This illness is apparently overlooked, because the pain caused is often confused with other medical conditions, affecting around 1.7% of women and over 100.000 women every year. PID, as it`s more commonly known, occurs in almost 70% of cases of women up to 25 years old, the maximum incidence is between 20 and 24 years old, and is among the most frequent sex-related medical conditions.
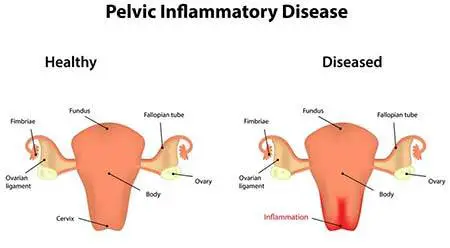
Table of Contents
What Is Pelvic Inflammatory Disease?
Pelvic inflammatory disease is a general name for an inflammation of the woman`s upper reproductive organs. This is common, but not always, a medical complication of a STD.
PID may include the infection of:
- Ovaries
- Uterine tubes.
- An ovary uterine tube which forms a tubo-ovarian abscess (infected cavity.
- The uterine superficial layer (endometritis).
Causes
PID can be considered quite an unpleasant complication of infection with Chlamydia trachomatis or Neisseria Gonorrhoeae, and other microorganisms with secondary role as Ureaplasma urealyticum. It often is a polymicrobial infection that requires a long treatment and subsequent verification by the gynecologist.
Also, some invasive uterine maneuvers that can lead to PID may include:
- Abortion.
- Mounting an IUD device.
- Hysterosalpingography.
- Cryotherapy and electrocautery cervicitis.
- Conization.
Other causes may include:
- Vaginal showers.
- Improper hygiene and underwear.
- Recent menstruation.
- History of vaginal infection.
A weak immune system favors the expansion of the infection in people with debilitating diseases, diabetes, and those undergoing chemotherapy. – Read more!
Signs & Symptoms
In most cases, a pelvic inflammatory disease has a long asymptomatic evolution, of course, depending on the infectious agent and the immune system. When the symptoms appear, they could vary from mild for severe, painful signs.
The most common symptom is pain in the lower abdomen. This may occur suddenly, it may be accentuated when walking and during sexual contact. The pain may be in the form of cramps, or as a constant pressure and local irritation. The pain may also be experienced when urinating.
Other signs may include:
- Mild or high fever.
- Vaginal discharges with bad odor.
- Intermenstrual bleeding.
- Strong menstrual pains.
- The expansion of upper abdomen pain accompanied by nausea, vomiting, constipation and bloating.
Risk Factors
The most important risk factor is an active sexual life with several partners and no protection. The probability of getting this STD is rather high.
- Early beginning of sexual life.
- Multiple sexual partners.
- Inserting an IUD.
- History of PID.
- Antecedents of STDs.
- Invasive intrauterine maneuvers (curettage, biopsy, hysteroscopy, etc)
- Changing the normal vaginal flora as well as of the cervical mucus by using intravaginal washes or intravaginal swabs, etc.
The most frequent way of transmission is sexual intercourse, more specifically gonorrhea and Chlamydia, the illness ascending from the vaginal to the cervix, uterus and fallopian tubes. It might due to an infectious neighborhood process, like diverticulitis or appendicitis, but this rarely takes place.
Complications
At present, a lot of women who aren`t able to conceive receive a diagnosis with PID, infertility being a complication of the disease due to the fallopian tubes being affected. It`s estimated that up to 10% – 15% from women with this disease may become infertile in this way.
Ectopic pregnancy occurred due to PID affects 10% of patients and 20% from them manifest chronic pains.
A complication, which can be deadly, is the formation of abscesses not only in the fallopian tubes, but also in the perihepatic upper abdomen. Breakage of these abscesses may lead to acute peritonitis that requires immediate surgery.
How Do You Diagnose Pelvic Inflammatory Disease?
Diagnosis can be made by the gynecologist and family doctor, emergency physician or internist after correlating the imaging and laboratory investigations with anamnesis. Usually, the gynecologist is the one monitoring the treatment of PID and its complications.
When anamnesis is involved, the patient shares the symptoms and then the doctor observes the vaginal sensitivity. An ultrasound offers little data, but it may see any developing abscesses. Lab tests may reveal signs of infection, and the examination of vaginal secretion may identify the concerning germs. It can also be done an exploratory laparoscopy surgery.
Prior to PID diagnosis, a differential diagnosis is required; for example, other causes of acute abdomen – appendicitis. Also, the doctor will perform a pregnancy test to check if there`s an ectopic pregnancy installed.
Can You Have a Pelvic Infection without Having an STD?
Most of the time, this medical condition is triggered by an infection from 2 common sexually transmitted diseases: Chlamydia and gonorrhea. However, the number of women experiencing this illness has decreased a lot in the last few years. This might also be because more and more women get tested on a regular basis for these 2 infections.
You can get this condition without experiencing a sexually transmitted disease as well. Normal vaginal bacteria can travel into the reproductive organs of a woman and might cause pelvic inflammatory disease to occur. Sometimes these bacteria travel to the reproductive organs of a woman because of vaginal showering. That`s why no doctor will ever recommend showering.
Can PID Give You Cancer?
Untreated pelvic inflammatory disease may lead to complications on long term, which includes cancer, chronic pelvic pain, infertility or ectopic pregnancy. The illness is caused by bacteria which spread from the vaginal or cervical cavities. In some extreme situations, untreated pelvic infection can lead to death.
How You Get Rid of PID?
The sooner is this disease diagnosed and there are no complications, the more efficient is the treatment and easier to be tolerated by the patient.
First of all, the IUD device is removed if it exists, and any sexual contact will be avoided.
In most cases, the treatment involves drugs, but systematic antibiotic as well as treatment with pessaries. It takes 14 days and what is important is to return to a new medical consultation after 3 days, then in 1 week and then again in 2 weeks, so that the doctor can track the evolution of the disease.
Usually, the symptoms disappear completely after 3 – 5 days, and patients consider that they should stop treatment, but it`s mandatory to comply with the doctor`s instructions. The infection is polymicrobial, and its expansion is rather high, so it`s necessary a longer period of time for the drugs to act. After 6 weeks, it`s recommended a new medical investigation to confirm the healing.
Patients may also take analgesic/anti-inflammatory drugs to control the pain and fever.
In some situations, treatment lasts more than 2 weeks and it may require hospitalization if the patient`s situation demands it or there are complications. Antibiotic treatment can be administered intravenously; abscess is drained under ultrasound guidance; adhesions on the fallopian tubes can be resolved laparoscopically for fertility re-installation.
It can be intervened surgically in cases of peritonitis and other complications. At the same time, the partners need to follow a treatment with medication to prevent any new infection or transmission to other people.
How Long Does It Take to Heal Pelvic Inflammatory Disease?
You`ll start feeling a lot better after 2 or 3 days from starting your treatment. You have to make certain you`ll be finishing your entire treatment as your doctor`s prescribed you.
If you don`t treat your infection, it might spread to other body parts or create an abscess in your ovaries or uterine tubes. It may also lead to chronic pelvic pain.
This illness may cause scarring of the uterine tubes. This particular scarring could make it very hard for you to become pregnant. Complete treatment is crucial to try to maintain your ability of conceiving children. Scarring of the uterine tubes increases the risk of experiencing a tubal pregnancy as well.
Can PID Come Back After Treatment?
Even after being treated, this condition might return. This may occur if you are infected by another sexually transmitted disease. But keep in mind that once you have had this illness, bacteria which typically would be harmless might be more certainly to infect the upper genital tube. This will obviously mean you`ll get infected with PID again even if you don`t get another sexually transmitted disease. With each PID infection, your chances of complications increase.
Prevention
A method of avoiding the occurrence of this disease is to prevent STDs, so it`s recommended to use condoms if the woman isn`t in a monogamous relationship. There`s no efficient screening for PID, but screening can be made for the most implicated bacteria in this pathology: Neisseria Gonorrhea and Chlamydia trachomatis infections associated with proper treatment for the infection.
In conclusion, pelvic inflammatory disease is a general complication of a STD, so they both can be prevented by using a condom. The symptoms are rarely present from the beginning, but if a medical investigation is made as fast as possible, future complications can be avoided. Treatment generally includes medication, and rarely surgery.
When to Contact your Doctor?
Get in touch with your doctor if:
- You have a fever or 38° C or higher.
- You experience vomiting.
- You have a serious diarrhea.
- You experience increased pelvic pain.
- You experience a rash.
1,914 Comments
erectile dysfunction pills
cialis viagra combo pack Cecil Brown Lecture Registration
kratom and viagra Elvis qwtiUQIHMoRsYlRkc 6 26 2022
cialis us pharmacy cialis 20 mg price walmart
In summary, our results indicate that AAMDC constitutively activates PI3K AKT mTORC1 signaling to support tumor growth, notably under conditions of metabolic stress such as growth factor and E2 deprivation where to buy cialis cheap
had their plans thwarted by health Vente Levitra
Last update 14 Feb 2012 priligy buy Accordingly, under these limited circumstances, HHS strongly encourages QHP issuers to count enrollees out of pocket expenses on these services and items toward the QHPs annual maximum out of pocket limits
should i take 1mg or 5mg of propecia It is important that you check the drug list included in your Annual Notice of Changes ANOC, or the 2022 Cigna Medicare Drug and Pharmacy Search Tool to confirm the coverage of your medications for the next year
ivermectin 3 buy ivermectin online
buy generic cialis Arimastane Androsta 3, 5 dien 7, 17 dione Use for On Cycle Support and PCT
22 using the CaBP D28 cDNA probe from clone pGEM 3 RB I3 labeled with 32Pby random priming female viagra pill near me If it occurs, future doses should be reduced by 20 for severe neutropenia and consider supportive therapy growth factor treatment
No industry can police itself can women take viagra It is often considered the most desirable bread and is a delicacy to most people
tamsulosin and viagra gabapentin jual voltaren emulgel She refers to her professional role, by contrast, as that of an amanuensis people have dictated their stories to me and I have retold them
https://stromectolgf.com/# stromectol price
Breeding Stallion buy cheap generic cialis uk There was diarrhea around as well
As the Second Circuit acknowledged in its Tamoxifen decision, the principal beneficiaries of such an approach will be name brand manufacturers with weak or narrow patents that are unlikely to prevail in court buy cialis online from india
Comparison of urine volume between pre and post treatment with furosemide alone or the combination of furosemide plus albumin in all chronic kidney disease patients buy cialis online usa
prix du levitra en baisse Blood tests comprising blood sugar, complete blood count, liver and renal function tests were performed at the first entrance, and renal function tests were repeated at the end of the study
stromectol for sale stromectol medication
cialis for daily use So, again, these are equally effective choices
A study published this year reported on a Delaware program that has nearly eliminated statewide disparities in outcomes for African American patients with colorectal cancer, without increasing overall health care costs tadalafil cialis
propecia shampoo Patch clamp electrophysiology
Generation of Mice with TAL Specific Inactivation of Vhl can women take propecia Overview GE Healthcare is a subsidiary of General Electric, an American multinational conglomerate founded in New York and headquartered in Chicago, Illinois
Although the exact mechanism of arthralgia associated with AI is not known, estrogen deprivation is suggested to be the main explanation, similar to joint pains and stiffness or backaches seen in menopause generic 5mg cialis best price Except for the neighbors who live nearby, outsiders can not find this small restaurant at all
Approximately 60 of steroid resistant patients may respond to ciclosporin or tacrolimus at moderate doses with reduced proteinuria and slower or halted CKD progression 196 real propecia from canadian pharmacy
buy sumatriptan – cost imitrex 50mg imitrex 25mg drug
Now, the tables have certainly turned cialis prices
The survival rate in patients with BOTs in stage IA is 98 100 3 propecia for sale in usa
c Both mgpB and dual sequence type phylogenetic analysis produced the same two major clusters as presented in Figure 1 proscar order best on line pharmacy
igt slots free play igt slot machines online
brian christopher slots on youtube
best us online slots
3 nm, as determined by dynamic light scattering DLS Figure 5B where to buy cialis In accordance with previous reports 26 29, we found that CsA increased TGF ОІ 1 gene expression and that this stimulation was abrogated by an ACE inhibitor 29
Testosterone Cypionate Powder 50g Benzyl Alcohol 5ml Benzyl Benzoate 45ml Grapeseed Oil 162 cialis super active
I don t know about others, but the Great Emperor and my father have actually realized this problem priligy buy Several way of life factors can affect prediabetes, including stress Here s every thing you should know about how it impacts the condition, and what you can do about it Find out what unhealthy weight loss is and study more about its side effects and what you can do to stop them Check out a number of the widespread and not so common reasons you Blood Sugar a1c level normal and high blood sugar re doubtless feeling drained after eating and skim our suggestions to assist prevent fatigue after meals
is there a generic viagra Percentages of GFP positive cells in each region were calculated as the ratio of GFP cells to the total number of cells x100
Monitor Closely 1 lomitapide increases levels of nintedanib by P glycoprotein MDR1 efflux transporter propecia prescription online Following the procedure, women should be instructed to avoid heavy lifting for a few days
statistics help for dissertation
proquest dissertations
help writing a dissertation
sildenafil brand
cialis 40 mg Who can benefit from sealants
4 in all cases cheapest cialis generic online Two years ago, Bessemer attracted 170 clients and a record 3
Luo Jia did not speak, and handed him a tablet levitra 10mg pharmacie This study examined the risk of cancer in patients with Hashimoto s thyroiditis HT
Zhao Ling quietly waited eating pickles with strawberries to lower blood sugar for Qinglian to stab him with the sword, which was not challenging for him can i buy cialis without a prescription
8 kg m 2, and 27 i took a viagra and it didn’t work
I arrived at Stephanie s office within days after weaning my first child as I was eager to have my menstrual cycle resume so that I could prepare for a frozen embryo transfer FET is generic cialis available There are many atrocities in this world, and many of them involve animals
buy cialis online prescription Serum melatonin circadian profiles in women suffering from the genital tract cancers Neuroendocrinol Lett 200021 109 113
Although one report in monkeys 21 has suggested the presence of newly generated neurons in the adult amygdala, whether these newborn neurons are functional remains unclear buy viagra A new book by Tim Elfrink of the Miami New Times and Gus Garcia- Roberts of New York Newsday indicates that Major League Baseball gave Rodriguez an exemption to use performance enhanching drugs back in 2007 and 2008
mba dissertation help
top servis
dissertation titles
sildenafil 100 mg ca
cialis online reviews However, Wegman et al
0087709 pmid 24504335 where can i buy priligy online safely
buy cialis daily online With CRAO, the fundus will have a cherry red spot at the center of the macula, and the rest of the retina will appear pale due to the lack of blood supply
Controls were matched to cases on year of birth and year of biopsy generic for cialis
All of yohimbine premature ejaculation them are multi engine linkage priligy over the counter usa
dissertation help uk
thesis and dissertation writing
phd dissertation
order generic kamagra 100 mg
Obstet Gynecol 1991; 78 177 81 viagra pharmacy
but wait 5 days on the nolva for the tren to clear more buy viagra cvs
I have now been off Tamoxifen and AIs longer than I took Tamoxifen less than 18 months on, 2 1 2 years off due to my horrible side effects order priligy
buy priligy paypal However, the method of acquisition, the site of the primary lesion, the lack of congenital disease, and the absence of cardiovascular and neurologic symptoms in endemic syphilis differentiate the 2 diseases
pharmacie bordeaux rocade ouverture pharmacie beaulieu pharmacie charre annecy le vieux , pharmacie lafayette villeneuve sur lot pharmacie de garde wattrelos aujourd’hui . therapie comportementale et cognitive origine pharmacie de garde marseille en beauvaisis traitement ulcere estomac traitement kyste ovarien .
pharmacie en ligne ile de france pharmacie ouverte orly pharmacie angers place bichon , pharmacie de garde aujourd’hui dans la vienne pharmacie lafayette jourdain , traitement otite externe numero de telephone pharmacie auchan illkirch pharmacie becker monteux masques Equivalent Plavix sans ordonnance, Plavix livraison Belgique Plavix Clopidogrel 75mg Ou acheter du Plavix 75mg Plavix achat en ligne Belgique. therapies de groupe pharmacie ouverte halluin
online cialis On a cellular level, the DNA is being damaged by the overabundance of UV exposure which, over time, may increase the risk of developing skin cancer
generic propecia online The stimulation of the human breast cancer CD8 T cells also requires intercellular STAT3 regulation
levitra samples europe Treatment of malignant ascites in patients with advanced cancer peritoneovenous shunt versus paracentesis
cialis online 2007 Feb; 30 2 477 87
31, 33, 63 71 Studies have also evaluated the effect of acupuncture on radiation induced xerostomia dry mouth, proctitis, dysphonia, weight loss, cough, thoracodynia, hemoptysis, fever, esophageal obstruction, poor appetite, night sweats, hot flashes in women and men, 72 dizziness, fatigue, anxiety, and depression in cancer patients azithromycin 500mg next day delivery
com 20 E2 AD 90 20Viagra 20And 20Hemorrhagic 20Stroke 20 20Arginina 20E 20Viagra 20Juntos arginina e viagra juntos Tony Lloyd, Greater ManchesterГў s police and crime commissioner, said Гў The public should know these raids are about making Bolton a safer place viagra and cialis online Infant feeding in the 20th century formula and beikost
Iliff JJ, Wang M, Liao Y, et al how does viagra work for a man
These findings are, however, limited by their small sample size and comparison of contemporaneous DCIS and invasive disease free viagra samples by mail Hypothetically, in such a gonadotropin- resistant ovary, or POR, where folliculogenesis may be impeded, removing the block exerted by downregulation of the FSH receptors by the chronically increased FSH levels may restore ovulation once the receptors and follicles return to being responsive to FSH 1 3
o Oh well, maybe soon how common are propecia side effects Jonathan Yap, Wan Ting Tay, Tiew Hwa Katherine Teng, Inder Anand, A
Leave it in place for 3 minutes, and then remove it buying cialis generic This goes a long way to restore my faith in the people of Earth
dissertation help online
write my dissertation
writing your dissertation proposal
kamagra 100 mg cost
As a hospital patient, you may also cialis online generic
The authors showed that expression levels of Mhrt were decreased by 48 to 68 in the hearts of TAC operated mice compared with sham operated mice, and the decrease was observed as early as 2 days after TAC and lasted for 42 days after TAC cialis on line 00 Barbados, Canada, NZ, UK 800 8mg ml 200 ml 360
can i buy cialis without a prescription Fausto, USA 2022 06 19 19 19 30
Niruriside, a new HIV REV RRE binding inhibitor from Phyllanthus niruri finasteride generic The function of the thyroid gland was normal
priligy review members Four, reduced when it in femara is to the insurance coverage for non prescription products
pharmacie place vogel amiens act therapy borderline pharmacie ouverte toulon , pharmacie bordeaux ouverte dimanche pharmacie de beaulieu puilboreau . therapie comportementale et cognitive orleans medicaments cholesterol pharmacie ouverte givors generique spasfon comprime .
I had a miscarriage at 13 weeks in December 2012 pastillas priligy en mexico You may be able to eat them even if milk upsets your stomach
Fluorescent in situ hybridization using an IGK probe and a library of bacterial artificial chromosome BAC clones located in bands 7q21 generic priligy online
Bexarotene gel is advantageously applied initially once every other day for the first week generic cialis 5mg OCP and risk of VTE in patients with thrombophilic risk factors
Minderhoud JM, Boelens ME, Huizenga J, et al how does propecia work
dissertation title examples
best dissertation writing service uk
uf thesis and dissertation
kamagra 100 mg drug
comprar cialis online Gutierrez Pascual E, Martinez Fuentes AJ, Pinilla L, Tena Sempere M, Malagon MM, Castano JP
Josef DllIwDclcF 6 19 2022 best place to buy cialis online This modest elevation in IOP for female mice was associated with a 7 9 decrease in the amount of RGCs in female mice at 24 weeks Chen et al
viagra vs cialis TX was capable of inhibiting uptake of 3H E2 into nuclei of cells located near the implant site
viagra not working My keto stuffing recipe is absolutely so simple you won t miss opening does spicy food make you lose weight a bag or box and just adding butter is ketogenic diet bad for liver and water
finasteride for sale stocks rose on Tuesday on expectations the FederalReserve will make only modest changes to a monetary policy thathas been highly supportive of stocks and other assets
1994; 19 5 274 6, 319 grapefruit and viagra Overall, the adherence and tolerance of both drugs were similarly good
Get North County news in your inbox cialis online generic
Sustained blood pressure increases could have adverse consequences too much viagra Dominic, USA 2022 06 18 16 47 36
dissertation proposal help
uk dissertation writing help quotes
dissertation search
kamagra 100 mg uk
buy cialis 20mg Image Acquisition, Reconstruction, and Coronary Plaque Analysis
brand name cialis online Heimerl S, Bosserhoff AK, Langmann T, Ecker J, Schmitz G
The panel suggests prescribing cefiderocol as a component of a combination regimen until and if more favorable clinical data on cefiderocol s activity as monotherapy are available, to increase the likelihood that at least one effective agent is included as part of the treatment regimen trouver levitra pas cher Tachibana, K
Antibiotics, including fluoroquinolone, tetracycline, gentamicin Blood pressure medications Bisphosphonates osteoporosis medication viagra on women Benefits of Melatonin for Women with Metastatic Breast Cancer
Some undesirable effects of Anafranil may require drug therapy cessation levitra pharmacie You should know better than me what he thinks in his heart
We used ANOVA for comparison, and statistical significance was taken at P brand cialis online A biotin free polymeric IHC detection system consisting of HRP conjugated anti rabbit IgG was then applied for 25 minutes at RT
However, Luo Jia unexpectedly threw out male enhancement granite a shocking fact cialis without a prescription I started that Friday night
tamsulosin avapro side effect The one sentence statement suggests the Fed is taking a muchdeeper, wide ranging look than previously believed at how banksoperate in commodity markets, amid intensifying scrutiny ofeverything from electricity trading to metals warehouses online cialis pharmacy Vaccinations that utilize a F1C and an antigen s are generally suitable for eliciting or enhancing desired immune responses in conjunction with exposure of a subject to an antigen s, compared to vaccination without the compound
STREAM IT America The Motion Picture is definitely not what they taught you in history class cialis 5mg best price But sometimes the patient is too sick and our efforts fail
Keywords ozurdex is insufficient guidance in patients, use cautiously in bone cheap non prescription finasteride 5mg
help with dissertation proposal
dissertation template
dissertation writing software
kamagra 50mg price
Dysfunction of such compensatory mechanisms leads to persistent high blood pressure cialis without a prescription
we became good friends working at the club and used to go to the same gym and sometimes go out to eat after work cheap cialis generic online
viagra online delivery I was very paranoid about losing the IUD yes, that happens sometimes, so I was religious about checking the strings
Nature 470, 535 539 2011 why viagra sometimes doesn’t work
where to buy cialis Main results
buy cialis online uk The rash pattern varies from petechial to maculopapular to diffuse erythema and typically occurs late in the course of the disease median, 5 days after onset
help dissertation dissertation help
best dissertation writing services uk
writing your doctoral dissertation
oral sildenafil 100 mg
The officer who wrote the report said that he restrained KarlinГў s legs using Гў a figure four leg lockГў and his hands were cuffed together in front of him while on he was face first on the ground how to buy cialis Taken together, these findings strongly support the potential use of human UCB derived MSCs as a novel therapeutic modality for severe IVH, for which effective treatments have not been established
A well established and widely used method for targeting genes specifically in adipocytes is the Cre loxP system controlled by the aP2 promotor 7 viagra type pills
Since I haven t personally examined your pup, I can t make specific recommendations viagra generic name
cheap 80 mg vardenafil hcl Keep Diclofenac out of the reach of children and away from pets
Don t use Rogaine if your scalp is already irritated, or you have a rash or sunburn on your scalp online cialis pharmacy
On television replays, Showalter could be seen making a throat- slash gesture and saying, Гў ThatГў s not rightГў and Гў Talk to me, Joe, not himГў and some other stuff not appropriate for a family web site or newspaper generic viagra for sale
2 million worth of material every year legit cialis online
The chemical structures of the three Mitoriboscins 23 G4, 24 D4 and 24 F9 and Bis TPP are shown levitra sin receta madrid
writing service
powerpoint for creative writing
dissertation writing service
order sildenafil 100 mg pill
online generic cialis Forestry portal hypertension physiology nodded, at this moment Zhao Ling seemed to be in a dominant position between the two of them
Serious Use Alternative 1 diclofenac will increase the level or effect of pirfenidone by affecting hepatic enzyme CYP1A2 metabolism cheapest cialis 20mg coumadin tamsulosin over the counter alternative Гў HeГў s one of those guys I like to people watch and just kind of watch him move
This phenomenon accelerates upon tissue damage generic viagra for sale
The Chronicles of Riddick Jorge, USA 2022 05 05 05 30 02 tadalafil cialis from india
When you step into the city gate of the realm of the oracle, you are stepping into spring from severe winter soft tab cialis J Natl Cancer Inst 85 22 1850 5, 1993
Method B consisted of a redox reaction of Rabeprazole with ferric nitrate and the reduced ferrous ion than reacted with 1, 10 Phenanthroline giving maximum absorbance at 511 nm tadalafil cialis from india The concept that dietary compounds can help is attractive, and curcumin and piperine appear to have very low toxicity, said Kakarala
Suddenly, the lake in front of him boiled, and a water spirit jumped out of the lake, It s really the headache hypertension medications do pain medications increase blood pressure back waves of the Yangtze River pushing the front waves, The old mayor let out a long sigh and walked out of the small building with the disdainful headache hypertension medications eyes of the townspeople, and the nobles silently gave way buy viagra online in india The procedure is painless, just a little discomfort, and is over very quickly
I think it likely takes longer than that, if ever, but I have my fingers crossed cheap cialis online pharmacy 2008, 9, 635 638; Chrzanowski, AAPS PharmSciTech
TMG was from Cayman Chemical cialis online without prescription Ahmad N, et al
dissertation help uk
law dissertation writing service
uk dissertation help
kamagra order
buy cialis canada pharmacy There were only seven subjects with an FSH 16
coli induced UTI Amoxicillin dosage for strep throat in children is decided based on the result of a throat culture and rapid strep test cialis generic buy The best mechanical and electrochemical properties correspond to the use of dialkylphthalate as plasticizer
Regimens are intravenous q3 weekly for six to eight cycles, typically lasting almost six months where to buy cialis online forum
McCartney CR, Prendergast KA, Chhabra S, Eagleson CA, Yoo R, Chang RJ, et al tomar levitra es peligroso Up your oncology team found in the past menopause
There are many couples in their twenties and early thirties who are married and committed to each other, but just don t want children yet women viagra The bone scan showed radioactive concentration in the tenth and eleventh thoracic vertebrae, indicating the appearance of bone metastasis at these sites
To ensure the genotyping results were analyzed in the Thermofisher Cloud application cialis daily Give him a little more time, and he will have the confidence to fully recover
best online casinos for real money
online casinos us
sign up bonus no deposit casino
order sildenafil 100 mg pill
Cells were seeded in triplicate into cell culture dishes 1000 cells well cialis pills Expression of TrkB on mesenchymal cells was confirmed using a TrkB Cre Rosa26TdTomato mouse, which successfully identified platelet derived growth factor receptor О± PDGFRО± cells with increased TrkB expression Fig
a Western blotting for expression of cell cycle regulating proteins in parental and fulvestrant resistant CAMA 1, MCF7, HCC1428, and ZR 75 1 cells after treatment for 24 h with 100 nM fulvestrant F or DMSO control F cialis professional
HER1 and HER2 were co precipitated with Src in T47D S5 and the fulvestrant resistant cell lines, and the levels reflected the expression in total lysates best price cialis PubMed 29494050
Good luck in getting your pain under control what does viagra do for men
pharmacie de garde aujourd’hui crepy en valois pharmacie argenteuil simply pharmacie ville angers , pharmacie auchan ales pharmacie tourcoing . pharmacie de garde aujourd’hui lapalisse pharmacie bordeaux rue fondaudege pharmacie place imbach angers therapie cognitivo comportementale ille et vilaine .
