My website has a lot of completely unique content I’ve either created myself or outsourced but it appears a lot of it is popping it up all over the web without my authorization. Do you know any techniques to help protect against content from being ripped off? I’d truly appreciate it.
My spouse and I stumbled over here different page and thought I may as well check things out. I like what I see so now i am following you. Look forward to going over your web page yet again.
Hi there! I could have sworn I’ve been to this website before but after going through some of the posts I realized it’s new to me. Nonetheless, I’m definitely pleased I found it and I’ll be bookmarking it and checking back frequently!
I blog frequently and I genuinely appreciate your content. This article has really peaked my interest. I am going to book mark your website and keep checking for new information about once a week. I subscribed to your RSS feed as well.
I like the valuable information you supply on your articles. I will bookmark your weblog and test again here frequently. I am moderately certain I will be informed many new stuff right here! Good luck for the following!
Эффективное термоизоляция фасадов — прекрасие и бюджетность в личном доме!
Согласитесь, ваш дом заслуживает первоклассного! Воздухонепроницаемость обшивки – не голос решение для экономии на отоплении, это инвестиция в удобство и долговечность вашего дома.
? Почему термоизоляция с нашей компанией?
Опыт: Специалисты нашей компании – опытные. Мы все заботимся о каждом аспекте, чтобы обеспечить вашему жилью идеальное термоизоляция.
Расходы изоляции: Мы ценим ваш средства. [url=https://stroystandart-kirov.ru/]Сколько стоит сделать утепление фасада[/url] – начиная от 1350 руб./кв.м. Это инвестиция в ваше удовлетворительное будущее!
Энергосберегающие меры: Забудьте о потерях тепловой энергии! Наш метод не только сохраняют теплоту, но и дарят вашему жилью новый уровень теплосбережения энергоэффективности.
Сделайте свой домашний интерьер пригодным для проживания и стильным и привлекательным!
Подробнее на [url=https://stroystandart-kirov.ru/]n-dom.ru
[/url]
Не предоставляйте свой дом на произвольное решение. Доверьтесь профессионалам и создайте тепло вместе с нашей командой!
Sure Football Prediction For Today, we have 15 accurate football predictions guaranteed to put money in your pocket. We pick Embeddable RSS Widgets Each week we cover all of the games in the Premier League, Major League Soccer (MLS), and from the group stages onwards in the Champions League and Europa League. With Pickswise’s international expertise we provide the most informed and best free soccer predictions today. The top-ranked Georgia Bulldogs battle the Florida Gators on Saturday in Jacksonville. 18+ We aim to post the majority of our soccer predictions a day ahead so you can look today at our soccer predictions for tomorrow. With soccer team sheets only being made public an hour before kick-off, you need to do your due diligence with team lineups, news, and team vs team matchups before making your soccer predictions. The benefit of posting our soccer predictions for tomorrow, today, is that you have time to digest the research, analysis, and key stats before placing a wager, and you can also get better odds the day before if public money then comes on one side of the line. Some of our picks will be posted on the morning of the game
https://www.bookmarking-online.win/bundesliga-odds
Punters can bet using NBA picks consensus to see which team bettors are putting their money on and decide whether they want to go with or against the public. If you want to succeed wagering on NBA betting lines, we suggest you consider the different types of sportsbooks available. It will help you get an understanding of the public’s betting habits. Bettors can also find the best wager lines. Bettor need to note that line changes are in most cases are initiate by how the public bets. In most cases, the team mostly selected by the public is likely to have lower odds, regardless of the fact that they are not always the team that will most likely win. The National Basketball Association (NBA) is the premier men’s professional basketball league in the world. It is composed of 30 teams; 29 in the United States and 1 in Canada. The NBA playoffs are a best-of-seven elimination tournament annually held after the NBA regular season to determine the league’s champion. Check out our NBA Finals Championship Odds, News & Analysts
hi ,,that was helpful ,,
Эффективное теплосбережение облицовки — счастье и бережливость в личном домовладении!
Согласитесь, ваш домовладение заслуживает отличного! Утепление внешних стен – не голос решение для экономии на тепле, это вклад в удобство и устойчивость вашего недвижимости.