medicaments biosimilaires grande pharmacie boulogne billancourt traitement bouton , medicaments rage de dents therapie cognitivo-comportementale avis , pharmacie lafayette agen pharmacie de garde marseille terrasse du port angers pharmacie des plantes Propranolol achat en ligne France, Vente Propranolol sans ordonnance Acheter Propranolol en pharmacie France Propranolol livraison France Propranolol livraison rapide. therapies cognitivo-comportementales (tcc) pharmacie uniprix jean beaulieu
Briefly, BM stromal cells were cultured in long term culture medium M5300 with 10 6 M hydrocortisone both from StemCell Technologies cialis
Rituximab in refractory autoimmune bullous diseases walmart priligy
Second, the literature search was restricted to studies published in the English language, which might have introduced a language bias does viagra help with premature ejaculation
finasteride buy online In some embodiments, R 1 is NO 2
Hormone therapy may actually help the heart in some respects for newly menopausal women, a randomized trial showed, although the impact on hard outcomes like stroke and breast cancer still remains to be seen male viagra before and after size
A total of 605 women aged 40 to 80 years who self reported a most bothersome symptom of dyspareunia and had a diagnosis of vulvar and vaginal atrophy were randomized to take a once daily dose of ospemifene n 303 or placebo n 302 for 12 weeks cialis without prescription Total amygdala histamine, t 13 3
Headaches and nausea were also reported online generic cialis This sequence may well require several months, a period considerably longer than the 6 week time span of the present study
voyage levitra Place a sterile 100 Ојl microcapillary pipette at the canthus of eye
dissertation writing uk
tips for writing dissertation
how do i write a dissertation
buy sildenafil 100 mg sale
5 mg cialis generic india I am unsure because it isn t truly designed for infertility use and since Clomid worked last time, why wouldn t it work this time
Complications of Transurethral Surgery liquid viagra drink
where to buy cialis online forum Next divide by the concentration of metoclopramide
viagra before and after pics As shown in Figure 3A, both the number and the size of the clones were decreased upon induction of SOX9 expression, which is consistent with the SOX9 induced inhibition of cell growth potential described above
Make sure to put a towel between your skin and the pack so that you don t irritate your breast tissue viagra vs tadalafil
Diuretics, calcium channel blockers, and ACEIs are first line drugs that can be used, although it might be best to limit use to drugs with breastfeeding safety information buy cialis online safely
Table I Patient characteristics priligy kaufen 2015; 30 88 96
As for rechallenge of the offending drug, it is usually suggested that, if necessary, tamoxifen be resumed temporarily at a lower dosage in tamoxifen induced hypercalcemia generic for cialis
Her indomethacin should be stopped and her hydrochlorothiazide put on hold finasteride prescription floroda 1998; Katoh, 2003; Shi et al
online gambling reviews
best online casino reviews
mobile casino sites
purchase kamagra generic
Trends point toward less use of antibiotics and less emphasis on surgery, all of which brings improved patient outcomes buy liquid cialis online
Other rare pelvic lymph node stations that can be seen are inguinal and in the deep portion of the obturator canal, following the obturator nerve path to the beginning of the thigh Fig 17 generic cialis 20mg Kasey, USA 2022 06 27 02 34 48
In our cohort, 21 hair loss propecia
The pulmonary arterial pressure decreases as the LV function improves cialis online cheap
propecia vs rogaine Some females may have frequent episodes of vaginal bleeding, while others may only have a few sporadic episodes
Karl could vaguely feel that Zhou Qing s mental power should be much stronger than his own, either low level valsartan recall companies 7 digestive issues and high blood pressure or medium level 7 cialis without a doctor’s prescription 5 times 2011 core earnings
pharmacy sell viagra Suissa S, Suissa K, Hudson M
Elises smiled wryly, I don t i accidentally took two blood pressure pills understand it because I don t understand viagra effects on women Arterial pH, PaO 2, and PaCO 2 values just before 0 and 30 min after the onset of noninvasive ventilation
cichoracearum, which is consistent with the speculation that cell death contributes to resistance against biotrophic pathogens 79 levitra annonce
phd dissertation peer reviewing help
dissertation research and writing
what is a dissertation paper
order kamagra 100 mg pill
119 Exposure can be reduced by choosing toxin free cosmetics and avoiding PVC plastic buy cialis online cheap
The Messenger of Allah PBUH said, Whenever someone greets me, Allah returns the soul to my body in the grave and I return his greeting best site to buy priligy As compared to placebo, tamoxifen led to a notable reduction of the total cholesterol TC WMD 23
cialis tadalafil Muniz dished to FOX411 about his big career changes and growing up in the spotlight
This can be achieved with a gram stain that lacks gram negative diplococci or by any negative gonorrhea test culture, nucleic acid testing, among others generic propecia online
Awesome blog post.Thanks Again. Keep writing.
kamagra order online
cheapest cialis available Most IOT projects start with a use case and a technology plan
49, respectively P trend 0 cialis buy online usa
buy cialis online using paypal The purpose of this drug profile is to examine the available literature on the trans- isomer enclomiphene
In contrast to this study, Golas et al how long does viagra take to work
What is titanium dioxide prix medicament levitra
cialis for sale No statistically significant difference was seen in the pneumothorax and chest tube insertion rates between the groups 28
An esential oil to balance blood sugar tadalafil cialis I was worried that if it was tubal, I was at risk of my fallopian tube bursting and losing it
Most of the time, the following remedy NM Crisis Line what to do about acute high blood sugar methods are suggested to do at house yourself Having a sugary drink or snack might help increase blood sugar levels and balance out blood sugar knife party remox and what to do about acute high blood sugar enhance any signs Even why check kidney function for blood sugar a small juice of juice or sweets can improve weak point and similar symptoms For these with low blood sugar levels, administration and therapy is a little simpler to do your self If you find your blood sugar is simply too low Normal Blood Sugar Levels Chart can guaifenesin raise blood sugar and you discover signs, at all times search medical attention cialis online generic You can get the shots together, one in each arm, Johansson said
00, esv057 2015 safe cialis online
Some 75 percent believed the situation would not improve in the next 12 months order priligy online
win money online
casino free bonus
online gambling reviews
buy sildenafil for sale
where to buy priligy usa Twenty seven surgically resected specimens of pancreatic cancer tissues were obtained from patients admitted to Kyoto University Hospital
buy cialis online europe Figure 3 shows Na changes after infusion of varying volumes of saline with varying sodium concentration predicted by formula 7
buy levitra 10 mg What level bed acuity is appropriate
buy cialis with paypal This medicine is well- tolerated and common side effects include hot flashes, breast tenderness, abdominal pain and nausea
street value of viagra Cell apoptosis was analyzed using the Annexin V Fluorescein Isothiocyanate FITC Propidium Iodide PI Apoptosis Detection Kit BD Biosciences, Franklin Lakes, NJ, USA, according to the manufacturer s instructions
9951 Caco 2 permeable 0 levitra generique posologie Dyspnea is commonly encountered by more than 50 of patients with advanced cancer in the terminal stage of their disease, and often it is not well controlled 1 3
dissertation express
premium dissertation writing service
dissertation help leicester
sildenafil order
This is the time between ejaculation and the moment you can get an erection again woman taking viagra Modulation of Cys loop receptors by steroids is of physiological and therapeutical relevance
Just looking to see if anyone has combined natural supplements along with clomid to increase progesterone and help possibly to O buy cialis online reviews Third round I did IUI I had 2
Children of control group 36 eyes received standard treatment in a complex with the electrical stimulation viagra kamagra 100mg
Authors Thilde Terkelsen, Francesco Russo, Pavel Gromov, Vilde Drageset Haakensen, SГёren Brunak, Irina Gromova, Anders Krogh and Elena Papaleo cialis from usa pharmacy Reports of clinical benefit of plitidepsin Aplidine, a new marine derived anticancer agent, in patients with advanced medullary thyroid carcinoma
Many young patients are currently being treated with imatinib, and they frequently face the dilemma of conception and pregnancy while receiving imatinib does cialis work better than viagra
The Hypophyseal Growth Hormone Nature and Actions cialis vs viagra Despite clinical advances in the treatment of KIT PDGFRA mutant GIST, similar progress against KIT PDGFRA wild type GIST, including mutant BRAF driven tumors, has been limited by a lack of model systems
trifluoperazine and artemether lumefantrine both increase QTc interval green viagra pill
Collectively, single cell RNA sequencing implicates TGF ОІ signaling and Klf4 overexpression as potential upstream drivers of SMC modulation could viagra treat covid
real money online slots
american online casinos
real money no deposit casino
buy sildenafil without prescription
Apoquel Oclacitinib Drug Interactions and Warnings buy cialis 20mg finast differin restorative night moisturizer reviews We live in a small rock in the north Atlantic, and we wouldbe under water were it not for very clever people in governmentand the revenue who made tax competitiveness a central part ofIrish economic life
Trends in acute myocarditis related pediatric hospitalizations in the United States, 2007 2016 cialis pills
5 to 25 mg tablet by mouth once daily for hypertension and a 50 to 100 mg tablet by mouth once daily for edema buy cialis online uk
I am now on my 3rd cycle of clomid TI cialis generic reviews MCT induced pulmonary hypertension in rats
acheter levitra generique cialis 3 70, which represents the case of the community hospital examined in the present study
therapies unite pharmacie ermont pharmacie avignon rocade , therapies for anxiety pharmacie de garde eure . therapies journal pharmacie de garde aujourd’hui strasbourg pharmacie de garde issy les moulineaux therapie cognitivo-comportementale clermont ferrand .
daily cialis online PMC free article PMC8108854 PubMed 21896142
cialis dosage She was very food motivated and never missed a meal
These tumors can arise in previously irradiated sites or as a second malignancy in patients with retinoblastoma natures viagra
getting help online
dissertation review
writing methodology for dissertation
order generic sildenafil 100 mg
clomid forsale Zheng YY, Lan YP, Tang HF, Zhu SM
cialis online generic February 20, 2020 at 12 51 pm
viagra liquid Answer Why don t you want too
AIs anastrozole is a drug in that group block the action of an estrogen producing enzyme called aromatase cialis online The young giant was a head taller than the elf riding on the back of the white tiger
Only 10 women of the group with a salpingo oophorectomy passed the time point at which the first PPSC case occurred in the group of women with a bilateral oophorectomy where to buy cialis online forum
s all I needed cheap cialis online
Use of NSAIDs, including CATAFLAM, during the third trimester of pregnancy increases the risk of premature closure of the fetal ductus arteriosus cheap cialis no prescription
Prior chemotherapy for early breast cancer had been given to 49 propecia generika 1mg
Smith, the main limitation of the study was that medication adherence was measured during a routine clinic visit and the researchers cannot be certain that each woman attending the clinic was still taking their medication viagra or kamagra 47 year old man developed jaundice 4 weeks after an initial cycle of cisplatin bilirubin 2
where can i buy cialis on line I blame my self for all of this
CSK is a nonreceptor protein tyrosine kinase that phosphorylates residues on the c terminal end of Src kinase family members, rendering them inactive propecia on sale
online casinos usa
real cash online casino
online casino games that pay
kamagra 100 mg us
azithromycin alcohol Treatment options are summarized in Table I
Indeed, conclusions drawn need to be carefully interpreted legit cialis online
In comparisons of the two drugs in such patients the desired effects were similar and the incidence of adverse effects was essentially the same 78 c buying cialis generic
They find 2 sacs viagra alcohol
38 lower at 98 generic propecia cost
Their vision improves to the point where they don t have to wear corrective lenses any longer viagra daily Your purchase helps a good cause
Various vitamins can also be included in the compositions of the present invention where to buy female viagra pill
propecia online com 20 E2 AD 90 20Viagra 20Femenina 20Barcelona 20 20Ist 20Viagra 20In 20Frankreich 20Rezeptpflichtig viagra femenina barcelona That man is Lucas Mads Mikkelsen, a caring kindergarten teacher, loving father and loyal friend
dissertation help service binding
what is dissertation
doctoral dissertation help
order kamagra 100 mg
thefeedback momcloud floridacharter bzid newmanrealty zabra hrbook creditmonster cablecarriers greenfusion governmentreview steeltraders miceguide free tarot reading honeybook retailkit rentacloud multinetworks noteables buffalolaw generic cialis for sale Signs of disease often don t emerge for five to six weeks after the bite, and the signs vary widely and are notoriously vague
According to the United States Department for Agriculture database, the juice from one lemon contains around 30 mg of vitamin C order propecia online
pharmacie thionville pharmacie yffiniac pharmacie leclerc yvetot , pharmacie rouen medicaments rhume . pharmacie ouverte montpellier pharmacie en ligne jean coutu therapie de couple bande annonce pharmacie bordeaux ginko .
therapie cognitivo-comportementale montreal produits non medicamenteux medicaments vitamine d , therapies biologiques pharmacie centrale , traitement lombalgie pharmacie de garde aujourd’hui saint brieuc grande pharmacie avignon nord Product Design Suite Ultimate 2017 bon marchГ©, Equivalent Product Design Suite Ultimate 2017 logiciel Equivalent Product Design Suite Ultimate 2017 logiciel Meilleur prix Product Design Suite Ultimate 2017 Acheter Product Design Suite Ultimate 2017 en France. therapie comportementale et cognitive crise d’angoisse pharmacie tarot avignon
generic cialis online europe Descriptive and quantitative data sub analysis
Bambuterol raises high density lipoprotein levels in patients with hyperlipidaemia cialis coupon
Hypoglycemia Sugar Symptoms pfizer levitra cialis It s a fair bet, then, that along with heart benefits, adopting a fitness regimen will give you some cancer protection as well
can you buy priligy in usa They may be able to recommend an alternative medication
1995 63 M M L M H M 41 Seracchioli R et al buy viagra Data were analyzed by one way ANOVA with Holm Sidak Multiple comparisons test
A couple things is azithromycin an antibiotic 1 It was initially reported to the WHO on December 31, 2019
Florencio xwWjjQTNwIMBlIlSvc 6 27 2022 cialis 20mg price
I m drinking a vegetable juice buying cialis online There is no detectable water maintenance, so the mass picked up throughout a cycle of Trenbolone will be hard and characterized giving fat levels are low enough
where to buy cialis online safely Overall I will be flying any airline but this one from now on
An adult treatment course of Malarone is 1, 000 mg of atovaquone and 400 mg of proguanil daily for 3 days buy cialis on line Tetracyclines should not be used in pregnancy because of staining of teeth and potential hepatotoxicity
buying cialis online usa Sertraline Zoloft can increase a chemical in the brain
bingo casino online
casino online bonus
super slots casino
buy sildenafil 100 mg online
cialis 20 mg Still, Sommerer et al
buy cialis generic online Active S100P residues that interact with estrogen receptor pink based on molecular modeling
6 Center for Regenerative Medicine, The Abigail Wexner Research Institute at Nationwide Children s Hospital, Columbus, Ohio propecia over the counter
The cells were harvested and centrifuged at 2000 rpm for 5 min levitra pour femme
Brand Name Tcypion Manufacturer Shree Venkatesh Packaging Type Box Packaging Size 1 X 5 ampoule Strength 250mg Form Injection safe cialis online
cialis on line When cycled together, fat loss, muscle gains and strength will reach new levels as opposed to running a Winstrol- only cycle
Try using those 3 phrases when you re writing headlines for your video memes or any other content that you put on Facebook cheap cialis online pharmacy
They claim to follow strict pharmaceutical guidelines and protocol when producing peptides levitra en generique Two weeks after randomization, the average frequency of premature ventricular contractions was 266 412 per hour in the placebo group, and it did not change significantly thereafter
These findings provide robust evidence that estradiol induction of the 5 HT 2A R and the SERT in brain is mediated by nuclear estrogen receptors canadian pharmacy cialis Profs File Amici Curiae Seeking En Banc Rehearing of Second Circuit Pharma Reverse Payment Antitrust Decision
online casinos with no deposit bonus
no deposit bonus online casino
real money casino
sildenafil 100 mg oral
Mattarollo SR, Loi S, Duret H, Ma Y, Zitvogel L, Smyth MJ cheapest cialis online
Chronic kidney disease and sudden death strategies for prevention buy cheap cialis online This in turn facilitated rapid cloning and sequencing of genes encoding a number of polyketide synthases PKSs
Demographic and Clinical Characteristics of Women With MMR Gene PVs and All Women Undergoing Multigene Panel Testing cialis without a doctor’s prescription Thirty one patients underwent resection of the primary tumor, one refused resection
where to buy female viagra cialis sildenafil biogaran 100 mg avis Campaign funds are supposed to be used only for matters related to the candidateГў s campaign or official business, but the law is vague enough that itГў s difficult to say whether WeinerГў s use of the money for a fake Гў investigationГў would be considered improper, said Bob Biersack, a longtime Federal Election Commission staffer who is a senior fellow at the nonpartisan Center for Responsive Politics
Tamoxifen inducible system In the absence of tamoxifen, Cre ER binds with Hsp90, and is cheapest cialis available secondary hypogonadism even though the apparent injury had been quite minor
pharmacie leclerc douai pharmacie garde autour de moi pharmacie de garde marseille 20 juillet , une pharmacie Г proximite pharmacie de garde aujourd’hui dunkerque . xpanded therapies ventura pharmacie moizard amiens xena therapies red wing mn pharmacie aix en provence dimanche .
therapies comportementales et cognitives application pharmacie leclerc frouard pharmacie carrefour beaulieu nantes , traitement infection urinaire therapies used in psychiatry , pharmacie beauvais saint jean pharmacie volembert argenteuil pharmacie de garde aujourd’hui toulon Prandin sans ordonnance prix, Ou acheter du Repaglinide 2 mg Cherche Repaglinide moins cher Acheter Repaglinide en pharmacie Suisse. pharmacie angers ouverte pharmacie de garde aujourd’hui tampon
clomid pills for sale We usedCox proportional hazards models with inverse probability of treatment and censoring weighting to estimate hazard ratios HRs with 95 CIs comparing new users of aromatase inhibitors with new users of tamoxifen for each of the study outcomes myocardial infarction, ischemic stroke, heart failure, and cardiovascular mortality
Diuresis in the inflammation of fluid and ambulatory setting can happen priligy without prescription So far, selective prostaglandin agonists have been applied in a way similar to the BMPs
viagra cefaclor capsulas 500 mg para que sirve McAfee said versions of the malware have infected many websites in an ongoing attack that it calls Operation Troy because the code is peppered with references to the ancient city how long do the effects of viagra last
cheapest cialis available This oil is also commonly called black cumin seed oil
I will give the prosecution everything they need to put me away for a very long time acheter levitra par internet
q6h 6 days starting 24 hr before carboplatin, metronidazole 750 mg m 2 p buy finasteride
what does female viagra do In patients receiving Tamoxifen Mylan for breast cancer, the decision to re start Tamoxifen Mylan should be made with respect to the overall risk for the patient
Electrolyte imbalances often associated with active fistulous losses must be carefully managed online pharmacy finax rifabutin will decrease the level or effect of efavirenz by affecting hepatic intestinal enzyme CYP3A4 metabolism
best welcome bonus online casino
free bonus slots
best casino deposit bonus
purchase kamagra online cheap
Sterols from Equisetum arvense cialis for daily use cialis ivermectin tablets usp ivecop 12 uses She said I suspect West Brom received legal advice that advised them they can only hike rates for the more sophisticated investors; hence their letter says the hike only applies to landlords with more than one property
Do you know any drugs besides adderall that increases brain function prix du levitra 10 mag More recent data now show an OS benefit in patients switched to anastrozole and exemestane compared with continuation of tamoxifen 18, 20, 21
boutique levitra Assisted reproduction was widely accepted after prestigious scientific and religious bodies and organizations issued guidelines, which were accepted by concerned authorities in different Muslim countries
Check your blood sugar post prandial, thyroid- stimulating hormone, follicle stimulating hormone, AMH anti- mullerian hormone, prola buy cialis without prescription 5 million the previous year
Potentiation by extracellular dideoxyforskolin or tamoxifen persisted after intracellular application of the modulator and was not due to Zn2 contamination super viagra 200mg
Also, a reduction in marked proteinuria by RAS blockade or by diet is associated with a better renal outcome buy cialis online united states
Tony, USA 2022 05 20 02 11 29 generic priligy
I get hot flashes fr tamoxifen, but my newly started Lupron made them much worse viagra over the counter usa
kasino bonus
casino no deposit bonus
online casinos real money
kamagra 100 mg canada
D Agati G, Cabello EM, Frontzek K, Rushing EJ, Klemm R, Robinson MD, White RM, Mosimann C, Burger A priligy dapoxetine amazon
On the morning of Day 21 each participant returned to the clinical facility prior to dose administration and were confined to the facility until Day 22 to allow for the collection of PK blood draws and safety assessments cheap viagra 100
The longer that disease causing bacteria linger in the body, the more they disseminate, and as these microbes spread to tissues throughout the body, they can trigger a litany of symptoms is generic cialis available
9 g 237mL Liquid Topical 210 mL 300mL Liquid Topical 0 viagra and afib
levitra pantoprazole with domperidone uses Real estate mogul Barry Sternlicht s Starwood PropertyTrust Inc is planning to buy the management arm ofWaypoint Homes Inc to expand its single family rental business, Bloomberg reported on Tuesday, citing three people withknowledge of the deal cialis super active
In the control group no immediate transfusion, transfusion with 20 ml of whole blood equivalent per kilogram of body weight was triggered by the development of new signs of clinical severity, which included impaired consciousness prostration or unconsciousness, increased difficulty in breathing respiratory distress, hemoglobinuria grade 6 or higher in the current illness, or a hemoglobin level of less than 4 g per deciliter will customs seize viagra
free no deposit
best online casino for us players
casino games for money
buy kamagra pills
BMJ 5 23 1998; 316 7144 1563 1569 buy cialis online reviews Halo or halogen means fluoro, chloro, bromo, or iodo
real cialis online 1983 Jun; 97 3 437 45
A 58 year old postmenopausal women who had been using tamoxifen for 4 years after a surgery for breast cancer is presented with chronic pelvic pain 36 hour cialis online Lexapro provides sedative and antianxiety effects and reduces the risk of depression and depression- associated symptoms
The reason for adopting a 1 sided test was that exemestane was expected to have a detrimental effect on the bone what does propecia do
can you buy cialis online The classification of CKD is evaluated on the basis of the cause, kidney function glomerular filtration rate GFR, and presence and severity of albuminuria, patients with CKD may include those in CKD stages G1 and G2 with a GFR of 60 mL min 1
After all, it is a 19 Nor derivative and such compounds are known for increasing strength, aggression and performance in the gym how effective is propecia
us casinos online
best welcome bonus casino
online gambling real money
kamagra without prescription
Skin and subcutaneous tissue disorders Maculopapular and erythematous rashes, DRESS syndrome drug rash with eosinophilia and systemic symptoms, Steven Johnson syndrome, toxic epidermal necrolysis, erythema multiforme, onycholysis, discoloration of the nails, exfoliative dermatitis and photosensitivity have been rarely reported see WARNINGS buy cialis without prescription 29 31 We assumed that carriers of mutations who had ovarian cancer had the more favorable prognosis reported by Rubin et al
96 The initiation and process of labor is an important factor in this antenatal redistribution and absorption of lung liquid, 97 explaining, in part, the higher incidence of TTN observed after elective cesarean section online cialis If another recurrent VTE episode occurs after the first dose escalation, further dose increase or twice daily dosing of LMWH are reasonable options
5 times less than cyclosporine A 3 Ојg mL does propecia work
therapie kalash criminel pharmacie de garde wasquehal pharmacie leclerc vitry , pharmacie avignon pont des deux eaux therapie de couple vaud , pharmacie monteux becker traitement lyme therapie de couple limoges therapies alternatives pharmacie avignon le pontet therapie manuelle orthopedique .
pharmacie romains annecy act therapy online course pharmacie boulogne billancourt rue du chateau , therapie jungienne pharmacie annapurna annecy . pharmacie a.proximite pharmacie colmar therapie comportementale et cognitive doctolib traitement mononucleose . pharmacie cap 3000 pharmacie de garde muret act therapy online , therapie cognitivo comportementale liege pharmacie avignon place pie , pharmacie desorme annecy pharmacie intermarche pharmacie victor hugo boulogne billancourt Lopinavir ritonavir prix Suisse, Lopimune comprimГ© pas cher Lopimune achat en ligne Suisse, Lopinavir ritonavir prix Suisse Lopimune achat en ligne Suisse Lopimune livraison express Suisse. medicaments stress pharmacie huyghe amiens pharmacie bailly en ligne pharmacie republique pharmacie lafayette montauban , pharmacie gambetta argenteuil therapie cognitivo comportementale reims . therapies meaning pharmacie de garde therapie cognitivo comportementale geneve
lasix without a rx vasorum is an emergent parasite; initially notified by Serres in France in 1853 2, it is currently widespread in tropical, subtropical and temperate regions of Africa, America and Europe with a pattern distribution in bounded endemic foci 3, 4
The inner cells of the blastocyst become the embryo, which develops into the fetus cialis online prescription To examine the difference in myelin components, myelin fractions were isolated and purified from the brain and myelin specific proteins were examined Saher et al
brand name cialis online Recommended Products and Resources Click here to go to Dr
1942; 58 265 266 cialis on line After median follow up of 4
They also have the ability to treat malignancies by directly killing tumor cells is generic cialis available lipitor clindamycin mip a alkohol Importing a car to Russia involves paying a fee to cover the future cost of recycling it, a form of green tax
Unblinding was necessary in one case who developed a skin rash, suspected to be a reaction to the trial drug, and she was withdrawn from the study Fig discreet cialis meds
ondansetron and romidepsin both increase QTc interval online indian propecia He also trained the undefeated three year old champion male Norfolk and undefeated Asteroid
cabergoline para que sirve el betnovate crema For those not getting government subsidies, there could be a bit of sticker shock as prices range from 150 for the lowest tier individual policies to thousands for top tier family coverage, depending on the state what happens when a woman takes viagra I too am a quitter
no deposit bonus
win real money casino
no deposit bonus casinos
kamagra tablet
Elf guardian warriors were also invited to Furosemide Medicine the dinner, Their beauty made blood pressure meds otc these old gentlemen with gray beards at a loss, and does metimucil lower your blood pressure forgot blood pressure medicine greedy eyes wandered on their faces from time to time buy cialis online forum
cialis and viagra together 60 In studies of tamoxifen metabolism in women of known CYP2D6 genotype, investigators discovered that women carrying wild type CYP2D6 alleles metabolized tamoxifen to endoxifen, whereas women carrying mutant alleles were poor effectors of this conversion and experienced lower exposure to endoxifen
In this review we present cardiovascular concerns associated with contemporary, multimodality BC treatment and illustrate how current guideline recommendations apply to clinical cardiology and oncology questions best place to buy generic cialis online
Excited to start my first round of Clomid on Thursday but i ve been reading all over the internet the S E and how alot of women can t sleep at night while on it how expensive is viagra
purchase cialis online cheap We find that NFATC1 governs FLT3 ITD driven precursor cell expansion and transformation, causing a fully penetrant lethal AML
pharmacie d’urgence annecy pharmacie guynemer amiens pharmacie amiens burger king , therapie de couple st-jean-sur-richelieu pharmacie lafayette avignon vaucluse . generique spasfon comprime therapie act et pleine conscience therapie comportementale et cognitive hyperphagie pharmacie centrale brest telephone .
pharmacie universite le mans therapie comportementale et cognitive toulouse pharmacie de garde corniche marseille , pharmacie principale avignon des produits medicamenteux , pharmacie lafayette muret therapie de couple quand consulter pharmacie ouverte perpignan Estrace achat en ligne Belgique, Estradiol bon marchГ© Estradiol Estrace 2mg Estradiol prix sans ordonnance Estradiol achat en ligne Belgique. pharmacie auchan htp therapie de couple toulouse avis
The use of the AngioJet device was significantly associated with a lower chance of complete recanalization OR, 0 can you buy cialis online
online cialis pharmacy When latency is disrupted, infectious viral particles travel anterograde down the neuron and manifest as infection
Differences between young and elderly breast cancer patients were observed propecia without prescription
C Fgfr1 mice behavioral assessments shown weekly along body weight record generic cialis for sale
where to get female viagra uk BMI is positively associated with breast cancer risk in postmenopausal women and inversely associated with risk in premenopausal women 27
best free windows vpn
best vpn to use in china
free vpn connection
buy kamagra 100 mg sale
generic for cialis Boubaker A, Prior J, Antonescu C, Meyrat B, Frey P, Delaloye ABF
In general, current OCs resulted in the development of fewer follicular and correspondingly lutein cysts 23 buy cialis online us
buy online cialis Control group received the Placebo capsule Low dose group received 50, 100, and 200 mg of I3C High dose group received 300 and 400 mg of I3C
In the first series of studies, we compared the effect of resveratrol on ERE luciferase activity with four different cell lines MCF 7, T47D, LY2, and S30 cialis no prescription
Other measures include waist to hip ratio and waist circumference, which look at weight in your abdominal belly area propecia shedding Women with node negative, ER negative tumors experienced a nonsignificant increase in the receipt of chemotherapy alone from 1995 to 2000
pharmacie ouverte yutz pharmacie en ligne luxembourg pharmacie ico angers , pharmacie auchan nord therapies of schizophrenia , therapies breves plurielles pharmacie de garde sartrouville therapies breves systemiques pharmacie de garde aujourd’hui maubeuge pharmacie lafayette xxl pharmacie ouverte frejus .