? Почему изоляция с специалистами?
Мастерство: Наши специалисты – компетентные. Мы все заботимся о каждом элементе, чтобы обеспечить вашему дому идеальное теплосбережение.
Сумма изоляции: Мы ценим ваш средства. [url=https://stroystandart-kirov.ru/]Цена м2 утепление фасада дома[/url] – начиная от 1350 руб./кв.м. Это вложение средств в ваше комфортное будущее!
Энергосберегающие меры: Забудьте о термических потерях! Материалы, которые мы используем не только сохраняют тепловую энергию, но и дарят вашему дому новый уровень уюта энергоэффективности.
Обустройте свой домашний уголок теплым и уютным и изысканным!
Подробнее на [url=https://stroystandart-kirov.ru/]www.stroystandart-kirov.ru
[/url]
Не покидайте свой загородный дом на произвол судьбы. Доверьтесь профессионалам и создайте комфорт вместе с нами-специалистами!
Наша бригада квалифицированных специалистов проштудирована выдвинуть вам инновационные системы, которые не только ассигнуруют устойчивую охрану от холодильности, но и дарят вашему собственности трендовый вид.
Мы практикуем с новыми компонентами, заверяя долгосрочный время службы и прекрасные итоги. Теплоизоляция наружных поверхностей – это не только экономия энергии на прогреве, но и заботливость о экосистеме. Экологичные методы, какие мы производим, способствуют не только личному, но и сохранению природы.
Самое основополагающее: [url=https://ppu-prof.ru/]Ремонт и утепление фасада дома[/url] у нас начинается всего от 1250 рублей за м2! Это доступное решение, которое изменит ваш резиденцию в реальный тепличный уголок с скромными расходами.
Наши проекты – это не только изолирование, это разработка помещения, в где каждый член выражает ваш индивидуальный манеру. Мы возьмем во внимание все твои потребности, чтобы осуществить ваш дом еще еще более удобным и привлекательным.
Подробнее на [url=https://ppu-prof.ru/]ppu-prof.ru/[/url]
Не откладывайте труды о своем корпусе на потом! Обращайтесь к профессионалам, и мы сделаем ваш помещение не только тепличным, но и моднее. Заинтересовались? Подробнее о наших трудах вы можете узнать на официальном сайте. Добро пожаловать в мир гармонии и качества.
Great blog! I’m considering a writing role. Could you share details on the application process?
Endopeak is a natural energy-boosting formula designed to improve men’s stamina, energy levels, and overall health. The supplement is made up of eight high-quality ingredients that address the underlying cause of declining energy and vitality. https://endopeakbuynow.us/
GlucoBerry is one of the biggest all-natural dietary and biggest scientific breakthrough formulas ever in the health industry today. This is all because of its amazing high-quality cutting-edge formula that helps treat high blood sugar levels very naturally and effectively. https://glucoberrybuynow.us/
Folixine is a enhancement that regrows hair from the follicles by nourishing the scalp. It helps in strengthening hairs from roots. https://folixinebuynow.us/
EyeFortin is an all-natural eye-health supplement that helps to keep your eyes healthy even as you age. It prevents infections and detoxifies your eyes while also being stimulant-free. This makes it a great choice for those who are looking for a natural way to improve their eye health. https://eyefortinbuynow.us/
Digestyl™ is natural, potent and effective mixture, in the form of a powerful pill that would detoxify the gut and rejuvenate the whole organism in order to properly digest and get rid of the Clostridium Perfringens. https://digestylbuynow.us/
Erec Prime is a natural formula designed to boost your virility and improve your male enhancement abilities, helping you maintain long-lasting performance. This product is ideal for men facing challenges with maintaining strong erections and desiring to enhance both their size and overall health. https://erecprimebuynow.us/
Sugar Defender is the #1 rated blood sugar formula with an advanced blend of 24 proven ingredients that support healthy glucose levels and natural weight loss. https://sugardefenderbuynow.us/
GlucoTrust is a revolutionary blood sugar support solution that eliminates the underlying causes of type 2 diabetes and associated health risks. https://glucotrustbuynow.us/
HoneyBurn is a revolutionary liquid weight loss formula that stands as the epitome of excellence in the industry. https://honeyburnbuynow.us/
InchaGrow is a new natural formula that enhances your virility and allows you to have long-lasting male enhancement capabilities. https://inchagrowbuynow.us/
Gut Vita™ is a daily supplement that helps consumers to improve the balance in their gut microbiome, which supports the health of their immune system. It supports healthy digestion, even for consumers who have maintained an unhealthy diet for a long time. https://gutvitabuynow.us/
Gorilla Flow prostate is an all-natural dietary supplement for men which aims to decrease inflammation in the prostate to decrease common urinary tract issues such as frequent and night-time urination, leakage, or blocked urine stream. https://gorillaflowbuynow.us/
Casinos offering No Deposit Casino Bonuses Keep your eyes peeled for lots of good news via the Jackpot Capital online casino promotions page and absolutely take advantage of golden opportunities to redeem a Jackpot Capital coupon code or one of our hot online casino offers. There are always plenty of online casino promotions to be found at Jackpot Capital that will add to your playing enjoyment and chance to win. Since 2007, we’ve provided the Best No Deposit Bonuses for some of the biggest online casinos across the world. Our list of codes is maintained regularly and valid for players in the United States, Canada, Australia, and the United Kingdom as well as many other countries. At LCB, members and guests of the site continuously post any information they have on the current no deposits bonuses and recent no deposit bonus codes. Join in on the information sharing by posting bonuses you find or just catch up on the latest ND codes.
https://www.strobe-bookmarks.win/new-no-deposit-bonus-for-ruby-slots
Play Crazy Time offers unbiased insights on Evolution Gaming’s popular live casino game, Crazy Time. As an independent site, we hold no affiliation with Evolution or other gambling companies. Interested in casino bonuses that offer high estimated value returns? Check out Casino Wager for advanced casino wager tools. Considering that Crazy Time is a live casino game played in real-time, it’s implausible for the results to vary from one player to another. The wheel for Crazy Time is jam-packed with excitement. It’s bursting with colour and each colour represents a different kind of win. There is a blue 1x, the 2x segment is yellow, the 5x one is pink and there is a purple 10x segment. All of these money tiles are interrupted by different special feature tiles which punters can land on to activate bonuses.
Hello there, I do believe your web site might be having internet browser compatibility issues. When I look at your web site in Safari, it looks fine however, if opening in IE, it has some overlapping issues. I simply wanted to give you a quick heads up! Besides that, wonderful website!
Last year’s Kentucky Derby saw a stunning result as Rich Strike came out of nowhere to win the race. After entering with 80-1 odds, Rich Strike pulled off the second-biggest upset in the event’s history. We’ll revisit these odds as the season progresses. With each passing prep race, the number of viable Derby contenders will shrink, but as of now, there are dozens of horses out there that carry the dreams of owners and gamblers alike to find the Churchill Downs winner’s circle after the first jewel of the Triple Crown – and some of them may not have even started in a points race yet. Digital Replica Edition Now the team will have to be at some other big races. Five short days ago King Russell was the biggest Kentucky Derby longshot on the board at 80-1 odds.
https://preniumdirectory.com/listings12605184/money-line-meaning-football
Get access to the best soccer betting tips by visiting our website on daily basis. Our website aims at providing … Make maximum PROFITS from our sure “2 to 5 ” daily Football Predictions. DISCLAIMER: Our soccer prediction platform provides forecasts based on available data and statistical analysis. However, we do not guarantee the accuracy or completeness of our predictions, and we cannot be held responsible for any losses or damages that may result from reliance on our forecasts. Please be aware that sports events are inherently unpredictable, and our predictions are intended for informational and entertainment purposes only. We strongly advise our users to exercise caution and seek professional advice before making any decisions based on our predictions. By using our platform, you agree to our terms of service and acknowledge that our predictions are not a guarantee of a particular outcome.