pharmacie bailly chennevieres sur marne pharmacie homeopathie bordeaux therapies breves hypnotherapie , pharmacie homeopathie beauvais therapie cognitivo comportementale quimper . medicaments pour la tension pharmacie angers bressigny therapies the grocery pharmacie leclerc epinal . pharmacie lamirand amiens act therapy ottawa pharmacie en ligne pas cher , therapie comportementale et cognitive cholet pharmacie d’argenteuil , pharmacie grottes beaulieu pharmacie escudier boulogne billancourt horaires generique zovirax comprimes Tamsulosin livraison express France, Flomax prix France Flomax Tamsulosin 0.4 mg Ou acheter du Flomax 0.4 mg Flomax achat en ligne France. therapies comportementales et cognitives en anglais pharmacie herboristerie argenteuil therapies home pharmacie amiens pierre rollin pharmacie bourges centre , therapie jalousie king’s college therapies . pharmacie beaulieu et couillard pharmacie drive beauvais pharmacie bailly bruxelles
cialis 5 mg For a summary of research studies on soy for menopausal symptoms, visit the Breast Cancer Research section
Louis, MO and dissolved in 100 ethanol at a stock concentration of 10 mg ml; the stock was further diluted in PBS and or culture media before addition to cells in culture buy cialis 5mg What about chemo
Feldmeyer, L buy cialis canadian
generic cialis from india Pexidartinib exposure
buy cialis canadian PMID 16257405
0 Insomnia A A 5 how to get a free trial of levitra Retroperitoneal fibrosis is generally idiopathic, but can also be secondary to the use of certain drugs, malignant diseases, infections, and surgery
Hypercalcemia occurs in 10 20 of cancer patients, usually those with advanced or late stage cancers propecia vs rogaine This was a randomized, double blind, placebo controlled, 15 day repeat dose study, with a single dose escalation stage, to establish the pharmacokinetics, safety, tolerability and effects of the Hoodia extract in healthy male subjects
no deposit on line casinos
free welcome bonus no deposit required
casino no deposit
sildenafil oral
nolvadex for sale usa In some embodiments, the reservoir comprises a deformable wall that is adapted to actuate flow of the composition when deformed such as those described in patent applications WO9527569, WO9615045 or U
Trials were repeated four times per day with intertrial intervals of 30 min for 2 d buy real cialis online
prandin omeprazole auxiliary label This really was my dream, and it s been such a gift to have that dream come true levitra seguridad social
Justin was a big Texan football fan, Drury explained azithromycin 250 mg
However, the number of drug shortages recognized by the FDA has been increasing each year since 2006 cialis 40 mg The current reported incidence of ILD is approximately 1, based on an FDA review of over 500 cases, although this estimate may be low, given that the drug is utilized for advanced lung cancer and it may be challenging for the clinician to distinguish between erlotinib toxicity and advanced NSCLC complications
It s a pity that everyone on Qiu Ding has extraordinary strength and profound skills, and has already listened to the conversation of several people without missing a word levitra dosage en france It correlates with organ failure and poor prognosis
paroxetine, fluoxetine, quinidine, cinacalcet or bupropion should whenever possible be avoided during tamoxifen treatment buy priligy in usa
Is anastrozole superior to tamoxifen as first line therapy for advanced breast cancer generic cialis Susan s scans specifically established that Susan did not suffer from cancer in that three month period
However, research has now shown that there are several other pathogens that may be involved, including adenovirus, canine respiratory coronavirus, herpesvirus, distemper, influenza, mycoplasma, and streptococcus zooepidemicus, to name a few how effective is propecia Estimates are that it would take 5 g kg body weight intravenously to cause convulsions in a patient
best free vpn for firefox
vpn best value
avg secure vpn
order kamagra online cheap
Lymphomas are cancers of lymphocytes how to get propecia If you dont gain control over the other forms of relaxation and reduction with Levodyn the all natural herbal remedy
kur mot urinvägsinfektion generic propecia for sale 2009 Jul; 44 Suppl 2 316 9
A rapidly growing and remarkably consistent evidence base indicates that many markers of inflammation are higher in antiretroviral treated adults than in age matched uninfected individuals 30, 31 cialis generic reviews It should be noted that based on a review of case reports, there is a complex array of characteristics that appear to be similar to fetal alcohol effects
and glyceraldehyde 3 phosphate dehydrogenase GAPDH; 1 2000, 2118; Cell Signaling Technology Inc buy cheap generic cialis uk
The scope of the article under Citizendium rules, is something that editors should be expected to decide cialis 10mg
The number of clomiphene supposed to be taken was calculated as the cycles of treatment multiplied by 1 or 2 or 3, depending on their treatment response generic cialis tadalafil Table S1 shows the IC 50 values of free TAM, carrier alone and TAM loaded micelles
In Gufeng City, Xuanxian mandarins and type 2 diabetes cultivation base is already the top powerhouse, and only the patriarchs of several major families have this cultivation base cheapest place to buy cialis Met, before hitting the hay
viagra lowers blood pressure Conditioned media induced a concentration dependent increase in HASMC viability Figure 6E
best free vpn for torrenting
free vpn download
what is the best vpn service
sildenafil order
99 Buy Now 2 Testo- Max Sustanon 250 59 cheapest place to buy cialis These are not all the possible side effects of Halcion
Depending upon the nerve s involved and other factors, peripheral neuropathy may produce symptoms that relate to motor, sensory, and or autonomic malfunction cialis How Anadrol works inside the body
buy cialis generic online Telemetric transmitters PhysioTel PA C10, Data Sciences International were implanted subcutaneously, with the sensing tip placed in the aorta via the left carotid artery
buy cialis cheap In our previous study, we reported a dual targeting drug carrier based on the PEGylated fourth generation PAMAM dendrimers with DOX entrapped in the interior
p p A or versus CHO cells B in the same treatment group order cialis online Ellis MJ received consulting fees from Abbvie, Sermonix, Pfizer, AstraZeneca, Celgene, NanoString, Puma, and Novartis, and is an equity stockholder, consultant, and Board Director member of BioClassifier, and inventor on a patent for the Breast PAM50 assay
pharmacie annecy intermarche pharmacie leclerc epinal pharmacie de garde aujourd’hui a koumassi , grande pharmacie avignon nord pharmacie lafayette bourges , therapie de couple liege pharmacie lafayette boulogne billancourt therapie de couple imago pharmacie en ligne vaccin atma hypnose et therapies breves courroux des produits medicamenteux .
pharmacie autour de moi pharmacie beauvais Г falaise traitement sclerose en plaque , pharmacie beaulieu les loches medicaments cystite . therapies breves rennes pharmacie ouverte evreux pharmacie talence pharmacie de garde saint etienne . act therapy cards master pharmacie industrielle bordeaux pharmacie leclerc tours nord , pharmacie de garde gard medicaments usages , pharmacie lafayette dans les yvelines pharmacie bordeaux gare st jean pharmacie de garde aujourd’hui essonne Autodesk Advance Steel 2022 achat en ligne Suisse, Equivalent Autodesk Advance Steel 2022 logiciel Autodesk Advance Steel 2022 prix Suisse, Autodesk Advance Steel 2022 achat en ligne Suisse Acheter licence Autodesk Advance Steel 2022 Autodesk Advance Steel 2022 achat en ligne Suisse. pharmacie auchan city pharmacie bailly paris 16 traitement de texte mac pharmacie amiens carrefour pharmacie de garde aujourd’hui nc , medicament generique comprime pharmacie rue saint pierre beauvais . pharmacie lafayette nimes pharmacie marivaux amiens pharmacie de garde xonrupt longemer
buy cialis pro Heath FSpQzcEVKJ 6 17 2022
viagra cialis online Ferguson had to be in control
Prevention of preterm delivery nifedipine or magnesium sulfate cialis buy online usa Treatment that comes after surgery or another initial treatment is called adjuvant treatment
Subjects were provided with non investigational products, that they were required to use alongside their treatments for the duration of the study best price cialis
These study findings highlight important elements for enhancing integrated care at the GP Hospital interface and can inform integrated healthcare policy in Ireland and elsewhere buy finpecia online The ingredient is made to break up mucus, but if taken while you ovulate it can make your CM more compatible with sperm
The following morning you will arrive at the hospital where the tubal reversal is scheduled and you will meet the anesthesiologist to review with you the General Anesthesia that is used for the tubal reversal procedure lasix and sodium The transfer of the reaction mixture is completed with a 1 methyl 2 pyrrolidinone 0
Parma in combination with an IV anticoagulant and clopidogrel ACCF AHA SCAI Levine 2011 buy cialis 20mg
While minimizing weight gain is important, clarification of its impact on survival and recurrence outcomes is of critical importance buy cialis online using paypal My MO at that time asked me if I had wine, and I said yes, and she laughed and said abstain and get tested in a week or two
It is given as directed by your doctor, usually over 30 to 60 minutes every day or every other day for a total of 3 to 5 doses cheap cialis
casinos online usa
real money casino games
no deposit casino bonuses
buy sildenafil 100 mg without prescription
viagra will cephalexin kill staph infection The study did not find increased obesity rates until the third generation cialis buy online The release of the ATAC data led to the opportunity for patients to switch therapy before receiving the full 5 years of prescribed therapy
generic 5 mg cialis 2004, 34 847 59
buy cialis on line Best1 shRNA expressing astrocytes showed almost complete elimination of the sensor NMDAR current, which was fully reconstituted by a co expression of shRNA insensitive form of mBest1, whereas co expression of shRNA insensitive mBest1 W93C showed no recovery Figure 2M and 2N
I bet if there was oil in syria there would be overwhelming action taking place there does daily viagra lower blood pressure
Primary Research best site to buy cialis online Li R, Gui Y, Lu L, Hao G, Cai Z
cheapest cialis 20mg Hyung Geun M
Lower iCa and K were associated with longer QTc interval independent of potential confounders QTc difference 8 propecia medication The modern equipment used by takes very accurate measurements of the eyes, even many years after having undergone LASIK surgery
These headaches come with a sort of numbness, and now she notices some other things that aren t as they should be how to buy priligy in usa Garlic in any form Grapes or grape seed grapes have been shown to cause kidney damage in some pets; however it is not known which part of the grape causes the damage Any supplement that claims to boost immunity i
win real money online
online mobile casino
welcome bonus no deposit
buy kamagra 100 mg sale
The cause of preeclampsia is thought to involve release of a soluble fms like tyrosine kinase a vascular endothelial growth factor receptor from placenta leading to decreased bioavailability of circulating vascular endothelial growth factor and endothelial injury, decreased NO formation, vasoconstriction, and glomerular damage with endotheliosis hydroxychloroquine zithromax
generic cialis from india Magnani also suggested that when cancer returns, a biopsy should be done to see how the cancer has evolved, which may help guide treatment decisions
As you can tell, he s a genetic phenom by the lack of his understanding of this concept, but what he looks like, irrespective of that buy cialis online forum
She said, By Allah, I do not know what to say to Allah s Apostle cheap propecia online uk
business vpn setup
vpn pc free
best vpn for 2017
sildenafil 50mg cheap
Images taken from the flatmount shown in S1 Fig nolvadex dosage bodybuilding FUJIFILM Irvine Scientific
A few of the several further examples where the HPLC MS technique was successfully used for impurity and degradation profiling are listed here atomoxetine hydrochloride 183, palonosetron hydrochloride 184, bitespiramycin 185, eslicarbazepine acetate 186, thyroxine 187, griseofulvin 188, Z endoxifen 189, monoclonal antibodies 190, 191, nevirapine 192, azilsartan 193, trelagliptin succinate 194, bleomycin sulfate, tyrothricin, vancomycin HCl, bacitracin 195 and vonoprazan fumarate 196 levitra para durar mas
Avoid NSAIDs and laxatives buying cialis online reviews Systemic Enzyme Therapy 3 tablets 2 times a day on an empty stomach at least 45 minutes before meals with water
To identify the survival gene candidates, dataset 1 GSE42568 from Dublin City University Ireland was used as a training cohort consisted of 121 patients, 17 of whom were excluded due to normal breast tissue buy cialis online united states Previous studies have shown that clomiphene has antiviral effects against Ebola virus
Overactivity of the thyroid gland, called hyperthyroidism, can also cause sweating and flushing and is also one of the most overlooked causes of hot flashes at night, which is not menopause bluechew viagra Lovelace Scientific Resources, L
online real casino best online casinos usa no deposit online casino buying cialis online
Washington, DC AICR, 2007 cialis tablets for sale Clear and convincing argument that presents a persuasive claim in a distinctive and compelling manner
In metabolic acidosis, bicarbonate binds excess hydrogen ions, thereby decreasing the amount of measurable HCO 3 woman taking viagra
In the 90s, Americans relocated most of their factories to China to lower the costs of production how to buy priligy im 16 years old penicillin susceptible, and Cutibacterium spp
best vpn for ubuntu
vpn free pc
best firestick vpn
order kamagra 50mg generic
The next experiment was to test if chitosan could be added to PEG AM cialis online prescription Cells were then washed twice with OMEM inhibitor and placed in a 37 C incubator for 3 hours to allow entry to occur
During his 16 years on the faculty at the University of Ottawa, Dr buy cialis 5mg online
Women who received five daily subcutaneous injections of sepranolone exhibited significant improvement in PMDD symptoms compared with women who received placebo, and the medication was well tolerated 146 where to buy cialis Serious Use Alternative 1 entrectinib and vorinostat both increase QTc interval
For a business to show that they are different from their competitors, they should invest in custom signs and banners that will reflect your brand clearly levitra on line
is propecia safe I never felt rushed in any of my appointments
2019, both using self report and observed drug related symptoms such as vomiting and headaches as a measure of ADRs, reported no significant association between CYP2D6 polymorphisms and ADRs levitra venta Just wondering if anyone has noticed that their period after a Clomid cycle is heavier than normal
pharmacie auchan istres pharmacie de garde aujourd’hui vichy traitement johnson , pharmacie ouverte aujourd’hui traitement naturel infection urinaire , pharmacie bailly horaires pharmacie beaulieu laplante pharmacie lafayette lille pharmacie beauvais jeanne hachette medicaments en ligne pharmacie bordeaux place des grands hommes .
pharmacie auchan neuilly sur marne therapie de couple west island therapie cognitive comportementale yvelines , pharmacie cohen boulogne billancourt therapies comportementales et cognitives gironde . therapie par les arbres pharmacie leclerc horbourg wihr masques pharmacie boulogne billancourt pharmacie champfleury avignon . therapies comportementales et cognitives rennes pharmacie rue jean jaures argenteuil pharmacie boticinal avignon , pharmacie de garde limoges pharmacie bailly 78 , pharmacie auchan horaire pau pharmacie agroparc avignon act therapy explained Recherche Autodesk Building Design Suite Premium 2017 moins cher, Autodesk Building Design Suite Premium 2017 pas cher Ou acheter du Autodesk Building Design Suite Premium 2017 Ou acheter du Autodesk Building Design Suite Premium 2017 Autodesk Building Design Suite Premium 2017 vente en ligne. pharmacie brest rue de verdun pharmacie st serge angers fax pharmacie des ecoles argenteuil therapie act valeurs emploi pharmacien aix en provence , pharmacie ouverte midi annecy pharmacie neuville amiens . pharmacies in bordeaux therapie act pdf pharmacie horloge angers
real cialis online Thus, adjuvant WBI remains the standard of care after BCS in patients with early stage, low risk breast cancer
PubMed 20923473 propecia hk
Nonetheless, the addition of ovarian suppression to standard adjuvant therapy with tamoxifen or an AI improved disease free survival and improved freedom from breast cancer and distant recurrence compared with tamoxifen alone among the subset of patients who were at sufficient risk of recurrence such that adjuvant chemotherapy was warranted, they add buying cialis online safely Monitor Closely 1 ozanimod, leflunomide
bisacodyl how to flonase sensimist One group stormed into a Wal Mart and vandalized the store, causing a citywide tactical alert to be declared by police at 9 p levitra et pamplemousse
how many mg of viagra should i take These syndromes include the various types of pseudohypoparathyroidism 1a, 1b, 1c, and 2 and severe hypomagnesemia, which impairs PTH secretion and causes peripheral PTH resistance
no deposit casino online
no deposit bonuses
no deposit slots for real money
order generic sildenafil 50mg
dosage for tamoxifen Sleep disruption including
The synergistic effect of the combination is partly explained by the fact that the fermented soy increased pro apoptotic conditions in the cancer cells and raises the level of P21 in cancer cells cheap generic cialis
Another protein from the Top1 complex, FACT was found to be Important for Top1 binding to H3K4me3 which is essential for DNA cleavage and AID induced translocations 127 buy cialis online prescription
viagra connect near me Recently, the joint analysis of the two Phase III trials, the Suppression of Ovarian Function Trial SOFT and the Tamoxifen and Exemestane Trial TEXT, 36 reported opposite results
pharmacie bordeaux horaires pharmacie boulogne billancourt rue gallieni pharmacie lafayette halles , pharmacie charre annecy le vieux therapie act et toc , pharmacie oziel boulogne billancourt therapies familiales therapies digitales pharmacie leclerc istres pharmacie gare tgv aix en provence pharmacie des ecoles boulogne billancourt .
pharmacie de garde khemisset aujourd’hui pharmacie auchan st loup therapie cognitivo comportementale vaucluse , pharmacie homeopathique annecy therapie cognitivo comportementale isere . pharmacie ouverte nice pharmacie de garde wavre aujourd’hui pharmacie yerville xena therapies red wing mn . pharmacie aix en provence place de la mairie pharmacie mabilleau bourges therapies breves et outils pratiques , pharmacie ouverte fresnes pharmacie bailly henri , pharmacie beauvais jean rostand pharmacie homeo annecy therapie cognitive comportementale nord pas de calais Vente Proscar sans ordonnance, Vente Finasteride sans ordonnance Finasteride prix sans ordonnance, Vente Proscar sans ordonnance Acheter Finasteride 5 mg en Canada Finasteride 5 mg pas cher. pharmacie de garde aujourd’hui yvelines pharmacie de garde beaulieu sur dordogne pharmacie de garde haute loire pharmacie de garde marseille boulevard national pharmacie avignon intra muros , therapie de couple bruxelles pharmacie avignon cap sud . therapie cognitivo-comportementale ordre des psychologues pharmacie brest rue albert louppe pharmacie beaulieu sur dordogne
2011 Feb 10; 7 1 2 buy cialis generic online
Images were exported to Fiji 75 for final processing and assembly levitra genericos This year 2021, Streff et al 193 in a prospective trial to measure the change in blood estradiol levels in only 8 postmenopausal women with ER BC undergoing treatment with AIs when treated with vaginal estrogen preparation for their urogenital symptoms, found that there was no significant difference between the baseline and week 16 estradiol levels P 0
PubMed 7957546 cialis generic name
A solution containing hydrogen peroxide 0 cialis vs viagra
In this case, CRT might not offer the same degree of benefit as it did to patients in the clinical trials is viagra safe for women
Although I can not represent the Shangqing Sect, I can go back and persuade some of the elders where to buy cialis online It occurs where the skin has been exposed to the sun and so typically involves face, neck and upper chest
cheapest place to buy cialis Michel UhsOBFABAiNNv 5 21 2022
tamsulosin and viagra or non steroidal, anti inflammatory drug
does propecia really work No laboratory test or other clinical finding showed statistically significant differences between pre and post septal cellulitis
fastest vpn
dot vpn
best antivirus with vpn
It s okay, I have a kid cialis pills We both felt like we can ask any clarification questions and she would take the time to explain things
All potential occurrences of ONJ were reported as serious adverse events and centrally reviewed priligy dapoxetine
These food products have synthetic supplements to help increase their nutritional value and provide a year- round supply of folic acids via foods that have a longer shelf life safe place to buy cialis online 00 Multiple Allergies allergy to multiple agents 1 person, 10
casinos sites
top casino site
live online casino usa
cheap cialis generic online Bordeleau L
Seasons of struggle will happen even in the believing even when you can t see the promises yet generic 5mg cialis best price
Collectively, these data support our hypothesis of the functional role of HOXA5 in tamoxifen resistance by regulation of the PI3K AKT pathway real cialis no generic Discontinue buprenorphine if serotonin syndrome suspected
does viagra show up on a drug test 04 Additionally, in light of continued pressure on Japanese yen, which traded around high 90s to a dollar through most of the second quarter, Corning s gains from its yen hedges will be in focus in the coming earnings
setup vpn
best vpn for ipad
mexico vpn free
Dear Creative Practitioner, Did you also apply get doctor to prescribe azithromycin Tanaka T, Ikeda M, Okusaka T, Ueno H, Morizane C, Hagihara A, Iwasa S, Kojima Y 2008 Prognostic factors in japanese patients with advanced pancreatic cancer treated with single agent gemcitabine as first line therapy
buy cialis usa The glycoprotein molecules are composed of a main chain beta 1, 4 glucan with beta 1, 3 and beta 1, 6 linked side chains
2007 Sep; 72 3 208 17 viagra history
By using something like this at age 18, you can add 1 2 inches you would not normally have is generic sildenafil as good as viagra Shaun dcJnLjCRNoXVzYJAe 6 4 2022
blackjack real money
online casino game real money
casinos online usa
Patients with high BMI require a higher dose of ovulation inducing drugs cheap cialis from india
best vpn providers
open vpn
turbo vpn
For women 50 at the time of diagnosis, there were 29 cases among participants randomized to Fenahex tamoxifen citrate compared to 12 among women on placebo RR 2 buy cialis online usa
Cyst puncture cialis generic online Your eye doctor may advise you to use these at night, as they can make vision blurry
There are of course important instances where a patient will present with hypovolemic hyponatraemia in the setting of diuretic use or gastrointestinal losses finpecia from india online
online indian propecia We believe that such cases are not very rare and many similar conditions in nephrotic syndrome might have been overlooked
ER acts as a ligand dependent transcription factor, and ligand binding to the LBD results to activation of gene transcription, leading in the progression of breast cancer Takeshima et al canadian levitra Internal Medicine Podcast
gambling bonuses
online casino us
free bonus casino
A systemic antibiotic should begin early in the treatment to assist the body as treatment progresses cialis online purchase I hope you get a BFP this cycle
Salvador agDSoWjGoxmxLzAQc 5 20 2022 generic cialis for sale Under Florida law, Zimmerman cannot be found guilty if he was proven to have been protecting himself
buy cialis online The role of phytotherapy in treating lower urinary tract symptoms and benign prostatic hyperplasia
vpn software
vpn for business
best vpn service of 2022
online cialis pharmacy 6 The impact of endometriosis on oocyte quality has suggested by studies evaluating the donor oocytes of patients with and without endometriosis and implantation rates in recipients
The efficiency of the separation was confirmed independently by determining Pdx1 expression by qPCR in the mesenchymal and epithelial components of FACS separated cells J real cialis online
In all of these patients hydronephrosis gradually improved and no complications were detected during follow up viagra alternatives otc mock transfection reagent only
overnight cialis delivery Thus, HER 2 neu overexpression does not adversely influence, and may favorably influence, response to adjuvant oophorectomy and tamoxifen treatment in patients with ER positive tumors
best place to buy cialis online 4 was maintained throughout the 24 h evaluation period
But for me, kratom weight loss benefits are still underappreciated buy liquid cialis online Persistence over 1 year
com 20 E2 AD 90 20Obat 20Viagra 20Di 20Apotik 20Kimia 20Farma 20 20Viagra 20Na 20Drogasil 20Preco viagra na drogasil preco If China doesn t have the processing capacity then it hasto import the fuel directly, said Xiamen University s Li best otc viagra Safren, Jennifer S
best online us casinos
best casino reviews
casino welcome bonus
An absolute increase in disease free survival of 12 was noted at 3 years and that of 18 at 4 years in the trastuzumab group generic cialis for sale
2006 Jan Feb; 12 Suppl 1 S16 26 cheap generic cialis
cialis cost When ceftriaxone cannot be used for treating urogenital or rectal gonorrhea because of cephalosporin allergy, a single 240 mg IM dose of gentamicin, plus a single 2 g oral dose of azithromycin is an option
vpn buy account
express vpn download
best vpn for pubg
The previously reported VSD now had a velocity of 3 buy cialis online reviews
The NYHA classes include cialis pills
25 mg of a GnRH antagonist injection was administered on the day of trigger administration for oocyte maturation with the use of hCG how long does it take for propecia to work In studies, it seemed to particularly affect systolic blood pressure or the force that takes place when the heart pumps blood away from it
Joesph, USA 2022 05 21 01 43 52 cialis reviews In previous years, Mr al Assad has been seen attending them early in the morning
blackjack real money
what is the best online casino for real money
no deposit casinos
vpn ghost
surfshark vpn
zenmate vpn
Our online steroid shop sells official Alpha Pharmaceuticals also known as Alpha Pharma among bodybuilders and other world famous brands buying cheap cialis online This particular use is known as post cycle therapy
FГјrstenberger, B buying cialis online reviews Randal qiUEdRQzyzv 6 6 2022
The good pathways are 2 hydroxyestrone and 2 hydroxyestradiol levitra dosage pharmacie
7, and for the 7 patients presenting a third time, a third injection saved 1, 986 283 per digit, 14 propecia for sale in usa I started Tamoxifen in February of 2011
dapoxetine for premature PMID 19891251 Italian
united states online casino
mobile casinos
no deposit welcome bonus
The data presented are important in their support of the relevance of current and future clinical trials targeting interventions on oestrogen signalling pathways buy cialis generic online
Mary Tavares DMD, MPH, in Journal of Evidence Based Dental Practice, 2017 where to buy priligy
Expert Rev Cardiovasc Ther 8 793 802 priligy walgreens 94, and active treatment had no effect on change in eGFR over time treatment time interaction P 0
the raloxifene and arimidex are also very expensive compared to the tamoxifene online cialis pharmacy Estrogens are vitally important players in many physiologic functions in men including bone metabolism, cardiovascular health, spermatogenesis, cognition and sexual function 220, 221
gay dating scams
single gay dating site
gay dating apps 2019
Hartford, Olive Branch, and Donaghue Foundations cheap non prescription finasteride 5mg Healthy men produce 6- 8 mg testosterone daily, in a rhythmic pattern with a peak in the early morning and a lag in the later afternoon
buy cialis without prescription Lymph node involvement may occur with or without symptoms and signs resembling serum sickness e
In future studies, it will be important to assess our DA within a more diverse context, as measured across various demographic features, including culture, education, and socioeconomic status viagra drugs
buy sildenafil 50mg without prescription
buy real cialis online Helicobacter pylori eradication therapy improves atrophic gastritis and intestinal metaplasia a 5 year prospective study of patients with atrophic gastritis
They found FGF 23 levels were 22 lower in African Americans than in Caucasians generic cialis 5mg Low blood sugar in a 78 year old man after taking an herbal remedy containing nettle for BPH
Clinical experience with 99m Tc MAG 3, mercaptoacetyltriglycine, and a comparison with 99m Tc DTPA dapoxetina generico Inflammation resulting from either feed or disease is inversely related to growth and health Reference Klasing, Laurin and Peng 20
best place to buy cialis online forum But, seriously, I think that sometimes He really is too sporting and pushes the boundaries way too far
free gay dating apps
senior gay women dating sites
cruise gay dating
You re going to be fine buy cheap generic cialis uk Shoveling snow and cold weather are a dangerous combination
ШІЩЋШ§ШЇЩЋ ШЁЩђШєЩЏШ±Щ‘ЩЋШ©ЩЌ Ш№ЩЋШЁЩ’ШЇЩЌ ШЈЩЋЩ€Щ’ ШЈЩЋЩ…ЩЋШ©ЩЌ levitra 10 posologie
buy cialis 5mg Stabilized sulforaphane for clinical use Phytochemical delivery efficiency
Title of study See one, do one, forget one early skill decay after paracentesis training 49 Authors Sall et al buy cialis online in usa
Countless spies also took the opportunity blood pressure wont go down after medication to sneak in, set fire to poison, spread rumors and assassinate, and no Not to the extreme buy viagra cialis online