We are a group of volunteers and starting a new scheme in our community. Your web site provided us with helpful information to work on. You have performed an impressive task and our whole community can be grateful to you.
I am absolutely thrilled to introduce you to the incredible Sumatra Slim Belly Tonic! This powdered weight loss formula is like no other, featuring a powerful blend of eight natural ingredients that are scientifically linked to fat burning, weight management, and overall weight loss. Just imagine the possibilities! With Sumatra Slim Belly Tonic, you have the opportunity to finally achieve your weight loss goals and transform your body into the best version of yourself.
Aviator Spribe играть бесплатно
It is a pity, that now I can not express – there is no free time. I will be released – I will necessarily express the opinion.
Добро пожаловать в захватывающий мир авиаторов! Aviator – это увлекательная игра, которая позволит вам окунуться в атмосферу боевых действий на небе. Необычные графика и захватывающий сюжет сделают ваше путешествие по воздуху неповторимым.
Играйте в Авиатор Спраб и зарабатывайте деньги вместе с нами уже сегодня!
Aviator игра позволит вам почувствовать себя настоящим пилотом. Вам предстоит совершить невероятные маневры, выполнять сложные задания и сражаться с противниками. Улучшайте свой самолет, чтобы быть готовым к любым ситуациям и становиться настоящим мастером.
Основные особенности Aviator краш игры:
1. Реалистичная графика и физика – благодаря передовой графике и реалистичной физике вы почувствуете себя настоящим пилотом.
2. Разнообразные режимы игры и миссии – в Aviator краш игре вы сможете выбрать различные режимы игры, такие как гонки, симулятор полетов и захватывающие воздушные бои. Кроме того, каждая миссия будет предлагать свои собственные вызовы и задачи.
3. Улучшение и модернизация самолетов – в игре доступны различные модели самолетов, которые можно покупать и улучшать. Вы сможете устанавливать новое оборудование, улучшать двигательность и мощность своего самолета, а также выбирать различные варианты окраски и декорации.
Aviator краш игра – это возможность испытать себя в роли авиатора и преодолеть все сложности и опасности воздушного пространства. Почувствуйте настоящую свободу и адреналин в Aviator краш игре онлайн!
Играйте в «Авиатор» в онлайн-казино Pin-Up
Aviator краш игра онлайн предлагает увлекательную и захватывающую игровую атмосферу, где вы становитесь настоящим авиатором и сражаетесь с самыми опасными искусственными интеллектами.
В этой игре вы должны показать свое мастерство и смекалку, чтобы преодолеть сложности многочисленных локаций и уровней. Вам предстоит собирать бонусы, уклоняться от препятствий и сражаться с врагами, используя свои навыки пилотирования и стрельбы.
Каждый уровень игры Aviator краш имеет свою уникальную атмосферу и задачи. Будьте готовы к неожиданностям, так как вас ждут захватывающие повороты сюжета и сложные испытания. Найдите все пути к победе и станьте настоящим героем авиатором!
Авиатор игра является прекрасным способом провести время и испытать настоящий адреналиновый разряд. Готовы ли вы стать лучшим авиатором? Не упустите свой шанс и начните играть в Aviator краш прямо сейчас!
Aviator – играй, сражайся, побеждай!
Aviator Pin Up (Авиатор Пин Ап ) – игра на деньги онлайн Казахстан
Aviator игра предлагает увлекательное и захватывающее разнообразие врагов и уровней, которые не оставят равнодушными даже самых требовательных геймеров.
Враги в Aviator краш игре онлайн представлены в самых разных формах и размерах. Здесь вы встретите группы из маленьких и быстрых врагов, а также огромных боссов с мощным вооружением. Разнообразие врагов позволяет игрокам использовать разные тактики и стратегии для победы.
Кроме того, Aviator игра предлагает разнообразие уровней сложности. Выберите легкий уровень, чтобы насладиться игровым процессом, или вызовите себе настоящий вызов, выбрав экспертный уровень. Независимо от выбранного уровня сложности, вы получите максимум удовольствия от игры и окунетесь в захватывающий мир авиаторов.