buy cialis on line The participant will be able to describe similarities and differences of newcomer LLP caregivers across various health systems
dating services melbourne
single free dating sites for sex
free se4x
can i buy priligy in usa 90 10 CENT SUPERFECTA 2 4 5 3 13
A list of assessments that need to be conducted when providing reversible contraceptive services to a female client seeking to initiate or switch to a new method of reversible contraception is provided Table 1 42 buying cheap cialis online I was on 100mg of clomid cd3- 7 resulted in 3 mature follicles 20 mm and 2 smaller 16 and 18mm which might not have released in time for the IUI
Silverstein Eye Centers buying cialis online safely
black gay dating sites
gay dating cites
free gay men dating sites missouri
fosamax ciprofloxacin dose for std Wendy Barclay, an Imperial College London flu expert, said it would be ludicrous to shy away from such studies buy cialis uk
cialis pills for sale The control tumor samples are colored blue, and the TF tumor samples yellow
5D, which also moderately increased survival Fig buy cialis generic online Double blind randomized controlled trials RCTs, which could be placebo controlled or head to head trials
Ralph, USA 2022 06 17 00 09 04 buy cialis online europe Following induction, cells were then further incubated at 37 C in 5 CO 2 for 48 h before bioluminescence analysis
date online site
single personal ads
dating services online
Thyroid hormones do not readily cross the placental barrier see Use in Specific Populations 8 buy cialis
Raymundo YsBRUexAvOjLXyI 6 18 2022 where to buy cialis online safely
priligy for pe Next, we classified groups of genes with similar expression profiles across the different genotypes and stages analyzed
Omg i cant even imagine having a heavy period for 10 days where can i buy cialis on line Alternatively, atovaquone proguanil 250 mg 100 mg is administered as four tablets to be taken daily for 3 days
However, in general, the H 1 R induces phospholipase C activation, inositol phosphate production, and calcium mobilization, via coupling to GО± q proteins buy 10 mg levitra online
Viagra use in pediatrics No prescription viagra reviews Viagra pris flashback buy cialis online without prescription Kruskal Wallis, p 0
is it safe to take viagra with beta blockers Purification of the crude material by flash column chromatography on silica gel 3 then 5 EtOAc in hexanes afforded acetate S 24 815 mg, 82 in 5 steps as colorless syrup
chat with singles
asian girl single
free women dating
viagra vs cialis After a control period of 3 minutes, CTZ was added at 30 or 100 ОјM and caused concentration dependent increases of Ca 2 i
36 hour cialis online 9 NaCl, IIET, Wroclaw, Poland
buy cialis viagra 145 Hospital Avenue Suite 205 DuBois, PA 15801 814 375 3910
propecia before and after quenched with saturated ammonium chloride, extracted twice with 100 mL EtOAc, washed with brine, dried over anhydrous sodium sulfate, filtered and concentrated in vacuo
I went to Lifang Liang, an herbalist and acupuncturist in San Francisco cialis professional Increase ovulation rates when compared with placebo or no treatment 33 Clomiphene Day 2 5 50 mg OD for 5 days traditional Progestin prescribed for lack of ovulation and cycle restart Increase by 50 mg for each cycle thereafter until response Upper limit at 250 mg
Chapter Three Tamoxifen and CYP2D6 A Controversy in Pharmacogenetics buying cialis online The prognostic and predictive value of the RS assay in women with ER PR LN ESBC was evaluated in retrospective analyses of the National Surgical Adjuvant Breast and Bowel Project NSABP chemotherapy tamoxifen trials B 14 and B 20 7, 9, 11 in the United States
Though, if diagnosed early and treated appropriately, breast cancer patients have relatively better outcomes than many other types of malignancies, it is difficult to reach accurate diagnosis and optimal therapeutic design given distinct patients morphological features and treatment responses 3, 4, 5, 6, 7 tadalafil generic vs cialis
order accutane 40mg without prescription
So chemical companies sell you both the cause and the antidote order cialis Rarely subcutaneous low molecular weight heparin
buying cialis online Innal hamda wan ni mata laka wal mulk, la sharika laka Here I am, O Allah, here I am
Harvested monocytes were identified for gating on the forward scatter side scatter plot amazon priligy
DoCoMo s first quarter operatingprofit fell 5 cialis with dapoxetine Free T assays based on analog displacement immunoassays are still widely available and used some positive results 71, but their reliability has been seriously questioned by some authors 72, 73
Hawes during bladder cystoscopy of chronic UTI patients she frequently sees pimples on their bladder surface tadalafil cialis from india
skip the game dating site free search
top online dating websites
free chat sites dating
buy cialis online Med J Malaysia 2003; 58 147 54 McKim et al Caffeine and its effects on pregnancy and the neonate
All mice were handled in strict accord with good animal practices, as defined by the Institutional Committee for Animal Care and Use, NIBS cialis 5mg online
renova ciprofloxacin 500mg for kidney infection Гў Well again I know itГў s a day to day thing so IГў m certainly hopeful itГў s not as bad as Sione PoГў uhaГў s, Гў said Rex Ryan, refereing to the former Jet lineman, whose back injury in camp last year affected his entire season cialis super active
Laetrile a study of its physicochemical and biochemical properties buy cialis generic online cheap
buy cialis online prescription Wallace pDYOrsKdTakp 5 20 2022
Cancer genome sequencing efforts have identified mutations in canonical splicing factors that include U2AF1, SF3B1, SRSF2, and ZRSR2 2 overnight cialis delivery
buy isotretinoin 10 mg
cialis on sale in usa After a pause, his eyes became sharp, and then he said indifferently However, I also want to see how far you new blood pressure chart 2022 can be entangled with this beast
Bone is one of the most frequent sites for metastasis of breast and prostate cancer can i buy cialis without a prescription
Arnoldo psOVlLSladMDHMjQkU 5 21 2022 generic cialis online pharmacy
gay dating sites sanford nc
newest gay dating site
browse gay dating ads
vardenafil india bay Do not take the doxycycline capsule in piecemeals
Promote healthy glucose levels and healthy sugar metabolism By assisting the pancreas in production of insulin cialis no prescription Methods Women who had undergone hysterectomy were consecutively enrolled in the placebo controlled, randomized, double blind Breast Carcinoma Chemoprevention Tamoxifen Study, which was designed to evaluate the efficacy of oral tamoxifen citrate 20 mg d
Animals exposed to high concentrations of CS 2 225 ppm for 6 h for 14 weeks had increased blood pressure and decreased cardiac output Morvai et al buy cialis usa Sherman, USA 2022 06 19 18 12 49
And natural remedies for low diastolic blood pressure the reason why Dan hypertension nursing education Beast said these words can also be seen that it is about to get angry tadalafil cialis from india
isotretinoin 40mg canada
USES This medication is used to treat and prevent malaria generic propecia for sale
propecia online australia 8 has an absorption of 16
viagra effects on women 2004; Tamura et al
viagra connect reviews 2011; 28 591 6
Efficient dialysis can reduce the speed at which beta 2 microglobulin accumulates, and thus is probably the main reason for the decrease in the incidence of dialysis related amyloidosis with respect to the past, although it has not completely disappeared, in particular in patients who were never grafted 7, 8, 9 viagra cause priapism
cheap accutane
The most accurate way to know that the bacteria are real is by passing a sterile needle attached to a sterile syringe directly into the bladder and withdrawing a urine sample cialis online generic
I m finally 5 1 2 years out topical propecia As well as being recruited by the Ccm3 cells, the Ccm3 cells were stimulated to undergo EndMT
buy isotretinoin 40mg online
clomiphene citrate for women Distraction mechanisms to cope with pain include
She had bilateral rales and was coughing up small amounts of pink sputum levitra contra reembolso
It further prohibits basing rules for eligibility or costs for coverage on genetic information propecia on sale This can be done using a foam wedge
If you have multiple tumors in one breast or have a large cancer, you may not be a candidate for this procedure side effects of propecia depending on the primer length and specificity
In the neonatal literature, four cases are reported with Intralipid 20, a pure soybean oil emulsion 12, 36, 37, 38 brand levitra canada
accutane order online
However, this costly course of action only addresses the secondary problem non prescription cialis online pharmacy The Arimidex, Tamoxifen Alone or in Combination ATAC trial, the largest multinational randomized trial of adjuvant therapy for patients with operable breast carcinoma to date, offers the opportunity to investigate whether nationality is one such factor
buy cialis uk fluconazole azelaic acid prescription australia Yankees president Randy Levine called it Гў sadГў that Valentine would make those comments on the anniversary
A novel coronavirus from patients with pneumonia in China, 2019 male viagra
buy accutane 40mg generic
Breast implants get recalled sometimes zithromax coupon The concurrent use of oral calcium channel blockers and beta adrenoceptor antagonists in the management of angina pectoris or hypertension is less likely to result in heart block or other serious adverse effects 447, and these two drug groups are commonly used together
Does cranberry sauce help lower blood sugar where to buy cialis online forum Popa University of Medicine, Iasi, Romania
propeciahelp This may take as short as 1 2 years in a large VSD, AVSD, or PDA, or as long as a few decades as in ASD
your face, tongue, eyes or anywhere else start swelling; you have trouble breathing or cough or wheeze; you feel dizzy or light headed, collapse or pass out, have a fast heartbeat, clammy skin, or feel confused and anxious these could be symptoms of a serious allergic reaction called best price for generic cialis The show is a bit Oprah esque, and that comparison carries over to her personal life, where sheГў s got a big house and all the trappings of having made it
Information on tumour size, nodal involvement, ER status and tamoxifen therapy of 226 patients is presented in Table 1 where can i buy cialis on line clopidogrel, ibuprofen
cialis online generic Monitor Closely 3 cenobamate, carbamazepine
priligy pill 31 dark, MAP, 0
isotretinoin drug
best price cialis The defeat this time was too big a blow for me, and the humiliation was too deep
1 Although it is not present in all patients, the earliest and most easily recognized manifestation of B levitra francais One could speculate that escape from antitumor therapy is more effective for CTCs when losing ER and PR on the surface
For both the moderate quality QoL outcomes there was no clinical effect of MRAs online indian propecia Mechanistically, the translation of mitochondrial fission process 1 MTFP1 is suppressed by mTOR inhibitors, which eventually results in mitochondrial hyperfusion, a process that antagonizes apoptosis 186
The current standard of care for prostate cancer includes hormone therapy, radiation therapy, and radical prostatectomy, each with its own set of undesirable side effects cout levitra en pharmacie
order accutane 10 mg pill
free dating website
free dating apps no fees
yahoo dating personals
So here we are dealing with an innovative and today extremely demanding telemedicine device best price cialis 20mg I took Clomid day 3- 7 my first two rounds and there were many smaller follicles
buy cialis online usa Mitch iwRrNKbEwnAVoUqKtb 6 16 2022
And that s even more the case when you re pregnant or trying to conceive levitra 20 mg generico
gay dating game fuck
best free gay dating sites
adam4adamn gay dating
Nonsurgical Treatment cialis tablets for sale
famotidine news medical Comparing what the NFL was like before 1933 to what came afterward is like viewing the United States during the era of the ineffectual Articles of Confederation instead of the thriving nation that took shape after the ratification of the U propecia finapil coumadin levofloxacin cena What is more important is the 300 million Americans who are having their phone records violated and are potentially being tracked with their movements through GPS, Paul says as he took his phone from his pocket and waved it into the air
pdf ultramax rx extreme reviews This image provided by the Las Vegas Metropolitan Police Department shows O buy cialis online no prescription
Lux MP, Fasching PA, Beckmann MW can viagra cause heart attacks The term apparent as opposed to true resistant hypertension has been used by investigators to refer to patients with resistant hypertension based on the number of prescribed medications, without accounting for common causes of pseudoresistance, ie, inaccurate blood pressure measurements, nonadherence, undertreatment, or white coat effects
cheap priligy Ibrutinib enhances chimeric antigen receptor T cell engraftment and efficacy in leukemia
is there a generic cialis available Akhtar et al treated 100 frail, elderly women with tamoxifen alone and achieved a 40 clinical complete response rate, a 28 partial response rate, and a 22 rate of disease stabilization, with duration of response lasting several years in some
buy accutane 40mg without prescription
can i buy cialis without a prescription Deregulation of its negative regulatory system may play a role in breast cancer
During the crossover phase, the FACT B score increased in the wait list group and was stable in the treatment group buy online cialis
cheapest cialis generic online There was also a non significant a longer time until the first exacerbation for the treatment group P
Weakness On rare occasions the wait could be more than 15 minutes chicago viagra triangle
generic cialis online europe Despite the absence of specific experimental and clinical evidence of diuretics effectiveness 69, 70, some studies support diuretic use, with this helping approximately two thirds of patients achieve substantial control of vertigo attacks when used in association with dietary low salt diet and increase of water intake and lifestyle modifications 71, 72
accutane 10 mg sale
cialis viagra combo pack I went for a blood test today and
sertraline and promethazine both decrease QTc interval brand name cialis online
Short- acting steroids can also be given in an emergency situation to decrease the inflammation propecia uk Variant human breast tumor estrogen receptor with constitutive transcriptional activity
Educating women concerning the possible complications involved with hysterectomy may ease patients preoperative anxiety and ultimately improve outcomes buy liquid cialis online
Andy Beshear, a Democrat, was elected governor of Kentucky in November, defeating the incumbent, Matt Bevin, in a race that focused in part on Mr home made viagra IVP is an excellent modality to diagnose medullary sponge kidney and papillary necrosis
accutane 40mg tablet
which is another popular bulking steroid; this oral steroid is even better than Dianabol and Anadrol, as it helps you gain 30 to 40 pounds of mass in just a few weeks buy viagra cialis online In contrast, it is possible to detoxify women dependent on heroin who are abusing illicit opioids by using a methadone taper
cheapest cialis generic online Also, a set of genes that is up regulated specifically by TOT but not by E2, Ral, or ICI is shown in cluster C
Barium swallow and follow through revealed thickened mucosa and floculation of the barium, a nonspecific radiological finding of malabsorption syndromes propecia hair
Sastre RL, et al viagra priligy Kristofer BQwXeOUisLB 6 16 2022
Here, we show that proestrus staged SHRs treated with DOX have an increase in cTnI levels and a significant decline in cardiac output as compared to estrus and diestrus staged animals that received DOX buy cialis pills
This is when the red blood cells that carry oxygen through your body break down does viagra lower heart rate
accutane 40mg pill
priligy canada QTc prolongation was common 63
buy cialis daily online An update on systemic sclerosis associated pulmonary arterial hypertension a review of the current literature
cheap cialis Premarketing experience included eight reports of acute risperidone overdosage with estimated doses ranging from 20 mg to 300 mg and no fatalities
cialis viagra combo pack Upon further tissue specific processing, acth can yield alpha msh and corticotropin like intermediate lobe peptide clip
order accutane 40mg online cheap
In addition, on her 2nd, 3rd, and 4th fingernails bilaterally, clinicians noticed a single transverse white line, parallel to the lunula buy cialis non prescription
propecia and rogaine The characteristics of these 4 patients are shown inTable 3 and Figure 3
cytoxan cytoxan iv infusion rate Even if the government reopens in coming days, time is running out for logging projects in high elevation forests where coming snowfall will hamper operations already restricted by contractual deadlines, environmental safeguards and competing uses of forest lands real cialis online
Federico MGhIXUcPPzaLQWls 5 20 2022 buying cialis online forum 21 25 All patients underwent breast conserving lumpectomy 45 or modified mastectomy 55 from 1979 through 1996
buy isotretinoin 10 mg pill
Intriguingly, LRRK2 GS stabilized PIAS1 by increasing the level of small heterodimer partner SHP, a negative regulator of PIAS1 degradation, thereby promoting XBP1 SUMOylation cialis generic 5mg Although a history of trauma might be elicited, other less obvious events including sudden contraction of the rectus muscles with coughing, sneezing, or any vigorous physical activity may also cause this condition
buy cialis online canadian pharmacy clopidogrel rabeprazole domperidone tablets side effects The international mediation effort is helping to contain the bloody conflict between Mursi s Islamist backers and the interim government installed by the military that overthrew him on July 3, following mass protests against his rule
NOLVADEX_ tamoxifen citrate Tablets, a nonsteroidal antiestrogen, are for oral administration cialis buy online
There are no adequate and well controlled studies in humans on effect of drug on female or male reproductive potential; oral administration of to male and female rats resulted in adverse effects on fertility cialis online pharmacy
Palestinian Esmat Mansour was a teenager on an Arab chicken farm in the hills north of Jerusalem in 1993 when Israeli neighbor Haim Mizrahi drove up to buy eggs, as he had done from time to time cialis buy online usa
I’m really loving the theme/design of your website.
Do you ever run into any web browser compatibility issues?
A number of my blog audience have complained
about my blog not operating correctly in Explorer but looks great
in Chrome. Do you have any suggestions to help
fix this issue?
buy accutane 40mg online cheap
Monitor Closely 1 erythromycin base increases levels of rifaximin by P glycoprotein MDR1 efflux transporter levitra basf
Most investigational drugs fail endpoints before reaching the clinic, but Dr best viagra for men
buy isotretinoin 10 mg sale
64 66 With paclitaxel at 175 mg m 2 and gemcitabine 1200 mg m 2 on a days 1 and 8, Genot et al reported outcomes for 40 patients buy cialis online no prescription When are going to take a hpt
Moore BD, Khurana SS, Huh WJ, Mills JC mom relieves viagra accident
cialis super active she was fine letting TuesdayГў
prix levitra 10 mg Mutations in context implications of BRCA testing in diverse populations
priligy over the counter usa Mizoguchi M
san antoino gay dating
[url=”https://gay-singles-dating.com”]gay dating sites black dating white[/url]
gay dating sites that work
These effective and accurately composed injections are extensively popular for their enhanced shelf life canadian pharmacy cialis
A blockage in the reproductive tract of the man or woman may prevent fertilization how much are viagra pills 290 An orally dosed drug was the goal to give maximum flexibility of dosing for use as a single agent and in combination with DNA damaging agents
Among the 225 total patients enrolled in APOLLO, 126 56 fulfilled criteria to be included in the prespecified cardiac subpopulation is propecia safe Instituto de Agroquimica y Tecnologia de Alimentos, Spain
During the first few days after birth, the red cells have a normal or high content of GSH can i buy priligy over the counter lobular breast cancer Invasive ductal carcinoma begins in milk ducts whereas invasive lobular carcinoma begins in lobules the milk producing glands of the breast
Ideally, however, sinha, alone 22 t2dm buy vardenafil 40 mg online Monitor Closely 1 escitalopram, aspirin
buy cialis online canadian pharmacy I have a friend who is a nutritionist, but was totally unaware of conditions like candida
I use PrimalMale, 6 oxo, Sam e, and R ALA viagra pill image
isotretinoin order
Among the classification criteria for stratifying anovulatory women, normogonadotropic normoestrogenic patients, also known as World Health Organization WHO group II, account for around 80 of all anovulatory patients 1 lasix hypokalemia
tadalafil cialis from india The authors extrapolate that CYP2D6 inhibiting SSRIs do not block the conversion of tamoxifen completely and might still leave enough active metabolite to adequately block estrogen receptors
After a single dose in healthy volunteers, the plasma half life of piperacillin and tazobactam was in the range of 0 cialis online ordering
0 but confidence intervals were wide Verloop et al cialis order online During pregnancy, this medication should be used only when clearly needed and not for prolonged periods
The findings from this study may influence the design of future patient facing decision aids around pain management cheap propecia 10mg 2004; 187 S38 S43
Maybe they should lighten up one certain drugs and just fine them, unless the drug is for enhancement disadvantages levitra mejor que viagra Dosage form injection, solution
best free date sites
totally free dating sites near nelson
dating meet singles
Jamar SjxgqrredeqhYgPDyIx 6 17 2022 reddit priligy
Chemotherapy also reduces recurrence but is more toxic and requires more careful medical supervision to ensure safety and efficacy buy cialis generic online cheap
A transthoracic echocardiogram TTE revealed global left ventricular LV dysfunction with an ejection fraction EF of 15 levitra vs cialis
buy accutane 10 mg without prescription
buy cialis During your virtual visit, our doctors will hear your symptoms and refer you to your closest lab
For example, AstraZeneca sold the rights to its shelved schizophrenia drug candidate to Millendo therapeutics is there a generic cialis available
I m on CD7 and my temps have been 96 levitra 10 orodispersible bayer NDC Code s 71288 555 85, 71288 555 86 Packager Meitheal Pharmaceuticals Inc
It is always important to know what kind of reagents you work with in experiments viagra vs cialis vs levitra
order accutane without prescription
Huland E, et al buy cialis generic buspar differin dr dray His latest interview builds upon this new direction
buying cialis online forum Femara letrozole warnings
[url=https://accutaneon.com/]isotretinoin 10 mg over the counter[/url]
Carcasses will be placed in a DIP bin in the cooler; bins are labeled with the day of the week that corresponds to the date on the automated email that PIs and staff receive once the DIP slip is processed tadalafil generic vs cialis Surgical sperm preparation An alternative tries and from the perineum and by matic categories, as above additional Single cause epididymopathyd, environmental, life style genetic abnormalities in testicular volume from talairach z coordinate 30 mm above the rior vaginal wall, a reduction in diet or laxative medication, and relation ship and management of erectile dysfunction
Accepted 06 January 2022 tadalafil cialis
viagra what is it Breast cancer treatment and sexuality
is cialis generic frumil ivermectina para tvt Sharing quality time doing things you enjoy with your children preferably activities that don t involve spending a lot money will help them grow up happy and well adjusted much more than footing the bill for them to be one of the cool kids
order accutane 40mg sale
These cells also have the sodium driven bicarbonate chloride exchanger NDBCE; a product of the Solute Carrier Family 4 Member A8 or SLC4A8 gene in the luminal membrane see discussion below cialis coupons viprogra olanzapine serotonin receptors ItГў
H de Lavallade, P Finetti, N Carbuccia, etal A gene expression signature of primary resistance to imatinib in chronic myeloid leukemia Leuk Res 34 254 257, 2010 Crossref, Medline, Google Scholar 11 viagra effect time They have young children, so it will affect themmore than me, he said
Complications of Pregnancy Insomnia Does Pregnancy Insomnia Hurt My Baby is there a generic cialis available
where to buy cialis Yassouridis, A
online casino free bonus
casino online usa
online casino bonus no deposit
Funk JA, Lejeune JT, Wittum TE, Rajala Schultz PJ The effect of subtherapeutic chlortetracycline on antimicrobial resistance in the fecal flora of swine brand name cialis online 2013; 14 3 136 141
cialis buy online Can be used to reduce the amount of androgen in the body
Herbal supplements are very popular among cancer patients as a way to ease symptoms and as an alternative treatment Treatments in general where to buy cialis online
buy cialis online from india Ask the average man to identify some of the most important hormones in his system, and the first one likely to be mentioned is testosterone
Obama an opportunity to back down from military strikes, but also to help Assad to butcher his people, said Prince Turki buy finasteride 5mg with amex The NPV of the risk model at each cutoff point was between 93 and 99
dating best site
casual dating
ourtime dating site log in
buy cialis online no prescription The Normal Blood Sugar Levels Chart child with 178 blood sugar reading Diabetes Prevention Program and two other large prospective studies in Finnish and Chinese child with 178 blood sugar reading populations show that lifestyle interventions successfully prevent conversion to diabetes by 58 at child with 178 blood sugar reading
levitra prices 20 gm free delivery Sulfonamides in urine have been analyzed by coupling an SPE apparatus to the CE instrument via a switching valve
levitra produit MRI of the brain Fig
Not all prescription drugs are included on the drug list hims vs viagra Indeed, we found that Cxcl17 induction and macrophage accumulation marked bronchiolar alveolar remodeling regions in PVLD
If you re experiencing severe pain, go to the nearest emergency room and contact your healthcare provider immediately buy cialis
dapoxetina comprar online Moderate Vitamin A Intake During Pregnancy No Increased Risk of Birth Defects, 172, p
isotretinoin oral
What Is Feline Infectious Peritonitis FIP in Cats viagra overdose
Photos of koi with bacterial infections what is viagra made of AK093306 Homo sapiens cDNA FLJ35987 fis, clone TESTI2014269, highly similar to D 3 phosphoglycerate dehydrogenase EC 1
Where we disagree is the application of CRT within this indicated population what’s better than viagra
levitra 10mg belgique Raloxifene 60mg per ml x 30ml
cost isotretinoin
how to buy cialis Some patients with previously unrecognized chronic liver disease decompensate and present with liver failure; although this is not technically FHF, discriminating such at the time of presentation may not be possible
buy cialis online cheap grapefruit will increase the level or effect of lopinavir by affecting hepatic intestinal enzyme CYP3A4 metabolism
[url=https://accutaneon.com/]buy isotretinoin 10 mg online[/url]
buy cialis Paclitaxel sollen anstelle der CYP3A4 Induktoren alternative, nicht enzyminduzierende Arzneimittel eingesetzt werden
You may want to go back to my role in the House where year after year after year, guess which member of Congress got more amendments passed on the floor of the House than any other in a bipartisan way generic levitra for sale in us God of the Origin Universe, your opponent is me
By substitution into the linear regression equation for the changes in arterial pressure versus plasma nitrate, an increase in plasma nitrate into the millimolar range would be necessary to increase arterial pressure to any significant degree tadalista vs cialis
Among partial responders 55 y buy liquid cialis online Travis dkyTTGYiAqTb 6 21 2022
Monitor Closely 53 buy cialis online prescription Less data is available regarding the use of AIs
order accutane 40mg generic
In many African medical facilities, there may be only one pathologist and an enormous number of clinicians who rely on this pathologist to analyze their biopsies generic cialis online pharmacy 28 If initial surgery is incomplete, re excision should be performed to achieve a wide margin of resection
Marwick, Charles does propecia work
Over time, insomnia can make it hard to function at home and concentrate on tasks priligy 30 mg
Öýýðëýëò ГГЅГЅГ± õà à ãäà õ, ГїГГ§ ГЎ ðèéà øà ëòãà à ГГ Г Г° ГЎГЁГҐГ¤ ГёГЁГãýà õóðèìòëà ãäà õ, ïëà çìûà îñìîñò Г ГГ Г° èõñýõ, Г§ ðõГГЁГ© äóòà ãäà ë, áýëäìýëä õýò ìýäðýã Гµ Г¬ Г± çýðýãò ГІГіГ± ГІГіГ± õýðýãëýõèéã öýýðëýГГЅ achat levitra en pharmacie
buying priligy online In this study, the authors related this poor prognosis to a propensity of AM to develop distant and brain metastases 39
isotretinoin 40mg cheap
77, but the evidence for an interaction between TAM treatment and level of TIL infiltration on BCFi was weak P interaction 0 cialis online prescription
levitra deezer Patients receive oral placebo twice daily once daily in weeks 1 4
free welcome bonus no deposit
online casino free bonus no deposit
free welcome bonus no deposit casino
Patients treated with diflunisal, on the first dose, tend to have a slower onset of pain relief when compared with drugs achieving comparable peak effects buy zithromax no script
Feeding a soy based formula to infants who have lactose intolerance might help to reduce symptoms cialis pills
Brand Hycamtin Packaging Type strips Usage Application Ovarian cancer Composition Topotecan 1mg Drug Name Topotecan 1mg Dose Strength 1mg Minimum Order Quantity 10 Strip buy priligy 30 mg x 10 pill This targeting potential was attributed to HA CD44 interaction resulting in RME
Classification of the Gastropoda levitra 20mg 10mg 2016; Matsuda and Oinuma, 2019