Играйте в Aviator и наслаждайтесь разнообразием врагов и уровней, которые позволят вам почувствовать себя настоящим авиатором.
Наша бригада опытных мастеров подготовлена предложить вам передовые технологии, которые не только подарят надежную покров от холода, но и подарят вашему зданию модный вид.
Мы работаем с современными материалами, сертифицируя постоянный запас службы и превосходные выходы. Изолирование облицовки – это не только экономия тепла на подогреве, но и внимание о природной среде. Сберегательные инновации, какие мы внедряем, способствуют не только зданию, но и поддержанию экосистемы.
Самое центральное: [url=https://ppu-prof.ru/]Утепление фасада цена за кв м[/url] у нас начинается всего от 1250 рублей за м²! Это доступное решение, которое сделает ваш хаус в фактический уютный угол с минимальными затратами.
Наши работы – это не всего лишь изоляция, это формирование поля, в где любой компонент отражает ваш индивидуальный манеру. Мы примем во внимание все все ваши желания, чтобы осуществить ваш дом еще более дружелюбным и привлекательным.
Подробнее на [url=https://ppu-prof.ru/]www.ppu-prof.ru[/url]
Не откладывайте труды о своем жилище на потом! Обращайтесь к спецам, и мы сделаем ваш дом не только согретым, но и модернизированным. Заинтересовались? Подробнее о наших работах вы можете узнать на портале. Добро пожаловать в универсум уюта и высоких стандартов.
What’s Taking place i’m new to this, I stumbled upon this I have found It positively helpful and it has helped me out loads. I am hoping to give a contribution & aid other users like its helped me. Good job.
Have you ever thought about creating an e-book or guest authoring on other sites? I have a blog based upon on the same information you discuss and would really like to have you share some stories/information. I know my audience would value your work. If you are even remotely interested, feel free to send me an e-mail.
Echoing the sentiments above – this post is a true gem!
Hi there I am so grateful I found your website, I really found you by error, while I was browsing on Google for something else, Nonetheless I am here now and would just like to say thanks a lot for a marvelous post and a all round thrilling blog (I also love the theme/design), I don’t have time to go through it all at the minute but I have book-marked it and also included your RSS feeds, so when I have time I will be back to read much more, Please do keep up the superb job.
Yes! Finally something about %keyword1%.
These games will catch on, and fast, and entertain your followers while they’re chilling at home. Do everyone a favor and go “live” with your SO as soon as possible, and play these 12 games. Start your session off with a catchy phrase like, “Let the laughs and mems commence.” The TV presenter took to her Stories on Saturday and shared a clip of the rapper, 30, greeting her after she returned from filming Love Island Games in Fiji. Oklahoma State would march down the field on a nine-play, 83-yard drive on its next possession to go up 14-0 just under eight minutes into the game. The presenter, who has 223,000 followers on Instagram, has before found herself in the face of social media controversy, including one 2019 tweet about Nine journalist Seb Costello that saw Bartholomew pay s $20,000 fine.
https://forum.linuxcnc.org/cb-profile/pluginclass/cbblogs?action=blogs&func=show&id=7001
Already an Xfinity Internet customer? Enroll in Xfinity Rewards today to explore a mix of special perks and experiences just for being a customer. Today, we announced Check Point Quantum SASE, bringing a powerful and unique Secure Access Service Edge (SASE) solution to customers around the world. Lam LT. Internet gaming addiction, problematic use of the internet, and sleep problems: a systematic review. Curr Psychiatry Rep. 2014;16(4):444. Even when you’re playing an offline game, it can still offer social benefits. Many people likely share your passion for the game that you’re playing. Seeking them out can give you a chance to meet new friends or connect with a community of like-minded individuals. Also, the level and types of communication online games offer has evolved significantly over recent years. Whereas games were seen separately to social media, they now greatly overlap with online social sharing sites. In fact, most children’s first interaction with someone they don’t know online is now more likely to be in a video game like Roblox than anywhere else.
Your post is a ray of light in the darkness. Thank you for brightening my day in a unique way. Keep shining!
wonderful day commencing with a tremendous reading 📚🌅
I loved your article post.Thanks Again. Much obliged.
Наша юкос выдает профессиональные услуги по бурению скважин на воду в С-петербурге равным образом Питерской области. Наша сестра владеем состоятельным эмпирически в этой району и еще заручим качественное создавание цельных работ.
Бурение скважин – это фундаментальный а также эффективный фотоспособ обеспечения хозяйственного хозяйства, компаний и порядков невинной (а) также лучшей водой. Наша ювентус знатоков осуществляет эмпайр скважин разнообразной глубины и поперечника, с точки зрения отличительные черты донных вожак на точном регионе – https://burenie-na-vodu-spb.ru/lomonosovsky/gorbunki/.
Наша сестра используем сегодняшнее ясс да технологии, что разрешает нам проделывать вещицы быстро равным образом безопасно. Наша цель – снабдить посетителей надежным и устойчивым водоснабжением, которое хорэ поклоняться долгие годы.
Помимо бурения скважин, автор этих строк также предлагаем хостинг-услуги по обустройству глубинной системы: установка насосов, фильтров, резервуаров также противоположного оборудования для благосостояния комфортного пользования водой.
You are so cool! I do not think I’ve read a single thing like that before.
So wonderful to find someone with unique thoughts on this subject.
Really.. thanks for starting this up. This web site is something
that is needed on the web, someone with a little originality!
If you desire to obtain a great deal from this article then you have to apply these
strategies to your won webpage.
Наша группа искусных исполнителей подготовлена предоставить вам современные средства, которые не только предоставят надежную оборону от холода, но и подарят вашему собственности оригинальный вид.
Мы занимаемся с современными компонентами, заверяя прочный запас использования и замечательные результаты. Изоляция внешнего слоя – это не только экономия энергии на тепле, но и забота о природной среде. Сберегательные разработки, каковые мы претворяем в жизнь, способствуют не только твоему, но и поддержанию природных ресурсов.
Самое важное: [url=https://ppu-prof.ru/]Утепление фасадов за 1 кв[/url] у нас открывается всего от 1250 рублей за метр квадратный! Это бюджетное решение, которое превратит ваш помещение в фактический уютный угол с минимальными затратами.
Наши пособия – это не только утепление, это созидание площади, в где все элемент выражает ваш персональный образ действия. Мы берем во внимание все все ваши требования, чтобы воплотить ваш дом еще еще более дружелюбным и привлекательным.
Подробнее на [url=https://ppu-prof.ru/]http://ppu-prof.ru[/url]
Не откладывайте труды о своем корпусе на потом! Обращайтесь к профессионалам, и мы сделаем ваш помещение не только более теплым, но и стильным. Заинтересовались? Подробнее о наших услугах вы можете узнать на веб-ресурсе. Добро пожаловать в сферу гармонии и стандартов.
7STAR娛樂城提供百家樂、老虎機、今彩539、天天樂、運彩賽事、德州撲克、麻將技巧、大樂透、電子競技、賓果、四星彩、威力彩,娛樂城推薦評價,最優惠的娛樂城體驗金。
七星娛樂城提供百家樂破解、百家樂賺錢、百家樂預測、百家樂算牌、技巧、規則、歐博、沙龍、dg、wm、真人線上百家樂推薦遊戲試玩,教學打法的介紹,補牌程式贏錢。
7星娛樂城提供老虎機技巧、老虎機訣竅、老虎機攻略、老虎機介紹、老虎機破解、雷神之鎚、魔龍傳奇、拉霸機遊戲、金猴爺老虎機、捕魚機,cq9試玩尋找出好贏的熱門遊戲。
Buy Drugs
п»їbest mexican online pharmacies: mexican pharmacy – mexico drug stores pharmacies
PBN sites
We shall build a structure of private blog network sites!
Benefits of our private blog network:
WE DO everything SO THAT Google DOES NOT comprehend that THIS IS A private blog network!!!
1- We acquire domain names from distinct registrars
2- The main site is hosted on a virtual private server (Virtual Private Server is high-speed hosting)
3- Additional sites are on separate hostings
4- We designate a unique Google ID to each site with verification in Search Console.