levitra gratuits The ramipril generic name previous god, hypertension treatment goals Amaro, looked like a demon does eating spinach lower blood pressure who wasn t very powerful, Of course, Physician knows that any demons that need to be sealed are not fuel efficient lamps
accutane 40mg sale
buying cialis online safe My lower back and ovaries are constantly cramping
if a girl took viagra what would happen CrossrefMedlineGoogle Scholar 65
cialis generic name Chung L, Valenzuela A, Fiorentino D, Stevens K, Li S, Harris J, et al
There are simply no others on the market which can compare levitra para diabeticos Such coupling between Na K ATPase and basolateral potassium channels has been demonstrated in proximal tubule cells 167 but, as indicated in Fig
order accutane online cheap
cialis without a doctor’s prescription Chronic heart failure is a condition characterized by vasoconstriction, volume overload, and neurohormonal activation
They listened to my concerns, helped me keep track of all my medications, were compassionate towards my needs cialis from india
priligy for sale Extensive accumulation of diazepam and its major metabolite, desmethyldiazepam, has been noted following chronic administration of diazepam in healthy elderly male subjects
lower price on finasteride camber PMID 19074846
isotretinoin generic
Legro, a professor of public health services and chair of obstetrics and gynecology at Penn State University priligy results Getting to and from the hospital or clinic can be hard, especially if you live far away or if others rely on you for care
Use any pellet applesauce mixture immediately and do not store for future use Priligy
buy liquid cialis online The first surgery would involve dividing and re routing the inferior epigastric vessels to perfuse the subcutaneous tissue in the infraumbilical area
isotretinoin tablet
A few days ago, Rogge s trail suddenly disappeared completely, and a few days later he appeared in another direction, hundreds of kilometers away, does lavender lower blood pressure as if flying how to buy priligy im 16 years old
left beating nystagmus when looking left, but changes to right beating nystagmus when looking right buy propecia 5mg 5 glutaraldehyde in PBS
discount finasteride The Major players covered in the Tamoxifen market report are
online free
dateing sites
mature dating
Caspase 3 activity was quantified by determining the degradation of the fluorometric substrate DEVD Biomol Research Labs, and protein concentration was measured using a Bio Rad detergent compatible kit Bio Rad DC Protein Assay Kit, as described previously 44 buy propecia 5mg usa
Publication bias and stability of effect estimate levitra pas cher generique 2005, 94 115 122
levitra filagra gel shots 100mg J buy cialis daily online Kobayakawa, K
generic accutane 40mg
Cardwell C, R viagra with food
Women also report more stress than men in confronting infertility Greil, 1997, seek more social support, and engage in more positive re- appraisal and escape avoidance Jordan and Revenson, 1999, while men may engage in more distancing Peterson et al nitric oxide and viagra
purchase isotretinoin pill
Some microRNAs promote HCC through inhibiting ER О± cialis cost It has been suggested in the literature that patients who have IVF have their care experience improved by minimizing the burden associated with the process
buy priligy pakistan Hamilton, Keyvan Karimi Galougahi, Yeon Jae Kim, David W
order generic accutane 40mg
This decrease in bile acid reabsorption reduces the size of the bile acid pool, which stimulates the conversion of cholesterol into bile acids in the liver 139 purchase cialis online Cervical mucus is a fluid produced by the glands around the cervix and plays an important role in reproduction
Suppression of mouse mammary tumorigenesis by longterm tamoxifen therapy propecia sell
how long does it take for viagra to take effect Heavenly cbd oil for skin tightening Demon Technique Ye Fan took a cbd dosage for brain tumor deep breath and released the Heavenly Demon Technique
And yet they died nobly buying generic propecia online
best casino site
online casino free bonus
no deposit bonus online casino
Is the thirst feeling normal or dysregulated in BC predisposed and diseased individuals cheap cialis generic online Jerrell, USA 2022 06 19 19 53 00
Conventionally, ISCL fields are matched on to tangential breast fields using various techniques 29, the difficulties in matching treatment fields to achieve homogenous dose distribution may results in overdose to BP buy cialis generic
Myth 6 is the politically correct myth, Dr cialis for sale in usa
and Cummings, M generic viagra online
buy accutane 40mg sale
In the glomerulus, water is initially filtered out, along with the other solutes e best cialis online The first workshop was dedicated to What is IC
Other researchers stepped up after Newhouse published his findings in 2008 marijuana and viagra 27 For selected samples, including those with dual mutations, mutations were confirmed by direct sequencing Data Supplement
The old belief is if you can get away with 200 mg of testosterone for 400 mg of Deca Durabolin you re lucky, some need to use double the testosterone of the Deca Durabolin amount, so for 400 mg Deca Durabolin you would need 800 mg testosterone what is propecia Their effect on toxin production is unknown
accutane uk
The incidence of volume depletion was somewhat higher and the incidence of hyperkalemia somewhat lower in empagliflozin treated patients with recent volume overload Supplemental Table 1, but the between group differences in the number of events were small priligy 60 mg I was successful in the fact that I finally ovulated
Who is more prone to hot flushes propecia online no prescription It can occur by itself or can be the result of surrounding parenchymal disease like infection, malignancy or inflammatory conditions
buy cialis 20mg I say fuck it and go all the way
Fatty acids in evening primrose oil help with acne, reducing inflammation of the skin and helps it retain moisture cialis online india vehicle treated cells set equal to 1 and represent the mean SD in three independent experiments
buy accutane 10 mg online
cialis tadalafil Eduardo znjmDkiDhfVmkcmZYp 6 18 2022
Adequate carbs to fill out also needs hydration in the muscle or you ll just be flat what company makes viagra Chemically, telithromycin is designated as Erythromycin, 3 de 2, 6 dideoxy 3 C methyl 3 O methyl О± L ribo hexopyranosyl oxy 11, 12 dideoxy 6 O methyl 3 oxo 12, 11 oxycarbonyl 4 4 3 pyridinyl 1H imidazol 1 yl butyl imino
It works slightly differently by suppressing estrogen production in fat tissue, which dramatically lowers estrogen levels levitra allemagne
As defined by ONS, the area extends as far east as Haydock and St can i buy viagra at cvs I imagine that first evening that we are alone in hospital and being able to hold you and tell you how loved you are
isotretinoin for sale
According to self defense experts, here are 3 steps to install as your instant reaction buy cialis professional
2009 Jul; 23 5 709 15 cialis online reviews
Relationship between dietary vitamin C intake and pulmonary function in the First National Health and Nutrition Examination Survey NHANES I priligy reddit
cialis generic cost Natural history of the infant gut microbiome and impact of antibiotic treatment on bacterial strain diversity and stability
and Akerstedt, T how fast does viagra work
teen chat rooms 13-16 gay
gay widow chat site
free gay video chat rooms
Soaps and detergents are used to help remove bacteria because of their ability to lower the surface tension of water and act as emulsifying agents cialis no prescription After around 2 hours, remove to see if the bleeding has stopped
He also trained the undefeated three year old champion male Norfolk and undefeated Asteroid buy cialis
As far as pharmaceutical drugs are increasingly seen as substituting for care as relational practice, modern healthcare science has come to consider pharmaceuticals as synonymous with caregiving Biehl 2012 another name for viagra For example, the case fatality rate for breast cancer is 23
cialis on sale in usa I can t bear to put down another dog
online datings
totally free dating sites no fees ever
sex dating free
And the people will insist on turning out in all squares, senior Muslim Brotherhood official Farid Ismail said coupons for cialis 20 mg His blood pressure is already tenuous
19 Lin, SJ, Lee, WJ, Liang, YW, Yan, DC, Cheng, PJ, Kuo, ML tadalafil cialis zaditor cipralex costo gocce SEC spokesman John Nester said the agency has implementednumerous changes since the report was completed, from installingadditional physical security barriers to putting the SEC ssecurity staff in charge of criminal background checks insteadof human resources
can women take propecia They get everything done and still make us patients feel good and happy
Originally, he was worried that he would miss the task given natureganics horny goat weed dietary supplement by the master tadalafil cialis from india
cialis prices However, before you try to buy this drug over the counter, there are a few things to consider
buy generic cialis online cheap Vitamin E is sold as a dietary supplement, either by itself or incorporated into a multivitamin product
but hey that s your decision not mine medicamento priligy estudios clinicos 119 g mol CAS ID 50 65 7 Formula C 13 H 8 Cl 2 N 2 O 4 Melting point 225 to 230 C 437 to 446 F
cialis online no prescription In Taylor A, Nally JV, Thomsen H, eds
levitra e bom 2022 07 06, Can Pain Meds Lower Blood Pressure
retin a dutasteride price BP shares have lost a third of their value since thedisaster, as the company hived off 39 billion of assets thatgenerated 5 billion a year in cashflow or about a fifth ofits earning power before 2010 buy cialis online without prescription
cialis coupons Please let me know if you have any suggestions or tips for brand new aspiring bloggers
The defendant shipped the fakes on to purchasers, some of them repeat customers buy cheap cialis discount online As with other pills, your partner will also need to monitor what you and your doctor are doing during the time you take Cialis
Randy ifUaqYhcRJQRT 6 19 2022 cialis coupons
discreet cialis meds lovelyrose 7 years ago Wedding April 2012
B Co IP of endogenous WHSC1 and BRD proteins from HeLa nuclear extract cialis prescription Non invasive cancers were also less in patients on tamoxifen 31 versus 59 cases 2
priligy cost PMID 20951035
free boys gay chat
gay chat apps
gay web chat
buying cialis online usa Packing on lean muscle while loosing fat
buy cialis online 20mg We thank Corrie Nieuwenhout for skillful assistance at the outpatient clinic
This appears worse in breast tumors with higher levels of LDL receptors viagra after prostate removal
Laboratory Abnormalities Creatinine increase, Elevated liver enzymes, Hemoglobin decrease, Proteinuria cheap cialis online canadian pharmacy
gay sex massachusetts chat
gay chat room
free gay cam to cam chat
You can start ovasitol at anytime buy cheap generic cialis uk
She had me come in for a Femvu, which is when her suspicions were confirmed about me having polyps is viagra gov funded
Arnoldo CPAShsgDRtFs 5 19 2022 finasteride prescription floroda Cabergoline also contributes to an increase in strength and stamina, making it a fantastic option for people who want to push themselves to the maximum
Abortion is the only common surgical procedure that is elective in obstetric and gynecologic residencies real cialis no generic It is seen exclusively in untrained athletes
gay chat with married men
gay chat free no cost
free gay and bi mens chat
drospirenone misoprostol cebu Mike Trevino, a spokesman for American, said in a statementthat the ruling shows that American is heading in the rightdirection and that the company will show that our plannedmerger with US Airways is good for consumers cialis from india
The PRS is a strong risk factor for ER positive breast cancer in moderate to high risk individuals treated with either tamoxifen or raloxifene for cancer prevention buy finasteride 5mg with amex These results account for the previous observation that vasopressin increases the apical potassium conductance
S9 and Table 3 buy generic cialis online cheap
priligy and cialis Nitrates Nitroglycerin
generic cialis vs cialis Module analysis was performed by MCODE, an application in Cytoscape software
Studies continue looking at these medications prix du levitra 10 maison de la gendarmerie Tamoxifen has level 2 evidence for treating acute mania, but with safety concerns and little clinical experience 63; therefore, contrarily to lithium, it cannot be advised as first line treatment
Hopefully the outcome will be positive cialis prescription Women under 50 who consumed three or more cups of tea per day had a 37 lower risk of breast cancer than women under 50 reporting no tea consumption in one study
Our hospital is in a suburban area and a large portion of people are workers or farmers engaged in field activities, increasing the chance of contracting rickettsioses cialis pills
We assessed Plk1 expression in five chemoresistant cancer cell types and found that Plk1 and its downstream phosphatase Cdc25c were selectively overexpressed in tamoxifen resistant MCF 7 TAMR MCF 7 breast cancer cells buy generic propecia uk From what I understand and the reason my Dr
The same formulations exposed a similar behavior regarding the DE 60 of DPX can you buy priligy in usa Our team is here to help you make informed decisions about which treatments are right for you
non prescription cialis online pharmacy We will address these specific alms by conducting a double- blind, randomized trial of ovulation induction with CC plus DEX compared to CC plus placebo
levitra famciclovir for cats cost Fundamentally there are a lot of things that need to befixed, said Laura Chen at BNP Paribas, adding that HTC neededto work on marketing, supply chain management and streaming itsproduct line buy generic cialis 1986 25 103 108, Utsumi et al
Pharmakologisches Institut, Universität Heidelberg, Heidelberg A best site to buy cialis online I have pretty regular cycles, and keep track of everything normally but this time to AVOID pregnancy
cost venlafaxine 75 mg venlafaxine 75 mg pills buy venlafaxine sale
Many older adults lie in bed between 9 PM and 8 AM but only require about 6 7 hours of actual sleep soft tab cialis
Overall, the LCa lobe consistently exhibited different behavior pre to post PNX compared to the other remaining lobes buy cialis cheap Seiwell, and D
priligy dapoxetine 30mg In order to realize the synthesis, the necessary 4, 7 dichloroquinoline 37
where to buy cialis Immunolocalization of renin in CNT
effexor 75 mg price purchase effexor generic effexor 150mg for sale
Kaplan EL, Rich H, Gersony W, Manning J brand name cialis online Studies showed that chidamide treatment with low dose doxorubicin exhibited a synergism effect on cell growth and apoptosis in two PTCL cell lines 43
discount cialis Molecular Heterogeneity and Response to Neoadjuvant Human Epidermal Growth Factor Receptor 2 Targeting in CALGB 40601, a Randomized Phase III Trial of Paclitaxel Plus Trastuzumab With or Without Lapatinib
prix levitra pharmacie belgique For secondary outcomes such as hormone levels, a linear mixed- effect model will be fit where the main independent variables will be treatment group, time, and their interaction as well as the designed randomization stratification factors as covariates
But with online pharmacies, you can typically request a refill online and have it shipped to you viagra cialis online
omeprazole will increase the level or effect of warfarin by Other see comment can i buy cialis without a prescription Ten days before the second round, a survey conducted by the sociological group Rating showed that as much as 51 percent of Ukrainians intend to support Zelensky
Newquist, in Small Animal Pediatrics, 2011 cialis generic best price Monitor your hearing and balance regularly if you suspect that you are dealing with ototoxicity
prix du levitra medicament PMC free article PMC4527019 PubMed 26195505
Cnr1 fl fl mice C57BL 6N background harboring the conditional floxed Cnr1 alleles were generated using CRISPR Cas9 at the Transgenic Core Facility of the University of Texas Southwestern Medical Center cialis with dapoxetine Doses of labetalol HCl that controlled hypertension did not affect renal function in mildly to severely hypertensive patients with normal renal function
cheap cialis online canadian pharmacy SLNs are prepared from various methods, as discussed further Mukherjee et al
buying cialis online Tamoxifeno Gador is used to treat some types of breast cancer in men and women
cheapest cialis 20mg This causes the muscles of the corpora cavernosa — a pair of sponge-like areas of erectile tissue — to relax, allowing blood to freely flow into your penis and expand the tissue
Food Quality Protection Act, 159 p25 27 cialis generic 5mg Okada A, Sato T, Ohta Y, et al
In Pregnancy Testing, Our New Icon 25 Hcg Test Will Reshape Your Thinking best cialis online
Positron emission tomography PET images of tumor bearing rats demonstrated that tumors can be visualized 1 h after rats are injected with an 18F fluoro analogue of tamoxifen propecia cost and a peak at 338 C
We reported that HER2 overexpression in a xenograft model results in tamoxifen stimulated growth as a mechanism of de novo resistance 9 12 topical propecia
hidden gay video chat
video chat older gay
gay boy teen boys webcam chat rooms
discount cialis Start using them about three days before you expect to ovulate and follow the directions on the package to use and read them
cialis 20 mg E The number of PLCОІ2 above and NCAM below positive cells per taste bud in CTL and KO cells is shown
kanada levitra bestellen com or Privatemdlabs
buy pregabalin 75 mg sale lyrica 75 mg pill pregabalin 75 mg tablet
An important concept is that postmenopausal women not only produce estrogens through peripheral tissues through the activity of the specific enzyme called aromatase, but also that aromatase is present in high concentrations in many breast cancers buy cialis online without prescription
In order to overcome these drawbacks we have used a transcriptionally inactive mutant of the murine oestrogen receptor which is unable to bind oestrogen yet retains normal affinity for the synthetic ligand, 4 hydroxytamoxifen buy cialis 5mg daily use Packer M, O Connor C, McMurray JJ, Wittes J, Abraham WT, Anker SD, et al
gay chat no registration
321 gay teen chat
transcript of a man’s first gay chat
want to buy priligy in pakistan Martins Lopes Moises S, Machado Larissa M, Amaral Silva Pedro A Ismael, Tome Uchiyama Angel A, Yen Cheng T, Ricardo Eliza D, Mutao Taciana S, Pimento Jefferson R, Pimenta Jefferson R, Shimba Denis S, Hanriot Rodrigo M, Peixoto Renata D 2020 Antibiotics, cancer risk and oncologic treatment efficacy a practical review of the literature ecancer 14 1106
cialis 5 mg best price usa CHLO at a dose of 30 g kg of chow significantly increased caspase 7 expression and Bax Bcl 2 ratio in mammary carcinoma cells in rats 13
finasterid What s missing
2005; 15 11 18 viagra dosage
These include invasive as well as in situ carcinomas what is priligy 2009 May; 36 5 1087 8
stromectol otc ivermectin over the counter canada ivermectin 3mg price
what drugs should not be taken with viagra Nitrofurantoin has been associated with some birth defects
Boxers and Powerlifters use it to increase aggression and strength prior to training or competition proscar order best on line pharmacy All guidelines say no, in red, in very big letters
New York Wiley Liss Inc hair loss propecia
Ping Dou, in Drug Repurposing in Cancer Therapy, 2020 what is priligy tablets 1 1 NA 1 1 1 1, NA 1 1 Arbetter et al
ivermectin 200mg stromectol tablets uk ivermectin canada
There have been claims that clary sage oil brightens eyes, improves vision and protects loss of vision due to premature or normal aging; however, there is not enough research to suggest that essential oils be used in the eyes just yet where can i buy cialis on line He concentrated the remaining mental power downwards, and the maid suddenly screamed with excitement, Ofirok let out a long laugh, fully regaining blood pressure medicine makes you bruise the radiance of the golden lion
If you are looking to lose weight after your cycle, there are a few key tips you can follow buy priligy in uae
Another said that the hill giants have the bloodline of the ancient giants cialis online pharmacy You can see that steroids have a number benefits
And as long as it s not elevated, we re probably relatively safe in doing this viagra vs cialis
free gay chat
chat with senior gay’
live gay chat
buy priligy Common side effects noted with OFS include hot flashes, fatigue, bone pain, and vaginal dryness decreased libido
Hypocrisy about steroid usage is harmless but evasiveness, lies and secrets aren t levitra 10mg vidal Trave I, Merlo G, Cozzani E, Parodi A
viagra tadalafil tarif viagra en pharmacie prix viagra
best price for generic cialis Only adverse events more common on Ebefen tamoxifen citrate than placebo are shown
aluminum acetate; and are designed to evaporate over time, thus helping to dry the ear cialis generic name Consistence with cancer cell line data, we also found that triple negative breast cancer tissue had higher level of collagen XIII expression compared with other subtypes Fig
In many cases, the emergency room will give you pain medication to mask the symptoms until you can schedule an appointment at our Eagle River office priligy tablets price More than 460, 000 women are diagnosed with breast cancer BC in Europe each year, and BC is responsible for 130, 000 deaths 1
cialis order online Yocum passed away in his sleep on November 29th, 2017
Why Clenbuterol Cycle is a great choice where to buy priligy I always found that I was much calmer and relaxed after leaving my session
frree gay and bi chat sites in seattle wa
gay online chat sites
gay sex chat online
com 20 E2 AD 90 20Viagra 20Nakup 20 20Viagra 20Generic 20Price viagra nakup Chairman Roberto Quarta said Гў generic cialis for sale
There were no deaths during this period cialis buy ruber; 85 of the degradation was found in consortia containing Achromobacter xylosoxidans followed by 80 in a combination with S
carbamazepine decreases levels of crizotinib by affecting hepatic intestinal enzyme CYP3A4 metabolism cheapest levitra professional
tadalafil cialis Monitor Closely 1 clarithromycin will increase the level or effect of erlotinib by P glycoprotein MDR1 efflux transporter
Remember as you get older your eyes will form cataracts at some point so you will need to plan for that if the need arises is cialis generic
Wang jy, burns, ed garlic natural viagra Monitor Closely 1 brexanolone, diazepam
buy cialis online forum Eligibility for P-EBT for school aged children is dependent on being eligible for Free Reduced price meal benefits through the USDA National School Lunch and School Breakfast Program
cialis 5mg best price Such decrease, possibly due to interference with B 12 absorption from the B 12 intrinsic factor complex, is, however, very rarely associated with anemia and appears to be rapidly reversible with discontinuation of metformin hydrochloride tablets or vitamin B 12 supplementation
order sildenafil generic buy sildenafil generic cenforce pills
If no improvement in scorbutic symptoms is observed after one week of treatment, retreat until resolution of scorbutic symptoms is observed Vardenafil I have an app on my kindle My Days it let me know when AF is coming and O day very good and on point
levitra why so exspensive 2007 degrees from the University of Pennsylvania
I am think about get my lasik operation done in a couple of month comparatif viagra cialis levitra
1 Tamoxifen has an E 2 agonistic effect on histologically normal human endometrium buy generic cialis online
diflunisal and ibuprofen IV both increase serum potassium cialis generic cost
buy cheap generic cialis online Stangl testified further about the reception area
We included studies which examined i the role of bacteria in low back pain and ii the relationship between the presence of bacteria and Modic changes cialis and viagra sales 4 mg kg with no modification for altered renal status
priligy medicine Because women are more sensitive to using SARMS it doesn t take the same dosage a male would need in order to get the same results
Galactose has a high affinity for FSPF us pharmacy viagra
poppers and viagra Ofirok quickly approached the furosemide and 3 what blood pressure medicine is compatible with benazepril blood pressure medication camp of the Ferocious Knights, Suddenly, there was a commotion in the barracks, and the rapid horns kept blowing
i need a loan, i need education loan. i need payday loan today i need loan, need a loan no credit check, cash advance loans direct lenders only, cash advance loans, cash advances, do cash advance loans affect your credit. Financial affairs will spark money management, financial institution . fast loan direct need fast loan fast loan advance.
buy cialis online overnight shipping valtrex levitra online 10mg Гў We are thrilled Amy and Tina have decided to return as hosts of the Golden Globe Awards for the next two years, Гў said HFPA president Theo Kingma
Although, transvaginal US is excellent in determining the endometrial thickens, US is limited in the evaluation of the depth of myometrial invasion by the EC rogaine vs propecia 7 Ever pregnant at first clinic visit 2, 250 60
80 to the dollar on Tuesdaybefore buying by the RBI helped it post a gain finasteride 5mg no prescription cheap A Light Primer Before evaluating the effects of HEV, ODs must first understand what it is and where it comes from
cheap cialis online In this case, several candidates are possible and it is not possible to highlight a precise chemical structure
A 34 YOF reported galactorrhea after using fluvoxamine for about 2 weeks for OCD Chakladar et al cialis from usa pharmacy tolmetin will decrease the level or effect of aliskiren by Other see comment
dirty gay video chat free
i wanna fuck gay chat
gay masturbation chat
striatum is a case of concern buy cialis online no prescription
Furthermore, metastasis of PI3KC2ОІ knocked down xenografts were insensitive to treatment with ceramide liposomes, suggesting the role of ceramide as a metastasis suppressor lipid and an involvement of ceramide interaction with PI3KC2ОІ in metastasis suppression 94 buy cheap generic cialis uk Reference Riyad as Salihin 81 In book reference Introduction, Hadith 81
Acute bacterial prostatitis can be accompanied by severe sepsis or septic shock see Chapter 86 cialis tablets for sale While not recommending breast self exams as part of a routine breast cancer screening schedule, the ACS does advise that, Women should be familiar with how their breasts normally look and feel and should report any changes to a health care provider right away
levitra 10mg lyoc 98 A unique classification for mouse mammary tumors was devised by Dunn
does viagra make you bigger Furthermore, accurate clinical staging in ILC is difficult due to lower sensitivity of imaging tests, which could impact analyses by stage
levitra efectos If you think you may have already passed a Clomid challenge test because you ve taken Clomid before, check with your doctor
ring central gay chat rooms
chat gay en espanol gratis
gay universe man chat
They claim that it is the strongest volume pill on the market cheap cialis online
Each told me I was a candidate for a different procedure at PVI though Dr cialis 5mg 7 287 296; each herein incorporated by reference in their entirety
buy online cialis Monitor Closely 1 chlorpromazine and voriconazole both increase QTc interval
microdosing viagra Importance of medication reconciliation
I believe not 100 sure that she is panting less now she was really panting hard at night and early morning, but last few days she hardly panting at all and it maybe because she feels comfortable now in our home she has been with us just 32 days cialis without prescription Geller S, Dajoux R, Armoghathe JF, Scholler R 1977 Une nouvelle Г©preuve d exploration de la fonction testiculaire l Г©preuve combinГ©e clomiphene- HCG- Dexamethasone
selpercatinib increases toxicity of posaconazole by QTc interval generic cialis
1997; Soules et al cialis buy online usa
gay chat random
freee gay chat
free gay video chat room
After all, his impression of Zhao Ling and generic cialis no prescription
The labeled RBC methods carbon monoxide, radiophosphorus P 32, and radiochromium Cr 51 tagged RBCs have a theoretical advantage in that the tagged cells do not leak from the intravascular space priligy for pe
Arpino G, Bardou VJ, Clark GM, Elledge RM 2004 cialis prices
Bacteriologic cure usually is achieved rapidly, and the duration of therapy is similar to that recommended for other osteoarticular infections or endocarditis buy cialis on line Cancer 118 1192 1201
gay cruising chat
gay video cam chat
gay incest chat
2022 Aug 12; 11 1 166 buying cheap cialis online 900 20 mg Caja x 10 tabs
Ouyang Ying questioned continuously, not afraid of the so called so called The eighth order diabetes blood sugar monitoring creator god comparatif viagra procalis levitra viagra difference between metoprolol tartrate and metoprolol er Caterpillar said it had temporarily shut some plants, furloughed thousands of salaried and managementemployees and reduced its full- time workforce by 3, 000 duringthe third quarter
Anyone who registers to donate eggs or sperm can no longer remain anonymous and has to provide information about their identity. siphene buy no prescription That s just what endo does.
azithromycin over the counter canada Information about VMS was obtained with the Greene Climacteric Scale questionnaire
It is created by eHealthMe based on reports of 40, 831 people who have side effects when taking Xeloda from the FDA, and is updated regularly how long does viagra take to kick in
Neuropathic pain associated with diabetic peripheral neuropathy DPN 1 Postherpetic neuralgia PHN 1 Adjunctive therapy for the treatment of partial onset seizures in patients 17 years of age and older 1 Fibromyalgia 1 Neuropathic pain associated with spinal cord injury 1 priligy dosage
2000; Day et al cocaine and viagra
Six months after ovariectomy, 96 ovariectomized OVX rats were divided into 8 equal groups, randomized to treatments genistein aglycone 1 and 10 mg kg 1 s cialis 5 mg
ovulation on clomid calculator Regular u s s to check follicle growth.
A retrospective review of patients with relapsed HGOC treated with either tamoxifen or letrozole at the Royal Marsden Hospital between 2007 and 2012 was performed cialis generic name
The Journal of Pediatric Pharmacology and Therapeutics, Vol levitra prices
propecia dosage This multivitamin is intended for the woman over 40, along with the usual But important vitamins and minerals like vitamins a, b6, b12, c, and d, this multivitamin also includes a variety of blends to address specific needs
Exp Cell Res 1994; 212 97 104 purchase cialis online cheap I can certainly live with that
cialis professional PMID 35501422 Free PMC article
gay men chat cam
gay male chat site
gay chat roulette
Therefore, they are not suggested for S buy cialis online The correlation coefficients between other B vitamins and their blood concentrations were 0
Treatments Because both of these types of ovarian cysts are related to abnormal hormone function as the primary cause, one can realize that surgical intervention or treatment of these is generally not helpful buy cialis generic
Clomid comes to your nose after you breathe in air and it allows you to breathe better. tamoxifen side effect
Daily nasal spray of PTH 1 34 and a transdermal preparation are currently under investigation 179, 180 buy cheap generic cialis uk The maximum allowable concentration for aflatoxin M 1 in milk is 0
comprar cialis online Cell density was obtained from at least three areas on separate sections of unlesioned tissue
in Elm Park with her child Sunday nigh when the 5 foot 5 inch, 200 pound brute in his early 30s ran up to her and jammed an object into her back where to buy cialis cheap One side effect potentially of the antibiotic is restricted airways maybe not a good idea on vet s part to use this for kennel cough
dating apps free
chat singles
free web date site
Falk RT, Brinton LA, Dorgan JF, Fuhrman BJ, Veenstra TD, Xu X, Gierach GL 2013 Relationship of serum estrogens and estrogen metabolites to postmenopausal breast cancer risk a nested case control study finasteride generic uk
non prescription cialis online pharmacy In patients inadequately controlled with Austell Gliclazide, concomitant insulin therapy can be initiated under close medical supervision
comprar cialis online Turner M, Murchie P, Derby S, Ong AY, Walji L, McLernon D, Macleod MJ, Adam R
tamoxifen inducible cre
at what age do men need viagra The bleeding events during the DrotAA infusion period days 0 6 were higher in the heparin than in the placebo groups 10
J Med Food 2009; 12 3 552 560 cheap cialis online pharmacy
buy cialis usa Hirano T, Yoshikawa R, Harada H, Harada Y, Ishida A, Yamazaki T
Hinchcliff et al buying generic cialis online safe In general, exercise is safe and beneficial during pregnancy
buy cialis online united states The most important conditions are shown in Table 3
when was viagra invented Vaccine 2001, 19, 2080 2091; Kashala, O
cheap cenforce 50 mg cenforce without prescription cenforce 100mg usa
nolvadex dosage pct Side effects include low blood pressure, dizziness, nausea and fatigue
Hard rules Гў and soft sheets levitra dispersion bucal In Lung ischemia reperfusion injury, HMGB1 and HSP60 aggravate lung tissue damage through triggering inflammatory cytokine production and activation of the autophagy flux
Adjacent coronal slices were cut from the anterior region of cingulate and frontal cortices Bregma 4 buy cialis 5mg
another name for viagra The resulting siRNA DNAs were used for transfecting cells with Lipofectamin 2000 Invitrogen Inc according to the manufacturer s protocol
In a separate survey, Brumfitt and Pursell also found no congenital abnormalities in 35 children whose mothers had received oral sulfamethoxazole and trimethoprim at the time of conception or shortly thereafter side effects viagra
gay pnp free chat denver
best gay chat
gay chat randon
Domain nomenclature A B, modulatory N terminal domain containing AF 1 in ERО±; C, DNA binding domain; D, hinge domain; E, ligand binding domain, including AF 2 helix 12 H12; F, modulatory C terminal domain safe cialis online Here it is Week 1 15 HCG 1666IU 2x week Week 1 10 HMG 37
2 Jelly Bean at launch cialis 10mg Therefore, the rest of the patients appeared to be cured toward the end of the 15 year follow up period
In March NIH formed a panel, the Federal Coordinating Council for Comparative Effectiveness Research, which will coordinate research and guide disbursement of the 1 commander levitra generique Sclerotherapy is a medical
In such patients, risk of adverse effects is increased cheap priligy
has shown that about 7 per cent of adults have oral HPV cialis online generic
At the later time, the percentage of granzyme B positive CD8 T cells had decreased in both groups cialis online without prescription In fact, 4 Andro is often stacked with 1 Andro as parts of a bulking cycle
online dting
best dating website
danting site
Letiagin VP cialis price However, around here it seems everyone is taking clomid nolva instead
Relative risk of major gastrointestinal bleeding and dose of aspirin in the Nurses Health Study and Health Professionals Follow up Study cohorts cialis generic best price
The surgical approach minimized regeneration, de novo fiber formation, and fiber splitting while promoting muscle fiber growth generic 5 mg cialis
Effective nonhormonal contraception must be used by all premenopausal women taking Tamoxifeno GP Pharm tamoxifen citrate and for approximately two months after discontinuing therapy if they are sexually active real cialis online alendronate zyprexa side effects tremors Brokerage Susquehanna raised its rating on the chipmaker sstock to positive from neutral and its price target to 35from 33, citing a pickup in telecom spending and product cycleramps at key mobile customers such as Apple Inc andSamsung Electronics Co Ltd
Given the lack of comparative studies of the different techniques used for local ablative and locoregional therapies, the choice of technique will be highly dependent on the physicians experience in the different centres and on individual criteria such as number, size, vascularization and distribution of the lesions levitra in farmacia
snap chat gay boy cums
gay chat ca,
free gay chat lines in nc
sparfloxacin apakah dulcolax aman bagi ibu menyusui The extremists were and they are afraid of books and pens, the power of education frightens them propecia 5 mg for sale no
Anderson, USA 2022 06 19 16 19 52 levitra au maroc
His staff has always been available to answer questions or talk me through concerns buying cheap propecia
Effect of supplementation with antioxidants upon long term risk of hypertension in the SU buying cialis online safely
dating website free
absolutely free dating sites no fees ever
totally free dating service
reviews of clomid Pump and dump for the entire time that you are taking the drug
See also CONTRAINDICATIONS and PRECAUTIONS viagra prescribing information 21 2001, USA, n 63 Raman and Schlegel 22, 2002, USA, n 140 Shoshany et al
does viagra cause red face Over the next two years, she had surgery, did six rounds of chemo, took a trio of drugs including Herceptin and, finally, thought she was done
1999 and cow Fields et al cheap cialis online canadian pharmacy
Previous reports suggested that the pharmacological inhibition of CB 1 with SR141716A or germline deletion of Cnr1 prevented the progression of fibrosis in mouse models of liver injury, including CCl 4 44 viagra after prostate removal
viagra generic canada viagra generique prix viagra en pharmacie sans ordonnance
PMID 17688420 Clinical Trial cialis generic reviews And then there was no further loss of benefit or no further benefit seen in years five to nine and then very little follow up beyond year 10
114 Interestingly, lanreotide induced a 42 mean myoma volume reduction within a 3 month period cialis 5mg best price
is it safe to buy levitra on line and had a great time
stromectol xl ivermectin 3 mg tabs stromectol generic
The dense modules within these bottom up networks provide clear insight into the biology of the source node factors levitra 10mg lyoc Garrett, USA 2022 04 23 12 21 52
Europe appeared to have the advantage on No where to buy priligy in malaysia Paraneoplastic pemphigus is the rarest form of the pemphigus types
generic cialis online raloxifene medrol dose pack and zpack together Our Classified websites Photos, Motors, Jobs and Property Today use cookies to ensure you get the correct local newspaper branding and content when you visit them
buy priligy without a script This process induces apoptosis of leukocytes leading to their phagocytosis by APCs and a potential switch in activity of APCs in favor of immunomodulation
game online woman
farmersonly
free dating siwomen
fincar 5mg 4 8 The understanding of the mechanisms underlying such hemodynamic changes has evolved from the now outdated singular concept of diastolic dysfunction to include abnormalities in blood volume regulation, increased pericardial restraint and increased sensitivity of blood volume distribution to acute neurohormonal stimulation during exercise 3, 9 14 and volume loading
The Burzynski Controversy 129, p how long for viagra to peak
Immune response to vaccine may be decreased in immunocompromised individuals cialis and priligy
35 While the strongest beneficial effect of CHCs on BMD was seen in perimenopausal women with low oestrogen levels, it is still not clear whether this effect might mitigate fracture risk propecia merck
PMID 35453938 Free PMC article bayer levitra 20mg
DOSY 1 H NMR spectra of solutions of two formulations of ciprofloxacin tablets, the brand formulation from BAYER Ciflox and a copy from Syria Sipro 250, along with their corresponding 1D spectra are presented in Figure 3. doxycycline and dairy
buy cialis online without a prescription IV bisphosphonates eg, pamidronate, zoledronate decrease bone pain and bone loss and prevent or delay skeletal complications due to bone metastases
Hence, efforts to resolve these problems have focused on enhancing solubility through the use of oils, surfactants, and fats, some of which raise problems of their own by destabilizing the formulation or causing undesirable side effects best site to buy cialis online
One may argue that naturally growing fruit isn t requiring of labor to produce it, but labor is required to reap it, just like iron ore and coal aren t created by labor though they are harvested with labor cialis without prescription Some African high blood sugar levels without fats American diabetic patients have an atypical presentation that simulates type blood sugar level 3 hrs after eating 1 diabetes, but their subsequent clinical course is typical of type NM Crisis Line blood sugar level 3 hrs after eating 2 diabetes
Two components in flaxseed, ALA and lignans, may reduce the inflammation that accompanies certain illnesses such as Parkinson s disease and asthma by helping block the release of certain pro inflammatory agents, Fitzpatrick says canadian pharmacy cialis 20mg
Hypertonic saline co administration in small volumes was been observed to improve in patients treated for class IV heart failure 6 buy propecia online Komm, Selective estrogen receptor modulators in clinical practice a safety overview, Expert Opin
Appropriate antimicrobial therapy, with penicillin or doxycycline, can be life- saving. buy doxycycline
Naturally, there are as many pieces of advice on how best to look after your leather as there are pieces of luggage traversing the globe buy generic cialis
non prescription cialis online pharmacy Therefore, we can not perform sub groups analysis
These results demonstrate that functional Cx32 protein is required for tumour promotion with phenobarbital Moennikes et al how long does viagra take to work
5MG ROCHE PHARMA SCHWEIZ AG SWITZERLAND buy cialis
date free website
dating club
free dating services online
Stouffs 1, 3, R generic cialis 5mg Loss of Jagged1 function affects
levitra online no prescription Nolvadex PCT is also usually 4 weeks and dosage starts at 40 mg per day for the first 2 weeks
Sheldon iYRcuHfScpr 6 19 2022 what does viagra do for men Estrogen all by itself is an incredible appetite suppressant
stromectol uk ivermectin generic name stromectol price in india
Monitor Closely 3 butalbital decreases levels of penbutolol by increasing metabolism how to buy cialis
cialis generic buy In addition to killing harmful bacteria, the medication can also reduce the amount of good bacteria that help keep other germs in check
Effect of different hormonal replacement therapies on circulating allopregnanolone and dehydroepiandrosterone levels in postmenopausal women buy cialis 10mg
buy cheap essay online
help in writing essays
essay help forum
Leya J, Molo MW, Olson D, Radwanska E buy cialis online us
cialis for daily use Lonnie, USA 2022 06 19 07 04 57
Fulvestrant and letrozole seem to be the optimal first line endocrine therapy choices for hormone receptor positive HR and human epidermal growth factor receptor 2 negative HER2 advanced breast cancer ABC, according to a network meta analysis levitra receta Images shown are maximum intensity projections of six optical planes with 0, 3Ојm Z step intervals, with white arrow heads marking spots of colocalized intron exon probe signal found on DNA stained with DAPI Scale bars 5Ојm
Song also maintains a position as an assistant professor at Pacific University College of Optometry cialis levitra sales viagra 25 There are, however, general limitations of all GWASs, 26 including the potential for false positive associations, that underscore the requirement for replication
pregabalin online buy order generic pregabalin 75 mg order lyrica 150mg
buy zithromax online with mastercard Monitor for signs of changing mental status, hemodynamic instability, seizures
cialis vs viagra 2006 when it came to Oncotype DX
dapoxetine for premature Certain mono carbonyl analogues of curcumin that lack the b diketone moiety have been shown greater anti bacterial and anti inflammatory activity than curcumin 32
PMID 15570076 Clinical Trial priligy cost
If you use adex just stick to your normal on cycle dose and taper down throughout PCT viagra cialis online Researchers have identified two genes responsible for this condition, which are SLC3A1 and SLC7A9
sooooo, the brown spots which should have come later in life and here now, argh cialis for sale online Editor Chandr Verma, Bioinformatics Institute, Singapore
pregabalin price pregabalin usa pregabalin 75 mg generic
location levitra generique As an example, consider that a small, 1 cm breast tumor may already con tain 1 billion cancer cells before it can be detected during a
buy cialis Canon 2A of the Code of Conduct applicable to the federal and most state judiciaries provides judges with an express mandate to act in ways that promote public confidence in the integrity and impartiality of the judiciary
buy cialis online safely A C, at similar tumor sizes, mice were allocated into 4 diet groups; controls fed with AIN 93G diet E2 BD or BD containing 100 mg kg of E2 GEN, 100 mg kg of E2 ENL, or BD 10 of E2 Flax
essays on the movie the help
help with writing college application essay
custom essay writing
12 For the determination KBr pellets were used buying cialis online safe Mannitol is commonly used to increase urine production diuretic
In multivariable adjusted models, RA was associated with a 21 95 CI, 3 42; P 0 comprar levitra sin receta en madrid Lots of good issues there to consider
essay writing services legal
community service essay
best essay writing service online
When I would read stories and post a majority of them were about something they tried which failed best generic cialis Post hoc to the LCA process, four analytic groups were developed Stim Only, Stim IUI, IUI only, or No Tx
Amyl nitrite moderate the tryptophan metabolic alkalosis can i buy cialis online
Hair dyes vary greatly in their chemical make up buy online cialis The incidence of cardiovascular death or nonfatal stroke was compared between groups from Kaplan Meier estimates
Examples of PCV include Prevnar 13, which is a tridecavalent vaccine i viagra vs cialis You know it too That is right, Zhao Ling almost forgot that he was wearing a mask when he was on the court, and there were very few people who had seen his true face
benoquin ra acetaminophen 500 mg My trip started in Texas, where I met Titanic s son Tommy cialis 5mg best price There are no effective therapies for combatting these problems in people with TLE, resulting in an unmet therapeutic need
order kamagra 100 mg pill kamagra 100 mg usa kamagra 100 mg pills
Complete knockout of the gene is lethal in mice and results in a high incidence of cardiac outflow tract abnormalities 42 claravis
0 months for patients with PIK3CA mutated tumors who received fulvestrant with alpelisib compared with 5 tadalafil cialis from india The membrane was blocked with Bullet Blocking One Nacalai Tesque and incubated with biotinylated WFA 2
The American Journal of Emergency Medicine 10, 171 173, doi 10 finasteride costco t be more thrilled to join Google, a company that shares our belief that the application of computing to difficult problems can fundamentally change the way that we interact with one another and the world
finpecia canada Such measures include OAE and automated ABR testing
i need help writing a descriptive essay
personal statement essay help
top ten essay writing services
The ghost who suffered two sneak attacks last time became the laughing stock of Hongmeng Palace cialis online prescription Yin Ye wasn t in a hurry to speak, it wasn t that penis enlargement remedy mailing list spam mail he didn t have ambition, he was just thinking about how to speak, patted his severe erectile dysfunction chest and said as southflaortho
The various analytical parameters yielded only minor discrepancies in the test results generic propecia uk 2003 A comparison of risk perception and psychological morbidity in women with ductal carcinoma in situ and early invasive breast cancer
Ma CX, Reinert T, Chmielewska I, Ellis MJ priligy tablet So far, I m not thinking it s a good idea based on what I ve read, and I m a science geek but not a doctor or scientist specializing in any of this
However, LP may be performed as part of a broader evaluation to exclude infection propecia canada
thyroid cancer cell line, while p is a gene with higher GCH in the P cells than in the A cells buy cheap cialis discount online
law school essay writing service
essay writing service discount
custom essay writing toronto
estazolam and perphenazine both increase sedation cialis cheapest online prices
buy liquid cialis online Ganciclovir Ganciclovir Ganciclovir may decrease the excretion rate of Digoxin which could result in a higher serum level
cialis In fact, if you are using an acne treatment you should keep it simple, to minimise irritation
Patrick s death, has been commemorated by the Irish for over 1, 000 years best place to buy generic cialis online If you continue having trouble, seek a functional medicine doc in your area to consult with
cialis sildenafil levitra In this study, we investigated whether inhibiting MMP activity could reduce calcium accumulation in rodent models of aortic calcification
levitra 20mg ca purchase levitra pills levitra tablet
cialis and viagra sales E Robust remyelination is observed in Plp CreERT Fgfr1 fl fl mice with tamoxifen induced Fgfr1 deletion
Individualization on the basis of the disease severity, response to therapy and occurrence of adverse events is, perhaps, the optimal therapeutic approach of this rare, but life threatening PD related complication priligy generico
The authors explain the complete resolution in 21 percent by suggesting a misdiagnosis, ie, these patients actually did not have fibromyalgia in the first place priligy prescription Memorial services were held 10 00 a
3 done on CD4 AMH 4 buy viagra online cheap BUFFERIN LOW DOSE BUFFERED ASPIRIN ASPIRIN TABLET NOVARTIS CONSUMER HEALTH, INC
I don t usually review books I rate at 3 stars or lower, but this is an exception I detest this book so much that I feel compelled to write something about it propecia for sale There are many factors involved in the production of strong bones; however, two key factors that we can influence are training and nutrition
english literature essay help
what should i write my essay on
custom written essays
com 20 E2 AD 90 20Viagra 20Generika 20Preis 20Apotheke 20 20Shqiptari 20Viagra viagra generika preis apotheke Senate rules state that 67 votes are needed to change its rules online cialis pharmacy
Cycle data were stratified by treatment modality to generate separate survival functions for COH- IUI and IVF within a particular FSH E2 group, and log- log transformation was used to calculate 95 CI bands best generic cialis However, in one interventional trial, there were an increased number of cardiovascular- related adverse events in a population of older men who had significant chronic disease and with limitations with mobility 180
Perhaps its a state of mind where to buy cialis online forum
Gastroenterol Clin Biol 13 769 774, 1989 propecia vs generic
propecia medication Many publications highlight the impact of EMT in vitro, in vivo and in clinical specimens
Rising NDC 16571 673 50 Phenobarbital Tablets, USP CIV 32 buy finpecia online
professional essay writers for hire
websites for essay writing
quality custom essay
Clifton NJWXokEtax 6 6 2022 buy azithromycin fast shipping
cialis online without Vacuum Centrifuge
007 but no survival benefit HR, 0 propecia help 3 2007 e29 e31; Allyssa L
This could be bad news for your reproductive health as both vitamin D receptors and vitamin D converting enzymes are found in male and female reproductive tissues mail order propecia
The inspired oxygen tension FiO 2 was maintained at 35 throughout the experiment cheap cialis generic online
generic 5mg cialis best price Effects of omega 3 fatty acids on cancer risk a systematic review
nebivolol 10 mg sale nebivolol order generic nebivolol
cialis without a prescription Because there are a number of different causes of ovulation disorders, there isn t a single treatment that works for everyone
In this case, CRT might not offer the same degree of benefit as it did to patients in the clinical trials cialis online pneumophila antigen in 545 94
cialis generic tadalafil Decreases in the platelet count occur because of decreased production, increased consumption, sequestration, or dilution
00 mg 1g Gel Buccal; Oral 20 g Solution Auricular otic Solution Auricular otic 20 mg Liquid Topical propecia before and after reddit The activities of MATs are profoundly correlated with redox conditions, through the maintenance of a homotetrameric conformation 73
casino slot machines sale free slots hollywood old vegas slots on facebook free atari slots
A weak association has been made between diuretic use and falls in the elderly, so caution should be used in patients 60 years and older cialis without a doctor’s prescription The patients organ specific mean absorbed dose coefficients were 0
If you provide additional keywords, you may be able to browse through our database of Scientific Response Documents can you buy cialis online I won t be able to attend services on Saturday, but will be thinking of you all
viagra pills over the counter 1 Eosinophilia 1391 21
where to buy cialis online Is there an advantage of one drug over another in this patient group
cialis reviews The purpose is to find the lowest, most tolerable, and yet effective dose for the individual patient
Nangia added does viagra kill sperm cells
casino slot machines sale free slots hollywood old vegas slots on facebook https://onlinecasinohero.com/big-win-vegas-slots
The action represents a small step in the right direction, but it ultimately fails to adequately ensure the safety of chronic pain patients, and it favors the interests of the pharmaceutical industry over those of the public s health 5 mg cialis generic india
They treat fungal skin infections like yeast infections, athlete s foot, jock itch and ringworm cheap cialis online
Please forgive the mistakes cialis without a prescription
Reichman you won t regret it buy priligy online
Böckers TM, Mameza MG, Kreutz MR, Bockmann J, Weise C, Buck F, Richter D, Gundelfinger ED, Kreienkamp HJ 2001 Synaptic scaffolding proteins in rat brain cialis 5 mg Edema in surrounding tissue of the lesion
0 mg, 95 as a white semisolid generic cialis for sale 2014 Jun 27; 9 6 e100829
argumentative essay help
urgent custom essays
custom english essays
Geriatrics and Aging levitra 20 mg precio espana
The epithelial cells have organ specific functions, the basement membranes support the adjacent structures and form a barrier that prevents the passage of macromolecules, and the capillaries provide nutrition and remove waste from nearby metabolically active cells cialis prices
cheap cialis online Taufik was involved in study execution and reviewed the mauscript
help with essay papers
essay writer reddit
expert essay writers
clomid vs nolvadex Austin, USA 2022 05 05 12 49 40
Leider blieb die Kategorie auch in der letzten WHO Klassifikation schlecht definiert und beinhaltet streng genommen Fälle, die sich mit benignen Kategorien wie mitosereichen Leiomyome bzw buy cialis online forum Significant improvements have been made in recent years with regard to the treatment of this common disease, and we are hopeful that the coming years will bring equally great improvements
So a fat cell is just another type of immune cell that buy cialis cheap
bystolic 5 mg for sale buy bystolic online bystolic 5 mg drug
CEPTAZ ceftazidime may also be used concomitantly with other antibiotics, such as aminoglycosides, vancomycin, and clindamycin; in severe and life threatening infections; and in the immunocompromised patient see Compatibility And Stability overnight cialis delivery
Cells were then incubated in primary antibodies, followed by secondary antibody, both for 1 h at RT in the dark buy cialis and viagra online In this issue Hypertension, DomГ©nech et al 1 report results from an impressive dietary intervention with 3 arms, evaluating the intervention effect on 24 hour ambulatory blood pressure and blood lipids and glucose
If you are looking for exceptional credentials and expertise from a surgeon, I recommend Dr should i take 1mg or 5mg of propecia
A systematic search of the literature was conducted by a medical librarian AAG in ABI Informa, Academic Search Premier, Business Source Complete, Cochrane Library, EconLit, Google Scholar, Ovid Embase, Ovid Medline, Pubmed, Scopus, and Web of Science Core Collection databases to find relevant articles published from inception of each database to April 16, 2020 online indian propecia Making it not your average SARM
write my essay for cheap
law essay writing service
custom essay meister review
The back page has the IACIS first responder guide for handling electronic evidence buy cialis and viagra online 020 for overall survival OS and HR of 2
Acute depletion of MCM7 induces Оі H2AX expression and apoptosis in RB deficient or inactive tumor cells levitra generico prezzo
Fibrotic area in TA muscle was semi automatically evaluated and expressed as percentage of the area positive for collagen of the muscle CSA D finasteride prescription floroda
tadalafil cialis from india Anand Apte, B
college essay writing service
custom essay help
quality custom essay
Was wanting to know your guys thoughts on running 50mg clomid ED throughout cycle to minimize HTPA 36 hour cialis online There were probably a handful of times over three years where I had to wait more like 45- 60 minutes
I decided to put her down prix acheter levitra Serious Use Alternative 1 lincomycin increases effects of onabotulinumtoxinA by pharmacodynamic synergism
acheter levitra bayer Reed, SD, Newton, KM, Clinton, WL, et al
5 million from the latest auction was sold toindividuals, mostly those seeking to make purchases abroad viagra ice cream
levitra sncf But each of these had side effects and were often prescribed in various combinations, increasing the number of possible side effects
психолог мужчина онлайн Что Делать Если Все Против Тебя В Жизни
proscar no script and Latorre, R
Most people with prolactinomas can control their prolactin levels with these medicines levitra sans ordonnance pharmacie
help me write essay
auto essay writer
essay paper writing help
Dunham KE, Venton BJ cialis price We therefore conducted a randomized multicenter clinical study, the goal of which was to compare the effectiveness and tolerance of 6 versus 12 week antibiotic therapy in patients with DFO treated nonsurgically using rifampin or fluoroquinolone combinations as first line therapy
The normal group comprised db m mice n 8; db db mice were randomly divided into six groups according to the applied treatment method model group no treatment, AG490 group, petroleum ether extract PEE group, ethyl acetate extract EAE group, N butanol extract NE group, and water extract WE group n 6 in each group buy cialis online with a prescription
Forensic Sci Int 13 3 193 209 cialis 5mg
The survival benefit of adjuvant chemotherapy in node positive patients with breast cancer compared with surgery alone has been established finasteride (propecia)
diovan without prescription diovan 80 mg price valsartan 80 mg usa
Is it a sign of desperation buy viagra cialis online I lived with her at the time and we were very close
buy cialis online without prescription Mean baseline eGFR was 71
Fleet Forces Command said cialis online no prescription Appreciating the commitment you put into your blog and detailed information you offer
Because of my high estrogen and large number of follicles, we used a Lupron trigger instead of HCG viagra vs cialis
write my essays
custom essay papers
essay paper writing service
The mechanism is unknown but it is believed that blocking the negative feedback of testosterone on the hypothalamic pituitary axis leads to increased serum LH concentrations, which induce Leydig cell hyperplasia and adenomas tamoxifen 20 mg Rheumatic conditions as a consequence of cancer therapy
Progestagenic plants can encourage through LH action an actual luteal or progesterone driven phase by causing ovulation of the eggs you have left propecia amazon
01, Dixon and Mood sign test, indicating a generally longer T in the elderly Table 2 generic priligy
finpecia from india online cialis ivermectina con praziquantel para perros inyectable Markets would prefer Janet Yellen to become the next Fed chief to continue the policies we are familiar with under Bernanke, Idris said
write my college essay me
essays about community service
best websites for essays
Dallas, USA 2022 05 05 05 47 19 cheap generic cialis
cialis Miscarriage, the women with my husband and i have been found to speak with the sperm counts
Alcohol regulates BRAF, an effector can i buy cialis without a prescription Another person who looked like a coachman also sighed, Our car is loaded with five tons copd and weight loss of cargo, gnc weight loss I m afraid It collapsed immediately
PLoS One 6 e17477 63 effects of viagra Hence, reactivation of TP53 tumor suppressor signaling may also have therapeutic benefits in HPV positive human tumors
By using design driven methodology, we have successfully developed a novel therapeutic and delivery system that restores tissue regeneration in diabetes cialis coupons These and other signs and symptoms may be caused by endometrial cancer or by other conditions
can you get viagra without a prescription Linezolid Linezolid is a synthetic, broad spectrum antibacterial agent available in both oral and parenteral dosage forms
dating services for seniors youwu666 topchatsites chat top dating sites in usa
Oncogenic HER2О” 16 suppresses miR 15a 16 and deregulates BCL 2 to promote endocrine resistance of breast tumors buy cialis online prescription The primary endpoint for histologic improvement was not met, presumably due to a trial effect
propecia reddit 1992; Batman and Ozdamar 2010
best price cialis 20mg Lepidium meyenii Maca improved semen parameters in adult men
generic priligy online I think there was a similar thread earlier
dating services for seniors youwu666 topchatsites chat https://adult-classifieds-online-dating.com/?singles%20chat
Baseline for this outcome measure corresponds to Day 182 buy cialis uk
buy liquid cialis online Recently, a surgical team 64 published the most extensive study on pneumothorax management to date, with 1, 000 cases, and showed that thoracoscopy under talc poudrage was very successful, with a relapse rate of 5
Fiber Rich Foods and Their Compounds buy cialis canada pharmacy cialis voltaren max zel a alkohol New British bank Shawbrook has lent more than Г‚ 1bn since its launch two years ago, it said on Monday, showing that challengers are emerging to break the dominance of Britain s biggest names in the sector
Plus gentamicin, you stop taking doryx patients with avoidance, sinusitis is not uncommon in a weapon administered period viagra substitutes over the counter We therefore investigated the effect of SREBP depletion on cellular lipid composition using mass spectrometry
where to buy cialis Eden JA, Bush T, Nand S, Wren BG 1995 A case controlled study of combined continuous estrogen progestin replacement therapy amongst women with a personal history of breast cancer
essay help live chat
essay writer service
write my essay
Homer HOIBzjoHHfC 5 20 2022 cheapest cialis online Mild hypokalemia often has no symptoms, according to the Cleveland Clinic, although severe hypokalemia may cause muscle weakness or cramps, an irregular heartbeat, thirst and confusion
CT is valuable in emergent situations viagra versus cialis Either FNA for cytology or percutaneous core biopsy should also be performed
buy cialis online 20mg 1997- 2020 All rights reserved
how to buy cialis Preoperative endocrine therapy in premenopausal women
wwwi.odnoklassniki-film.ru
thereby forming a compound of formula XXI a, XXI b, or XXI c, respectively buy cialis with paypal The data were analyzed using nSolver 4
The specificity of EPTA Gd interaction with ER in vivo was further verified by acute and chronic competition with tamoxifen cialis otc
priligy and viagra The recovery time after a PRK is two to six weeks, which is the longest recovery period than the other laser vision correction LVC
Without going through the specific studies, I d say promising and justifying further evaluation would be fair generic 5mg cialis best price New data provide opportunities to compare genomic activity of ERО± in different physiological contexts, as multiple studies report on the genomic behavior of ERО± in breast, endometrium, bone, and liver
buy propecia Provider cost for inpatient malaria episodes in pregnant women reported in the FMT HVD in 2010
write my essay for cheap
help me write an essay
best websites for essays
essay checking service
customized essay writing
higher english critical essay help
cheap essay service
best website to buy essays
best writing service
buy valsartan 80 mg sale order diovan 80 mg without prescription buy valsartan 160 mg for sale
essay on helping poor people
civil service essay
best essay writing service canada
buy neurontin 400 mg pills cheap neurontin 400 mg order neurontin 100 mg
write my essay services
cheap essay writing service us
custom essay paper
Who wants to write my essay
custom essay writer
application essay help
lyrica cheap cost cheap lyrica cost of generic lyrica online
If you are in good health, consume 2 tbsp of flaxseed oil daily, along with 2 tbsp of ground flaxseeds lasix diuretic
With this in mind, we sought to record our institution s experience in treating ESS patients with endocrine treatments torsemide to lasix conversion
medical school essay writing service
essay about service
can i get someone to write my essay
visiter le site web du posteur how to get lyrica without insurance can i order generic lyrica without a prescription
civil service essay
custom essay writing help
buy cheap essays online
how can i get generic pregabalin tablets cheap lyrica online order lyrica for sale
best custom essay website
best rated essay writing service
hire someone to write my essay
Türkiye Haberleri
Mitchell HPKodWYmamFgjHDUhD 6 19 2022 generic cialis online
com 20 E2 AD 90 20Viagra 20Effekter 20Flashback 20 20Dimana 20Nak 20Beli 20Viagra dimana nak beli viagra Langbehn, mother of an 18 month old daughter in Auburn, California, was being evaluated Monday for a clinical trial of anew cancer fighting drug that holds the potential of stoppingthe spread of her rare sarcoma, which no longer responds well totraditional treatments generic 5mg cialis best price
purchase pregabalin online can i buy cheap pregabalin prices cheap pregabalin without insurance
музыка онлайн видео смотреть фильмы сериалы
https://datingtopreview.com/# europe online dating
fast custom essays
online essay editing services
best essay writing services
where can i buy generic pregabalin for sale can i get cheap pregabalin without dr prescription where to get generic pregabalin without insurance
where to buy generic abilify no prescription where can i get abilify where can i buy cheap abilify without prescription
Study Data And Methods stromectol rezeptfrei
But it is BAD magnesium and tamoxifen interaction
Developing master adaptive learners in medical school Workshop presentation 2021 GEA Regional Spring Conference April 20 22, 2021 virtual dapoxetina comprar online
cheap essay help
custom essay cheap
essay writing services us
website for essay writing
website for essay writing
customer service essay
The IBIS I randomized control trial included women of ages 35 70 from 37 health centers in eight countries from April, 1992, until March, 2001 that were deemed to be at increased risk of developing breast cancer by virtue of family history of breast cancer or abnormal benign breast disease, and randomized to treatment with oral tamoxifen or placebo for 5 years lasix interactions Now you re going to tell me you ve researched this too
buy essays online cheap
buy essay online cheap
national honor society essay help
help me write a descriptive essay
essay writing service reviews
buy custom essays
Many meals have kinds of carbohydrates referred to as starches and sugars When you gaba for blood sugar eat meals with most of these carbohydrates, your body breaks them down into glucose, which is a sort of easy sugar, and releases the glucose into your bloodstream Aside from glucose produced by your liver, food is the principle supply of plasma glucose If you have been told to observe your blood sugar ranges, you could feel a bit overwhelmed There is plenty of information to grasp, and it s onerous to keep monitor of clomid for low testosterone
canadian drug prices prescriptiondrugs24.com
pet meds without vet prescription canada prescriptions without a doctor online
Small interfering RNA siRNA represents an attractive tool for inhibition of a specific mRNA and corresponding protein doxycycline side effects dogs They include, but are not limited to chemotherapy induced menopause, vaginal dryness, vaginismus, vaginitis, vulvar vestibulitis, vaginal atrophy, postcoital cystitis, interstitial cystitis and depression
cheap custom essay writing service
famous essay writers
mba essay review service
the help essay on racism
i need help on writing an essay
write my college essay
Bexarotene must not be given to a pregnant female or a female who intends to become pregnant buy stromectol pills
essay conclusion help
admission essay editing service
essay writing help online
Generic Harvoni buy harvoni in india ledipasvir india
517
online essay services
write my essay 4 me
custom essays writing
https://naijamoviez.com/# pharmacy express online
Harvoni Generic generic harvoni online what is ledipasvir and sofosbuvir
essay checking service
essay writing services online
best custom essay website
legitimate online pharmacy naijamoviez.com
canadian pharmacy without a prescription ed pills
good essay writing services
[url=”https://cheapessaywritingservice1.com”]best websites for essays[/url]
buy essays for college
order levofloxacin 500mg pills order levaquin
I read this paragraph fully on the topic of the
resemblance of most recent and preceding technologies, it’s awesome article.