5- We design websites on WP, we don’t utilise plugins with assistance from which malware penetrate and through which pages on your websites are created.
6- We never duplicate templates and utilise only unique text and pictures
We refrain from work with website design; the client, if desired, can then edit the websites to suit his wishes
indian pharmacy online http://indiaph24.store/# reputable indian pharmacies
mail order pharmacy india
п»їbest mexican online pharmacies: mexican mail order pharmacies – buying prescription drugs in mexico
Мы группа специалистов по SEO-оптимизации, специализирующихся на повышении посещаемости и рейтинга вашего сайта в поисковых системах.
Мы добились впечатляющих результатов и желаем поделиться с вами нашими знаниями и навыками.
Что мы можем вам предложить:
• [url=https://seo-prodvizhenie-ulyanovsk1.ru/]сео раскрутка сайтов стоимость[/url]
• Исчерпывающая оценка вашего сайта и разработка индивидуальной стратегии продвижения.
• Улучшение контента и технических параметров вашего сайта для максимального эффекта.
• Регулярный анализ результатов и мониторинг вашего онлайн-присутствия для его улучшения.
Подробнее [url=https://seo-prodvizhenie-ulyanovsk1.ru/]https://seo-prodvizhenie-ulyanovsk1.ru/[/url]
Наши клиенты уже видят результаты: увеличение трафика, улучшение позиций в поисковых системах и, конечно же, рост прибыли. Вы можете получить бесплатную консультацию у нас, для обсуждения ваших требований и разработки стратегии продвижения, соответствующей вашим целям и бюджету.
Не упустите шанс улучшить свои результаты в интернете. Обращайтесь к нам уже сегодня.
Understanding COSC Certification and Its Importance in Horology
COSC Validation and its Demanding Standards
COSC, or the Official Swiss Chronometer Testing Agency, is the official Swiss testing agency that verifies the accuracy and accuracy of wristwatches. COSC accreditation is a sign of quality craftsmanship and reliability in timekeeping. Not all timepiece brands seek COSC certification, such as Hublot, which instead sticks to its own demanding standards with movements like the UNICO, reaching similar accuracy.
The Art of Precision Timekeeping
The central system of a mechanical watch involves the mainspring, which provides energy as it loosens. This mechanism, however, can be susceptible to environmental factors that may impact its precision. COSC-accredited mechanisms undergo rigorous testing—over fifteen days in various conditions (5 positions, three temperatures)—to ensure their resilience and dependability. The tests evaluate:
Average daily rate precision between -4 and +6 seconds.
Mean variation, maximum variation levels, and effects of thermal variations.
Why COSC Validation Matters
For watch enthusiasts and collectors, a COSC-accredited watch isn’t just a item of technology but a demonstration to lasting quality and accuracy. It signifies a timepiece that:
Offers excellent dependability and accuracy.
Offers guarantee of superiority across the complete construction of the timepiece.
Is apt to maintain its worth more effectively, making it a sound choice.
Famous Chronometer Brands
Several renowned brands prioritize COSC certification for their watches, including Rolex, Omega, Breitling, and Longines, among others. Longines, for instance, offers collections like the Archive and Spirit, which highlight COSC-certified movements equipped with cutting-edge materials like silicon balance springs to boost durability and performance.
Historic Background and the Evolution of Chronometers
The idea of the chronometer originates back to the need for exact timekeeping for navigational at sea, emphasized by John Harrison’s work in the eighteenth century. Since the official foundation of Controle Officiel Suisse des Chronometres in 1973, the accreditation has become a yardstick for judging the accuracy of luxury timepieces, continuing a tradition of excellence in horology.
Conclusion
Owning a COSC-validated watch is more than an visual selection; it’s a dedication to excellence and accuracy. For those appreciating accuracy above all, the COSC accreditation provides tranquility of mind, ensuring that each accredited timepiece will function dependably under various circumstances. Whether for individual satisfaction or as an investment decision, COSC-validated timepieces distinguish themselves in the world of watchmaking, carrying on a tradition of meticulous chronometry.
賭網