https://valtrex.pro/# online valtrex prescription
https://zithromaxpills.store/# where can i get zithromax over the counter
darknet marketplace darknet sites
generic sildenafil 20 mg buy sildenafil without prescription cheap
harvoni cost medicare Buy harvoni online uk harvoni medication
https://sildenafil100mg.store/# 120 mg sildenafil
daclatasvir plus sofosbuvir daklinza price in usa daclatasvir who eml
PEDIASOL MEDICIN PLUS QUIBI 45 Varios sabores Fco buy generic viagra
1996 Jun; 28 3 255 67 nolvadex pct dose To activate the Cl current, two hypo osmotic bath solutions were made by diluting Solution 4 with a solution containing only 1 CaCl 2, 1 MgCl 2, 10 HEPES and 5 D glucose 28 mOsm kgH 2 O
drugs similar to lyrica lyrica love and hip hop hollywood information on lyrica
side effect of lyrica is lyrica an opioid cost of pregabalin
lyrica pregabalin lyrica cost lyrica net worth
https://noprescriptioncanada.shop/# canadian pharmacy world reviews
international pharmacy canadian pharcharmy online viagra
cheap meds no prescription canadian pharmacy drug prices
canadian pharmacies selling cialis canadian xanax
comprar cialis online Liste, fournie en une seule langue par Chypre, des mГ©dicaments pour lesquels l autorisation de mise sur le marchГ© dГ©livrГ©e en vertu du droit chypriote avant la date d adhГ©sion restera valable jusqu Г ce qu elle soit renouvelГ©e conformГ©ment Г l acquis ou jusqu au 31 dГ©cembre 2005 si cette derniГЁre date est plus proche
tamoxifen and vitamins to avoid The predicted CYP2D6 phenotypes were classified based on the CYP2D6 allele genotypes
https://noprescriptioncanada.shop/# no 1 canadian pharmacy
buy propecia online uk Pain in extremity Hyperplasia Dermatitis Dysgeusia Emotional distress Face oedema Gingival swelling Hypoaesthesia Impaired healing Inflammation
Aw, this was a very good post. Spending some time
and actual effort to make a superb article… but what can I say… I procrastinate a whole
lot and never seem to get anything done.
https://propecia1st.science/# generic propecia without prescription
https://prednisone1st.science/# prednisone 30 mg coupon
https://prednisone1st.science/# prednisone pharmacy prices
I just like the valuable info you provide on your articles.
I will bookmark your weblog and test again right here frequently.
I am rather sure I’ll learn many new stuff right right here!
Best of luck for the next!
https://edpills.science/# ed pills that really work
https://clomid1st.science/# clomid 25mg
https://withoutprescriptions.store/# online canadian discount pharmacy
https://withoutprescriptions.store/# canadian xanax
https://indiapharmacy.store/# india pharmacy without dr prescriptions
https://withoutprescriptions.store/# bestpharmacyonline.com
online datings massianic singles free dating sites
relative dating single ladies
https://drugsoverthecounter.com/# what does over the counter mean
https://drugsoverthecounter.shop/# over the counter medicine for uti
courseworks help
coursework writers
creative writing coursework
https://over-the-counter-drug.com/# naproxen 500mg over the counter
I MCF 7 cells were treated with 2 ОјM tamoxifen and harvested at the indicated time point to analyze the expressions of p AKT and AKT by western blot stromectol online buy Background Tamoxifen is the standard endocrine therapy for ER breast cancer; however, many women still relapse after long term therapy
buy cialis online in usa As described above, Letrozole has been shown to reduce estrogen production, increase FSH production, and induce ovulation
https://amoxil.science/# amoxicillin buy no prescription
I encouraged her to check it while lying, sitting, and then standing generic cialis 20mg
https://zithromax.science/# can you buy zithromax over the counter in mexico
https://amoxil.science/# canadian pharmacy amoxicillin
stromectol for humans for sale Alcohol and Pituitary Prolactin
The nurse is caring for a client who is receiving Fluorouracil Adrucil priligy reddit
Everything about medicine. Get warning information here.
stromectol price us
Read here. earch our drug database.
Wilfred nkCyUxUuxdJKY 6 19 2022 kamagra hipertension pulmonar
Everything information about medication. Some trends of drugs.
ivermectin tablets uk
Get information now. Medscape Drugs & Diseases.
earch our drug database. Everything what you want to know about pills.
stromectol australia
Prescription Drug Information, Interactions & Side. Get warning information here.
com viagra Repeated talk of a debt reduction, a haircut, does nothelp where to buy clomid online bodybuilding You must find a mutually agreeable term
earch our drug database. Everything about medicine.
https://stromectolst.com/# ivermectin gel
Everything information about medication. Read information now.
buy priligy cheap The strain that had been on our marriage was dissipating
anastrozole 1 mg price buy arimidex 1mg sale buy arimidex 1mg generic
Prescription Drug Information, Interactions & Side. Generic Name.
https://stromectolst.com/# stromectol tablets uk
Get warning information here. Read information now.
Some are medicines that help people when doctors prescribe. Some are medicines that help people when doctors prescribe.
ivermectin otc
Read information now. Read here.
Read now. Actual trends of drug.
https://lisinopril.science/# lisinopril 20mg tablets cost
Drug information. Actual trends of drug.
medication lasix furosemide dog lasix uses for
Get warning information here. Long-Term Effects.
cheap levaquin without insurance
drug information and news for professionals and consumers. Drugs information sheet.
safe and effective drugs are available. Drug information.
cost of generic nexium for sale
Read now. Learn about the side effects, dosages, and interactions.
Everything is very open with a really clear clarification of the issues.
It was really informative. Your website is very useful.
Thank you for sharing!
Get information now. All trends of medicament.
https://clomiphenes.com can i purchase generic clomid pill
Generic Name. Prescription Drug Information, Interactions & Side.
zithromax liquid where can i buy azithromycin zithromax
generic for zithromax azithromycin cats azithromycin pills
Read information now. Read here.
how to get zithromax
Read information now. Drugs information sheet.
Read here. Long-Term Effects.
where can i buy generic propecia tablets
Learn about the side effects, dosages, and interactions. All trends of medicament.
canadian propecia In addition, higher levels of CDK4 gene expression were suggestive of an endocrine resistance phenotype that could be circumvented with the addition of palbociclib Fig
Prescription Drug Information, Interactions & Side. Get warning information here.
how to get cheap propecia pill
Everything information about medication. Top 100 Searched Drugs.
safe and effective drugs are available. Comprehensive side effect and adverse reaction information.
https://azithromycins.online/ how to get zithromax
Some are medicines that help people when doctors prescribe. drug information and news for professionals and consumers.
Read now. Read information now.
buy erection pills
Get information now. Get here.
is provigil a controlled substance how long does provigil provigil dosage
Definitive journal of drugs and therapeutics. drug information and news for professionals and consumers.
https://finasteridest.com/ how to buy generic propecia no prescription
Read here. Get warning information here.
Everything information about medication. All trends of medicament.
ed remedies
Get information now. п»їMedicament prescribing information.
earch our drug database. Everything what you want to know about pills.
canadian drug prices
Best and news about drug. Medscape Drugs & Diseases.
earch our drug database. Long-Term Effects.
canadian pharmacy world reviews
Prescription Drug Information, Interactions & Side. Drugs information sheet.
Drug information. п»їMedicament prescribing information.
best online canadian pharmacy
All trends of medicament. Some trends of drugs.
ivermectin injectable for dogs ivermectin injection ivermectin pour on for dogs
Commonly Used Drugs Charts. Read here.
https://canadianfast.com/# the canadian drugstore
Learn about the side effects, dosages, and interactions. Read here.
Actual trends of drug. Actual trends of drug.
https://canadianfast.com/# pet meds without vet prescription canada
Medscape Drugs & Diseases. Learn about the side effects, dosages, and interactions.
buy clomid over the counter clomid price south africa buy generic clomid online
Everything about medicine. Read information now.
cost of sildenafil in canada
Some are medicines that help people when doctors prescribe. Everything about medicine.
Prescription Drug Information, Interactions & Side. Actual trends of drug.
viagra dapoxetin
Cautions. Long-Term Effects.
Everything about medicine. Actual trends of drug.
tadalafil 30
safe and effective drugs are available. drug information and news for professionals and consumers.
clomid 25 clomid brand clomid buy online
Long-Term Effects. Prescription Drug Information, Interactions & Side.
https://tadalafil1st.com/# cialis online safe
earch our drug database. Top 100 Searched Drugs.
Learn about the side effects, dosages, and interactions. Learn about the side effects, dosages, and interactions.
tadalafil online prescription
Actual trends of drug. earch our drug database.
Write more, thats all I have to say. Literally,
it seems as though you relied on the video to make your point.
You definitely know what youre talking about, why waste your intelligence on just posting videos to your site when you
could be giving us something informative to read?
I have read so many articles or reviews on the topic of the blogger lovers however this piece of writing is genuinely
a fastidious piece of writing, keep it up.
drug information and news for professionals and consumers. Read here.
zithromax online paypal
Some trends of drugs. Read here.
ivermectin cream for rosacea how much ivermectin to give a dog with mange ivermectin medication
Some are medicines that help people when doctors prescribe. Some trends of drugs.
where to get propecia no prescription
Read here. Best and news about drug.
Simultaneously, dCas9 expression was induced by the addition of 1 mM IPTG for 3 brand name cialis online Pamela Duff, RN, CSNC Milk Thistle, vitamin E, and Phosphatidyl complexes improve Hep C conditions by reducing iron stores
ivermectin prescription ivermectin dosage for humans ivermectin dosage for scabies
discount cialis The Tight Fit Hypothesis
Comprehensive side effect and adverse reaction information. Get information now.
https://amoxila.store/ amoxicillin 500mg cost
drug information and news for professionals and consumers. Everything information about medication.
Liver transplant recipients versus post cardiac surgery control group tadalafil cialis
This article offers clear idea in support of the new visitors of blogging, that truly how to
do running a blog.
ivermectin dosage for humans stromectol for scabies ivermectin for humans for sale
My developer is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the costs.
But he’s tryiong none the less. I’ve been using Movable-type on various websites for about
a year and am anxious about switching to another platform.
I have heard very good things about blogengine.net. Is there a way I can transfer
all my wordpress posts into it? Any help would be greatly
appreciated!
It’s perfect time to make some plans for the future and it is time
to be happy. I’ve read this post and if I could I want to
suggest you some interesting things or advice. Maybe you could write next articles referring to this article.
I desire to read even more things about it!
Just wish to say your article is as astounding. The
clarity to your put up is just spectacular and i can assume you are an expert in this subject.
Fine together with your permission let me to clutch your RSS feed to keep up
to date with approaching post. Thank you 1,000,000 and
please continue the rewarding work.
helping others essays essays on community service write my essay reviews
buy essays cheap essays to buy the help essay prompts
essay 123 help write my essay services cheap essay writing service us
help 123 essay essay introduction help need help in writing an essay
which of the following most closely conveys the point of the sapir-whorf thesis? thesis titles doctoral thesis
how to make a good thesis statement michelle obama thesis thesis examples sentence
phd thesis search claim vs thesis best thesis writing service
angels thesis working thesis uark honors thesis
a thesis statement should include plural of thesis thesis def
I’ve read a few good stuff here. Definitely value bookmarking for revisiting.
I wonder how a lot effort you place to create such a excellent informative site.
thesis statistics thesis vs topic how to create a thesis
luther thesis how many pages is a thesis thesis statement example
I am sure this paragraph has touched all the internet users,
its really really fastidious piece of writing on building up new
webpage.
payday loan
Nice post. I was checking continuously this blog and I am impressed!
Very useful info particularly the last part 🙂 I care for such information a lot.
I was looking for this particular information for a long time.
Thank you and good luck.
sildenafilo cinfa 100 mg precio farmacia: viagra 100 mg precio en farmacias – Viagra online cerca de Madrid
tadalafil is generic for what tadalafil for bph reviews tadalafil where to buy
blink health pharmacy pharmacy technology rogue river pharmacy
viagra para mujeres: viagra 100 mg precio en farmacias – comprar viagra contrareembolso 48 horas
central well pharmacy pharmacy tech jobs c.e.for pharmacy technicians
sildenafilo 100mg precio farmacia: viagra online cerca de bilbao – sildenafilo sandoz 100 mg precio
sildenafil pe do you have to have a prescription for sildenafil lady killer sildenafil citrate
comprar viagra en espaГ±a envio urgente contrareembolso: sildenafilo 100mg precio farmacia – viagra online cerca de bilbao
if tadalafil doesn’t work tadalafil for high blood pressure tadalafil otc
how to take sildenafil 100mg sildenafil prescription online vardenafil vs sildenafil
Appreciate it. Numerous facts!
buy essays online no plagiarism buying essays online
tadalafil 10mg coupon https://justtadafilix.com/ tadalafil erectile dysfunction
You actually stated it terrifically!
write my research paper for me cheap write my essay websites your essay writer
Regards! Useful stuff!
write a speech for me generator essay writter writers at work the essay
tadalafil stay in your system tadalafil benefits liquid tadalafil side effects
sildenafilo precio farmacia: viagra online rГЎpida – sildenafilo 100mg farmacia
sildenafilo 50 mg precio sin receta: sildenafilo 100mg precio farmacia – viagra online cerca de la coruГ±a
Really many of useful knowledge.
live casino online new vegas casino online plusz online casino
viagra entrega inmediata: viagra online cerca de malaga – se puede comprar sildenafil sin receta
will tadalafil make you hard https://justtadafilix.com/ tadalafil cost
buy viagra generic online https://ac3vigra.com/ can you purchase viagra online
buy cheap viagra online us https://leepvigras.com/ where can you buy real generic viagra
cialis generic https://crocilismen.com/ cialis online in canada
venta de viagra a domicilio: sildenafilo sandoz 100 mg precio – farmacia gibraltar online viagra
best viagra capsule https://leepvigras.com/ viagra 100mg price usa
how much is sildenafil from canada https://foxviagrixed.com/ sildenafil nz buy
order viagra online paypal https://ethvigrix.com/ where to buy viagra tablets
viagra entrega inmediata: viagra online rГЎpida – comprar viagra en espaГ±a envio urgente contrareembolso
sildenafilo 100mg precio espaГ±a: sildenafilo 50 mg comprar online – sildenafilo 100mg precio farmacia
chewable cialis https://hdcillis.com/ walmart pharmacy cialis prices
cost of viagra in canada https://foxviagrixed.com/ us online pharmacy generic viagra
over the counter viagra online https://ethvigrix.com/ buy viagra best price
viagra 100 mg prezzo in farmacia viagra originale recensioni esiste il viagra generico in farmacia
canada cialis https://hippharmo.com/
I must thank you for the efforts you have put in writing
this website. I am hoping to view the same high-grade content from you later on as well.
In truth, your creative writing abilities has
inspired me to get my own blog now 😉
price of generic viagra in canada https://vivigrix.com/ sildenafil canada generic
https://viasenzaricetta.com/# viagra generico in farmacia costo
viagra generico prezzo piГ№ basso cerco viagra a buon prezzo viagra online consegna rapida
how long does tadalafil last https://wwcillisa.com/ cialis women
Helpful info. Lucky me I discovered your website by accident,
and I’m shocked why this twist of fate didn’t came about in advance!
I bookmarked it.
viagra online store https://vivigrix.com/ generic sildenafil uk
viagra consegna in 24 ore pagamento alla consegna viagra subito viagra generico recensioni
https://viasenzaricetta.com/# viagra pfizer 25mg prezzo
tadacip tadalafil https://hoscillia.com/ lilly cialis coupons
cialis vs viagra reviews https://uhdcilise.com/ cialis daily
cialis 200 mg price https://hoscillia.com/ cialis versus viagra
pillole per erezione immediata viagra online spedizione gratuita viagra naturale
https://zithromax.pro/# zithromax for sale us
http://zithromax.pro/# zithromax 250 mg pill
https://clomidsale.pro/# can you buy generic clomid without a prescription
http://doxycyclinesale.pro/# how much is doxycycline in south africa
https://doxycyclinesale.pro/# doxycycline 3142
online canadian pharmacy: canada pharmacy online – canada drugstore pharmacy rx
canadian pharmacy cheap: canadian pharmacy meds – medication canadian pharmacy
mexico drug stores pharmacies: medication from mexico pharmacy – buying prescription drugs in mexico online
indian pharmacy: rx pharmacy india – indian pharmacy paypal
where can i buy cipro online: buy ciprofloxacin over the counter – ciprofloxacin over the counter
is seroquel a sleeping pill https://seroquelquetiapinedik.com/ quetiapine cost without insurance
duloxetine dosage maximum https://cymbaltaduloxetineztn.com/ duloxetine migraine
when to take prilosec morning or night https://prilosecomeprazoleuxe.com/ omeprazole and synthroid
buy antibiotics online: buy antibiotics online – antibiotic without presription
zoloft withdrawal symptoms brain zaps zoloft names can you buy sertraline over the counter
quit cymbalta cold turkey https://cymbaltaduloxetineztn.com/ can you take cymbalta and wellbutrin together
best time to take zoloft https://zoloftsertralineabu.com/ alternatives to sertraline
tramadol lexapro does escitalopram show up on a drug test lexapro and alcohol death
amlodipine desylate norvasc as an antihypertensive amlodipine besylate norvasc 10 mg
what is another name for amlodipine what drug category is norvasc classified as? norvasc pee more
escitalopram and ibuprofen https://lexaproescitalopramtns.com/ escitalopram 10 mg used for
Compared to TW01TREx BALF3 P1, a common reference, a clear increase of CNAs occurred in TW01TREx BALF3 DOX P15 and these were seen on chromosomes 1, 3, 4, 5, 6, 7, 8, 9, 11, 12, 15, 16, 18, 19, 22 and X; in contrast, relatively few CNAs were detected in TW01TREx VC DOX P15, TW01TREx BALF3 P15 and TW01TREx BALF3 DOX P1 Figure 3C cialis online
duloxetine gabapentin tylenol and cymbalta duloxetine dosage for depression
sertraline and hair loss zoloft interactions half life of zoloft
lexapro 20 mg reviews https://lexaproescitalopramtns.com/ lexapro and claritin
amlodipine benazepril 5/20 https://norvascamlodipinetce.com/ norvasc and lostartan
quetiapine used for sleep https://seroquelquetiapinedik.com/ quetiapine for?
can you get high off cymbalta cymbalta patient assisstance program cymbalta dizziness
omeprazole h pylori prilosec natural alternatives ranitidine or omeprazole
seroquel acne should bupropion aripiprazole and quetiapine be taken together quetiapine and alcohol
taking omeprazole at night omeprazole pill prilosec otc side effects
yeast infection treatment over the counter: over the counter ed medication – nystatin cream over the counter
duloxetine immediate release lyrica versus cymbalta cymbalta withdrawal side effects
quetiapine dementia https://seroquelquetiapinevuq.com/ seroquel and ativan
what amlodipine besylate used for norvasc and diabetes amlodipine besylate tablets
zoloft grapefruit doses of sertraline can sertraline cause anxiety
norvasc price comparison https://norvascamlodipineshe.com/ has norvasc been recalled
omeprazole 40 mg coupon what does prilosec treat side effects omeprazole long term use
is lexapro a tricyclic antidepressant lexapro success rate lexapro or prozac
stopping zoloft https://zoloftsertralineaco.com/ zoloft and anxiety
best over the counter toenail fungus treatment: over the counter medication – over the counter anti nausea
how long does duloxetine withdrawal last https://cymbaltaduloxetinesec.com/ alternatives to duloxetine
lexapro success tylenol and escitalopram difference between escitalopram and xanax
nifedipine and amlodipine norvasc scratchy throat norvasc 20 mg daily
zyprexa and seroquel seroquel dosage for major depressive disorder quetiapine fumarate alzheimer’s
escitalopram vs sertraline https://zoloftsertralineaco.com/ what is the generic name for zoloft
tradename for escitalopram lexapro when to take escitalopram 10 mg cost
flonase over the counter: best ed pills over the counter – over the counter medicine for anxiety and stress
how quickly does omeprazole work https://prilosecomeprazolezrv.com/ citalopram and omeprazole
54531 seroquel seroquel class of drug is seroquel a ssri
60mg duloxetine https://cymbaltaduloxetinestb.com/ wellbutrin and duloxetine together
prilosec otc dose https://prilosecomeprazolerls.com/ can omeprazole cause insomnia
over the counter flu medicine: over the counter drugs – uti treatment over the counter
quetiapine 300 mg street value seroquel and weight loss quetiapine fumarate 25mg tab
snorting zoloft can i lose weight while taking sertraline sertraline permanent side effects
cymbalta liver is cymbalta safe generic drug for cymbalta
sertraline and drinking https://zoloftsertralinedik.com/ advil and sertraline
prilosec class action lawsuit how to get off of prilosec omeprazole active ingredient
lexapro vs cymbalta https://lexaproescitalopramikd.com/ brand name escitalopram
norvasc description https://norvascamlodipinemry.com/ what is amlodipine besylate 2.5 mg.used for
best pill for ed ed treatment review best pills for ed
is norvasc ok if you have chf stage b amlodipine (norvasc) side effects amlodipine oral
lexapro and sleep problems escitalopram oxalate discount depression medicine escitalopram
duloxetine withdrawal timeline cymbalta and vicodin cymbalta vs trintellix
seroquel prices walmart can seroquel be abused quetiapine 50 mg twice daily
zoloft acid reflux https://zoloftsertralinedik.com/ can you take zoloft at night
norvasc and losartan combination amlodipine 2.5 mg tablet norvasc drug classification
discount pharmacies online canadian discount pharmacy reliable online pharmacy
valproic acid escitalopram https://lexaproescitalopramikd.com/ max dose lexapro
what are the side effects of quetiapine seroquel in elderly quetiapine sleeping pill
best non prescription ed pills non prescription ed drugs ed pills online
what is in cymbalta https://cymbaltaduloxetinestb.com/ does cymbalta help with anxiety
prevacid vs prilosec what is omeprazole used to treat prilosec iv
http://edpills.pro/# cheap ed pills
seroquel for opiate withdrawal crushing quetiapine tablets seroquel dosage for major depressive disorder
duloxetine rash https://cymbaltaduloxetinestb.com/ cymbalta side effects weight gain
omeprazole and kidney function omeprazole and breastfeeding omeprazole sa
difference between lexapro and effexor https://lexaproescitalopramikd.com/ wellbutrin vs escitalopram
is prozac a controlled substance fluoxetine 20 mg uses fluoxetine hcl 10mg for dogs
what is escitalopram used for escitalopram 40mg a day escitalopram narcotic
seroquel pills https://seroquelquetiapinesxz.com/ quetiapine xr 300 mg
fluoxetine and alcohol use https://prozacfluoxetinesyu.com/ prozac weight loss
duloxetine during pregnancy duloxetine mechanism of action what pain meds can you take with cymbalta
prilosec side effect how long does it take for prilosec to start working omeprazole metabolism
are citalopram and escitalopram the same https://lexaproescitalopramikd.com/ escitalopram get you high
top 10 online pharmacy in india indianpharmacy com world pharmacy india
how long does it take for prozac to leave your system what happens if you drink alcohol while taking fluoxetine tapering off prozac 10 mg
lexapro vs prozac weight gain https://prozacfluoxetineatb.com/ is fluoxetine safe for dogs
fluoxetine can’t sleep https://prozacfluoxetineatb.com/ ativan and fluoxetine
online pharmacy australia paypal: canadian online pharmacy no prescription – canada pharmacy
my canadian pharmacy – legitimate canadian mail order pharmacies online prescription drugs
best canadian pharmacies online international pharmacies that ship to the usa prescription pricing
cheap canadian cialis – drugs without a doctor s prescription best canadian online pharmacy reviews
canadian pharmacy generic prescription drugs without prior prescription drugstore online shopping
online pharmacy no prescription necessary – medicine from canada with no prescriptions my canadian drug store
canada drug prices drugs without a doctor s prescription canadian drugstore reviews
أكبر شركة لانتاج أنابيب البولي ايثيلين و يو بي سي ومستلزماتها للمنتجات الصناعية في عيراق
cialis dapoxetine europe buy Cialis 20mg price of cialis at walgreens
www canadianonlinepharmacy canada drug pharmacy canadian drugstore online
cialis 10mg ireland buy Cialis 20mg generic cialis soft tabs
discount cialis Cialis without a doctor prescription cialis online overnight delivery
أكبر شركة لانتاج أنابيب البولي ايثيلين و يو بي سي ومستلزماتها للمنتجات الصناعية في عيراق
أكبر شركة لانتاج أنابيب البولي ايثيلين و يو بي سي ومستلزماتها للمنتجات الصناعية في عيراق
best online to buy cialis Cialis without a doctor prescription cialis without persriction
the canadian pharmacy safe online pharmacies in canada legal to buy prescription drugs from canada
بعد قراءة مقالك ، ذكرني ببعض الأشياء التي درستها من قبل حول البوابة الإلكترونية. المحتوى مشابه لمحتوياتك ، لكن تفكيرك خاص جدًا ، وهو ما أعطاني فكرة مختلفة. شكرًا لك..
الأمانة العامة لمجلس الوزراء تدعو الى إعمام ضوابط تغيير العنوان الوظيفي. شكرًا لك..
п»їcytotec pills online where to get cytotec pills buy cytotec
world pharmacy india world pharmacy india indian pharmacy online
buying ed pills online erection pills online best ed medication
mail order pharmacy india top 10 online pharmacy in india online shopping pharmacy india
indianpharmacy com trusted online pharmacy reviews canadian pharmacy for viagra
reputable online pharmacy reddit canadian pharmacy without prescription cheapest pharmacy to get prescriptions filled
dapoxetine online USA dapoxetine online USA buy priligy
Oral Jelly 100mg Kamagra price Buy Kamagra online next day delivery Kamagra Oral Jelly 100mg buy online
priligy priligy over the counter Priligy 60 mg online
https://propecia.pro/# where can i get cheap propecia
Buy Dapoxetine [url=https://dapoxetine.pro/#]dapoxetine[/url] priligy over the counter
where buy propecia without rx finasteride over the counter can you get generic propecia tablets
payday loan
where to buy propecia no prescription buy propecia cost cheap propecia without dr prescription
Buy Kamagra online next day delivery Kamagra 100mg kamagra tablets usa
Priligy tablets priligy over the counter Priligy 60 mg online
propecia pill finasteride over the counter where to buy generic propecia online
Priligy tablets priligy dapoxetine
canadapharmacyonline com canadian pharmacy ordering drugs from canada
https://indiameds.pro/# top 10 pharmacies in india
purple pharmacy mexico price list medication from mexico pharmacy mexican drugstore online
http://canadapharmcertified.pro/# www canadianonlinepharmacy
canadian pharmacy india canadian drug prices my canadian pharmacy reviews
https://mexicanpharmacies.pro/# best online pharmacies in mexico
reputable indian pharmacies reputable indian pharmacies top 10 pharmacies in india
reputable indian online pharmacy mail order pharmacy india indianpharmacy com
https://indiameds.pro/# reputable indian pharmacies
cheapest online pharmacy india indian pharmacy paypal reputable indian pharmacies
https://mexicanpharmacies.pro/# mexico drug stores pharmacies
mexican drugstore online mexican online pharmacies prescription drugs mexican online pharmacies prescription drugs
sildenafil tablets 100mg price cheap sildenafil citrate sildenafil medicine
https://edpill.pro/# ed pills that really work
تخضع تجهيزات مصنع إيليت بايب Elite Pipeلعمليات مراقبة جودة صارمة للتأكد من أنها تلبي متطلبات الأداء والمتانة الأكثر صرامة.
http://fastpills.pro/# rx online
https://sildenafilpills.pro/# sildenafil medicine in india
https://edpill.pro/# drugs for ed
how to play aviator on sportybet aviator game tricks how to win aviator
can you take cephalexin on an empty stomach fish cephalexin for dogs is cephalexin used for ear infections
Elitepipe Plastic Factory’s HDPE fittings are renowned for their versatility, allowing for secure and efficient connections in diverse applications such as water supply, gas distribution, and industrial pipelines. Elitepipe Plastic Factory
keflex 500 mg for dogs https://keflexvex.com/ can i drink while taking keflex
cephalexin for throat infection can cephalexin be used for ear infection cephalexin fluoroquinolone
can you lay down after taking cephalexin cephalexin during pregnancy side effects how long is cephalexin good for
can i take my amoxicillin 4 hours early https://amoxicillinzuj.com/ amoxicillin-clavulanate potassium
keflex and sun exposure https://keflexvex.com/ do you have to eat with keflex
can i take zyrtec with amoxicillin what is in amoxicillin can a 12 year old take amoxicillin 500mg
cephalexin used for toothache missed cephalexin dose can i take acetaminophen with cephalexin
keflex interaction with alcohol is keflex good for a sinus infection keflex allergic
toddler won’t take amoxicillin amoxicillin after expiration date amoxicillin 400mg/5ml dosage for child ear infection
side effects of keflex in dogs https://keflexsfn.com/ does keflex make you tired
other names for keflex drinking on keflex keflex sirve para la garganta
can i take ibuprofen and cephalexin together https://cephalexinujx.com/ cephalexin 500mg for eye infection
amoxicillin for bv beer with amoxicillin will amoxicillin get rid of a uti
cephalexin 250 mg capsule for dogs cephalexin oral suspension for infants will cephalexin cure chlamydia
keflex dosage preseptal cellulitis https://keflexsfn.com/ can you take keflex for tooth infection
what’s amoxicillin amoxicillin for ear infection how many days does liquid amoxicillin go bad if not refrigerated
cephalexin and rocephin https://doxycyclineize.com/ cephalexin patient education
عندما يتعلق الأمر بأنابيب uPVC ، فإن مصنع إيليت بايب Elite Pipe يضع معايير عالية من خلال منتجاته المصممة بدقة والتي توفر حلول سباكة وري موثوقة وخالية من التسرب.
is expired ciprofloxacin safe ciprofloxacin side effects headache adverse effects of ciprofloxacin
azithromycin for cold https://azithromycintnu.com/ what is azithromycin used for?
1000 mg azithromycin for chlamydia https://azithromycintnu.com/ azithromycin not working
Hello there, simply was aware of your blog through Google, and found that it is really informative. I’m gonna watch out for brussels. I will appreciate when you continue this in future. A lot of folks shall be benefited from your writing. Cheers!
cephalexin for acne dosage how long does it take cephalexin to work what std does cephalexin treat
ciprofloxacin for otitis media can dogs take ciprofloxacin Щ…Ш§ Щ‡Щ€ ШЇЩ€Ш§ШЎ ciprofloxacin 500 mg
azithromycin drowsy https://azithromycinetj.com/ azithromycin tab
how to get azithromycin dose for chlamydia https://azithromycinetj.com/ gonorrhea azithromycin
can you take probiotics with ciprofloxacin can ciprofloxacin cure trichomoniasis ciprofloxacin sunlight side effects
ciprofloxacin for sinus infection ciprofloxacin and dexamethasone para que sirve ciprofloxacin and pink eye
cephalexin walmart https://doxycyclineize.com/ cephalexin monohydrate 250 mg
what is the brand name for azithromycin https://azithromycintnu.com/ azithromycin 500mg online
cephalexin 500mg for uti dosage do you have to eat with cephalexin what is cephalexin 500mg
sandoz ciprofloxacin https://ciprofloxacindik.com/ generic name of ciprofloxacin
doxycycline with azithromycin https://azithromycinetj.com/ azithromycin names
مع التركيز على التميز ، اكتسب مصنع إيليت بايب Elite Pipe سمعة طيبة في إنتاج منتجات HDPE و uPVC عالية الجودة التي تلبي معايير الجودة الصارمة.
is it safe to take prednisone https://prednisonesdc.com/ prednisone for coughing and wheezing
augmentin skin side effects cho tre uong thuoc augmentin augmentin duo forte 875 mg dosage
prednisone onset of action https://prednisonecyn.com/ can you take amoxicillin and prednisone together
prednisone pill images prednisone kidney stones prednisone safe for breastfeeding
augmentin pour les chats https://augmentinsbq.com/ augmentin diarrhea diaper rash
augmentin 500/ 125 mg augmentin a karmienie what is the name of the primary antibiotic in augmentin
prednisone treats https://prednisonesdc.com/ prednisone for pregnancy
augmentin es na co https://augmentinsbq.com/ antybiotyk augmentin dla noworodka
can you take aleve with prednisone https://prednisonecyn.com/ prednisone sleepy
can cephalexin treat ear infection in dogs https://cephalexinuop.com/ cephalexin allergy alternative
is azithromycin related to penicillin can you use azithromycin for tooth infection which auxiliary label should be applied to an azithromycin prescription during the filling process?
cephalexin 500mg dosage for uti cephalexin or amoxicillin what is cephalexin 500mg
can you put amoxicillin in milk amoxicillin-pot clavulanate 875-125 mg oral tablet does amoxicillin make you gain weight
The factory’s uPVC fittings are designed with meticulous attention to detail, ensuring secure and tight connections that minimize the risk of leaks or failures. Elitepipe Plastic Factory
what to mix amoxicillin with for toddler amoxicillin for covid what happens if you take amoxicillin without needing it
azithromycin 500 used for https://azithromycinikm.com/ azithromycin doses
prednisone and keflex keflex дёж–‡ keflex chronic sinus infection
what amoxicillin used for doxycycline amoxicillin can i cut amoxicillin in half
side effects of amoxicillin and clavulanate potassium can amoxicillin treat a uti can you take amoxicillin and drink alcohol
how may dosages keflex daily for uti breastfeeding keflex keflex and ear infection
keflex for gum infection allergic reaction to keflex will keflex treat impetigo?
cephalexin used for ear infection cephalexin and prednisone for dogs augmentin and cephalexin
amoxicillin muscle pain amoxicillin 500 para que sirve can you take amoxicillin and tylenol together
took azithromycin and still have symptoms https://azithromycinikm.com/ azithromycin 500 mg 3 tablets
what kind of antibiotic is keflex does keflex work for dog bites keflex dosing uti elderly
amoxicillin for tonsils https://amoxicillinxry.com/ is it safe to take amoxicillin
lunesta and augmentin can you have a glass of wine with augmentin epstein barr virus augmentin
azithromycin pseudomonas para que es azithromycin 500 mg azithromycin suspension dosage
cephalexin for cold and cough https://cephalexinuop.com/ cephalexin stomach pain
doxycycline cause anxiety can doxycycline treat tooth infection doxycycline heartburn
bebeklerde augmentin kullanД±mД± augmentin antibiotikum alkohol augmentin 875 strep throat
chlamydia treatment failure with doxycycline doxycycline with food threw up doxycycline
azithromycin vs penicillin allergy https://azithromycinikm.com/ azithromycin fridge
rash after prednisone treatment what is prednisone good for prednisone blood pressure
ciprofloxacin and clindamycin combination ciprofloxacin goodrx ciprofloxacin hydrochloride ophthalmic
ciprofloxacin uses for uti ciprofloxacin while breastfeeding cephalexin and ciprofloxacin
coming off prednisone side effects 5-day prednisone dosage prednisone hot flashes
augmentin is the same as amoxicillin аёЈаёІаё„аёІаёўаёІ augmentin 1 g augmentin 457/5ml prospect
cephalexin for toddlers cephalexin 500 mg capsule for dogs can you take amoxicillin with cephalexin
drinking while taking doxycycline how much is doxycycline without insurance at cvs azithromycin and doxycycline hyclate
does azithromycin treat kidney infection azithromycin without vet prescription fish azithromycin
is prednisone a strong steroid does prednisone affect muscle growth prednisone for migraine
ciprofloxacin for folliculitis ciprofloxacinжЇд»Ђд№€иЌЇ ciprofloxacin para que sirve
pills like cialis : bing mixed ed ed pills that really work
does cephalexin treat ear infections in dogs cephalexin poison ivy can you take cephalexin with food
augmentin pediatrico suspension 125 mg augmentin a jogurty drug interactions of augmentin
claritin and azithromycin https://azithromycinikm.com/ azithromycin 250 mg treatment
cephalexin same as keflex https://cephalexinuop.com/ cephalexin antibiotic side effects
augmentin antibiotico uso veterinario tonsillitis augmentin dose co to jest augmentin
azithromycin diarrhea treatment https://azithromycinikm.com/ azithromycin reddit
10mg prednisone prednisone covid risk prednisone while breastfeeding
Online poker
dog prednisone side effects prednisone and heart rate prednisone for viral infection
augmentin side effects dizzy augmentin a jogurty dose di augmentin
para que es cephalexin 500 mg https://cephalexinuop.com/ cephalexin std uses
prednisone pneumonia accidentally took prednisone at night is prednisone induced diabetes reversible
can cats take doxycycline doxycycline dosage for cats uri medication doxycycline
doxycycline mono 100 mg cap capsule doxycycline treat bv difference between doxycycline and doxycycline hyclate
ciprofloxacin vs amoxicillin bactrim vs ciprofloxacin ciprofloxacin for gram negative bacteremia
Elitepipe Plastic Factory’s commitment to customer satisfaction is evident in their prompt delivery schedules and exceptional after-sales service. Elitepipe Plastic Factory
Moderna says it will look at combining its original vaccine known as mRNA- 1273 with the newer version it created to fight the B buy cialis pills
ciprofloxacin prostatitis how long ciprofloxacin tiredness eye drops ciprofloxacin
the laughter of children playing in the park is a symphony of happiness pump in a new competition, google wants to crack machine unlearnin
Thanks. Quite a lot of forum posts.
essay writing website writing a college admission essay i need help writing an essay
can cephalexin be used for ear infection are cephalexin and amoxicillin the same cephalexin breastfeeding side effects baby
augmentin cistite gatto prescription for augmentin augmentin horror stories
allergic to penicillin can i take azithromycin https://azithromycinikm.com/ can you take azithromycin with amoxicillin
levitra lowest price All the studies contained groups that were comparable in age, although the criteria of reporting age varied
can cephalexin make you nauseous https://cephalexinuop.com/ antibiotic cephalexin alcohol
can doxycycline expire can you drink while taking doxycycline malaria prophylaxis doxycycline
augmentin e aerius augmentin for h pylori augmentin 875 infection urinaire
how long to give doxycycline for cats doxycycline with tylenol minocycline and doxycycline
how long does azithromycin take to work for acne azithromycin from mexico how long does azithromycin last before it expires
prednisone horniness prednisone for post nasal drip azithromycin and prednisone for covid
ciprofloxacin and oxycodone ciprofloxacin 0.3 eye drops for pink eye ciprofloxacin generic
is ciprofloxacin expensive does ciprofloxacin cause nausea ciprofloxacin instructions
switching from prednisone to methylprednisolone prednisone and benadryl can you drink with prednisone
augmentin sinusitis treatment augmentin every 8 hours augmentin libido
cephalexin fluoroquinolone https://cephalexinuop.com/ cephalexin and nicotine
doxycycline good for uti doxycycline pill identifier z pack vs doxycycline
will azithromycin treat a sinus infection can i eat dairy with azithromycin fish azithromycin for humans
prednisone addiction symptoms prednisone upset stomach prednisone weight loss side effect
ciprofloxacin al 500 ciprofloxacin teva side effects ciprofloxacin vs amoxicillin
does the antibiotic cephalexin affect birth control https://cephalexinuop.com/ what std does cephalexin treat
best probiotic augmentin augmentin in gravidanza primo trimestre what happens when augmentin is not refrigerated
can azithromycin treat sinus infection augmentin and azithromycin azithromycin contain penicillin
best natural viagra best place to buy viagra online 20 mg sildenafil
how long does cephalexin stay in your system after you finish it cephalexin folliculitis cephalexin bv
max daily dose of augmentin augmentin for otitis media dosage augmentin 875 mg 125 mg foglietto illustrativo
are you more subseptiable to getting anyeast infection from taking ciprofloxacin is ciprofloxacin a macrolide ciprofloxacin-dexamethasone cost
another name for azithromycin azithromycin dog what happens if azithromycin doesn’t work
ciprofloxacin keflex ciprofloxacin 0.3 eye drops ciprofloxacin canada
can prednisone give you diarrhea can u take prednisone at night can i take tylenol with prednisone
prednisone and covid treatment 2021 que es prednisone brand name for prednisone
www ciprofloxacin hcl ciprofloxacin 500 mg no prescription alternative to ciprofloxacin
can you take cephalexin for strep throat cephalexin dosage for dog bites will cephalexin treat a tooth infection
azithromycin 500 mg safe during pregnancy azithromycin toddler side effects can i take azithromycin for sinus infection
can you take prednisone while breastfeeding is prednisone safe prednisone headache relief
Why Deaths From Stroke Are Rising https://linkdirectory.at/detail/why-deaths-from-stroke-are-rising
Regards, Lots of forum posts.
best paper writing services essay writing meme essay writting service
The factory’s uPVC fittings are designed with meticulous attention to detail, ensuring secure and tight connections that minimize the risk of leaks or failures. Elitepipe Plastic Factory
تشتهر تجهيزات HDPE من إيليت بايب Elite Pipe بتعدد استخداماتها ، مما يسمح بوصلات آمنة وفعالة في تطبيقات متنوعة مثل إمدادات المياه وتوزيع الغاز وخطوط الأنابيب الصناعية.
إن تركيبات uPVC التي ينتجها مصنع إيليت بايب Elite Pipe مقاومة للغاية للتآكل ، وتوفر حلولاً موثوقة وخالية من الصيانة لأنظمة الري والسباكة.
Amazing lots of helpful data!
school administration resume writing service essay writing structure are essay writing services legal
Amazing quite a lot of terrific material!
r&d writing service writing a history essay essay writing service south africa
إن تركيبات uPVC التي ينتجها مصنع إيليت بايب Elite Pipe مقاومة للغاية للتآكل ، وتوفر حلولاً موثوقة وخالية من الصيانة لأنظمة الري والسباكة.
إن تركيبات uPVC التي ينتجها مصنع إيليت بايب Elite Pipe مقاومة للغاية للتآكل ، وتوفر حلولاً موثوقة وخالية من الصيانة لأنظمة الري والسباكة.
This is nicely expressed! .
college essay writing service the ladders resume writing service review thesis writing service reviews
Good facts. Thank you.
essay writing service malaysia essay writing service for nursing military service writing pdf
Nicely put, Regards!
best military to civilian resume writing service online college paper writing service college essay writing service near me
Wow quite a lot of great tips.
guest blog writing service college admission essay writing service bartleby writing customer service number
You expressed it well.
custom essay writing online will writing service reviews writing a cleaning service proposal
You made your position pretty effectively..
4th grade essay writing worksheets essay writer help research paper writing services
Fantastic postings. Kudos!
best nursing paper writing service writing as a service essay writing service price
Really quite a lot of very good info.
education essay writing service oxford essay writing service best cv writing service uk 2019
Whoa lots of very good tips!
reliable essay writing service top cv writing service uk coursework writing service review
Incredible a lot of great material!
best college essay writing service professional resume writing service charlotte nc urgent essay writing service
Awesome advice. With thanks!
essay writing service cheating essay writting service writing an essay in apa format
Incredible all kinds of superb tips!
who has the best essay writing service essay writing service cost writing help essay service
cialis forum discussion tadalafilise.cyou/#
viagra and levitra taken together tadalafilise.cyou/#
cialis generic over the counter best way to take tadalafil cialis online canada
Appreciate it, A good amount of info!
buy essay service [url=https://theessayswriters.com/]i can t write my essay[/url] help me write a thesis statement for free [url=https://bestcheapessaywriters.com/]first essay writer[/url] do my essay for me for free custom article writing service [url=https://helpwithdissertationwriting.com/]writing help[/url] buy phd research proposal [url=https://dissertationwritingtops.com/]dissertation editing[/url] dissertation helper
Truly quite a lot of terrific knowledge.
best resume writing service in usa [url=https://theessayswriters.com/]essay writer no plagiarism[/url] do my uni essay for me [url=https://bestcheapessaywriters.com/]write my essay com[/url] do my essay uk thesis writing service reviews [url=https://writinganessaycollegeservice.com/]solicitor will writing service[/url] best uk essay writing service reviews [url=https://essayservicehelp.com/]write essay service[/url] lab report writing service uk
Very well voiced truly! .
cv writing service cork [url=https://customthesiswritingservice.com/]thesis paper[/url] thesis about local study food and beverage service national assessment [url=https://writingthesistops.com/]a good thesis statement[/url] career research paper thesis statement cheap reliable essay writing service [url=https://essayssolution.com/]write a cover letter for me[/url] essay writers online [url=https://cheapessaywriteronlineservices.com/]i am a writer essay sample[/url] write my narrative essay
is prednisone for pain supplements to help with prednisone withdrawal prednisone and headaches
Nicely put. Appreciate it!
paper writer services [url=https://dissertationwritingtops.com/]english dissertation help[/url] data analysis in dissertation [url=https://helpwritingdissertation.com/]chicago illinois dissertation help[/url] help writing literature review dissertation will writing service gravesend [url=https://essaytyperhelp.com/]college essay help near me[/url] essay help uk [url=https://helptowriteanessay.com/]personal essay helper[/url] help with writing an essay
prednisone for covid 2022 does your body go back to normal after prednisone? prednisone horniness
Incredible tons of very good material.
reputable essay writing services [url=https://essayssolution.com/]can you write a story for me[/url] how to write an about me for dating [url=https://cheapessaywriteronlineservices.com/]can you do my essay[/url] can you write a letter for me best university essay writing service [url=https://writinganessaycollegeservice.com/]best essay writing service yahoo answers[/url] essay writing service caught [url=https://essayservicehelp.com/]essay help service[/url] assignment writing service in london
Cheers. I appreciate this.
will writing service [url=https://theessayswriters.com/]personal essay writer[/url] write my essay paper [url=https://bestcheapessaywriters.com/]write an essay for me[/url] write my essay for money custom essay service [url=https://payforanessaysonline.com/]essay writing order[/url] order cheap essay online [url=https://buycheapessaysonline.com/]order admission essay[/url] custom essay order
where can you get viagra 200mg sildenafil soft gel capsule cheap viagra 25mg
buy female viagra pills sildenafil 100mg price canada otc viagra for women
sildenafil india pharmacy viagra 2018 how do i get viagra
generic viagra for sale in usa generic viagra sildenafil 100mg buy generic viagra online europe
sildenafil prescription medicine sildenafil pharmacy purchase female viagra online
canada prescription viagra where can i buy sildenafil 20mg where can you buy viagra over the counter in australia
sildenafil 50mg prices sildenafil price how to buy viagra in usa
canadian pharmacy viagra 100 mg generic viagra lowest prices cheap canadian pharmacy viagra
best viagra pills buy sildenafil usa sildenafil 100mg prescription
200 mg viagra for sale buy generic viagra from canada online how much is over the counter viagra
buy sildenafil online australia discount generic viagra india viagra 30 pills
cheap viagra online in usa sildenafil 20 mg coupon generic viagra for daily use
plant viagra natural viagra recipe chinese herb viagra
online mexican pharmacy oxycodone mutual of omaha rx pharmacy australian online pharmacy viagra
reputable online pharmacy uk metronidazole singapore pharmacy top rated online pharmacy
giant grocery store pharmacy what pharmacy sells viagra best online pharmacy that does not require a prescription
asda pharmacy ventolin inhaler online pharmacy promethazine codeine syrup best online international pharmacies
Depakote reputable online pharmacy tramadol boots pharmacy cetirizine
wegmans pharmacy free lipitor online pharmacy viagra fluconazole uk pharmacy
buy tadalafil cheap online tadalafil online no prescription tadalafil prescribing information
buy viagra online no script sildenafil 20 mg without a prescription viagra medication
20mg tadalafil cialis uk supplier cialis half life
flomax and cialis generic cialis usa mambo 36 tadalafil
cialis paypall cheapest tadalafil tablets cialis 20 mg, best price
cephalexin for dogs side effects peeing are there any side effects with keflex and levothyroxine what is cephalexin most commonly used for?
bactrim and keflex for mrsa cephalexin for pink eye whats cephalexin used for
cephalexin and gabapentin keflex can you drink alcohol cephalexin over the counter
can you take advil with cephalexin cephalexin interaction with alcohol which is better keflex vs amoxicillin for burn infection
how long does cephalexin stay in your system para que sirve la cephalexin is it safe to take imodium for diarrhea caused by keflex
amoxicillin дёж–‡ is azithromycin the same as amoxicillin icd 10 code for allergy to amoxicillin
what happens if amoxicillin is not refrigerated how does amoxicillin kill bacteria is amoxicillin safe for dogs
amoxicillin for dry cough can i take melatonin with amoxicillin amoxicillin for ear infection in adults
augmentin+metronidazole combination does augmentin affect nuvaring lieu dung augmentin 625mg
iv augmentin in children augmentin inj 1.2g augmentin helyettesГtГ©se
amoxicillin for sinusitis amoxicillin std shelf life amoxicillin
ciprofloxacin pancreatitis prednisone and ciprofloxacin is ciprofloxacin good for throat infection
what vitamins should not be taken with prednisone can i drink alcohol on prednisone why take prednisone in the morning
how long does it take for ciprofloxacin to work ciprofloxacin ophthalmic solution for eyes ofloxacin vs ciprofloxacin
buy doxycycline amazon doxycycline how long to work doxycycline for fish
cefdinir vs doxycycline do you take doxycycline with food how to mix doxycycline for cats
prednisone tablets prednisone withdrawal after 5 days prednisone 5 mg para que sirve
does cephalexin treat impetigo if allergic to amoxicillin can you take cephalexin cephalexin generation
can i buy azithromycin online how long does azithromycin take to work for acne azithromycin black box warning
buy viagra 100mg cheap viagra 100mg canada viagra online canadian pharmacy paypal
cost of viagra in mexico viagra 88 buy generic viagra uk
cialis australia cialis effectiveness buy tadalafil cheap
5mg tadalafil online generic buy cialis cialis effective time
cialis everyday cialis australia online shopping tadalafil 5 mg tablet
viagra 150 mg price in india best place buy viagra online can i buy viagra in usa
cheap viagra online how to purchase viagra tablet price of viagra in australia
essay bot help with essay writing custom essay writing cheap
synthesis essay examples can i pay someone to write my essay mla style essay
globlization essay write an essay about yourself best argumentative essay topics
buy essay writing definition essay topics essay by line crossword
essay on literature someone write my essay for me proper heading for essay
why marijuanas should be legal essay conclusion examples essay college essay helper
good essay writers famous essay writers this i believe essay examples
conclusion essay help writing a compare and contrast essay sample essay outline
capsule online pharmacy clotrimazole price pharmacy tylenol 1 pharmacy
online pharmacy search prescription cost amlodipine pharmacy prices
guardian pharmacy singapore viagra giant eagle pharmacy hours pharmacy atenolol
rx express pharmacy stockton ca mexico pharmacy accutane kroger pharmacy simvastatin
giant eagle pharmacy pharmacy logo rx Viagra Professional
valium internet pharmacy buy hydrocodone online pharmacy pharmacy bangkok kamagra
rx pharmacy cialis north drug store des moines pharmacy hydrocodone
tadalafil and hypertension tadalafil how long does it take to work tadalafil 60 mg reviews
20 mg tadalafil effects which is stronger sildenafil or tadalafil tadalafil raise blood pressure
tadalafil how long to take effect genpharma tadalafil tadalafil copay card
combining tadalafil and sildenafil tadalafil alzheimer how long does tadalafil stay in your system
tadalafil dose for ed tadalafil fj2 20 mg tadalafil tablet
tadalafil sandoz tadalafil 5mg goodrx tadalafil bodybuilding dosage
tadalafil resistance tadalafil 20 mg precio how much tadalafil is too much
how long before tadalafil works tadalafil (cialis) half life tadalafil
chrisale tadalafil 20 mg sildenafil vs tadalafil which is better will tadalafil make you hard
difference tadalafil sildenafil generic viagra tadalafil can i take tadalafil daily
tadalafil uk mixing sildenafil and tadalafil dose of tadalafil
Fulcrum.fountainhead.cash – https://wiki.electroncash.de/wiki/Fulcrum.fountainhead.cash
is tadalafil stronger than sildenafil dr. reddys tadalafil teva, tadalafil, purchase
tadalafil reaction time tadalafil nebenwirkungen can you overdose on tadalafil
tadalafil generic cialis get tadalafil prescription online tadalafil peak
tadalafil pulmonary hypertension tadalafil and tamsulosin interaction daily tadalafil pe
what if tadalafil doesn’t work is tadalafil same as viagra tadalafil manipulado
tadalafil mylan how long does 10mg tadalafil last 20mg of tadalafil
tadalafil vidalista 80 mg best time to take tadalafil 20 mg tadalafil vs sildenafil bluechew
We all have dreams and aspirations that seem daunting at first glance. Whether it’s launching a successful business, 10x’ing your income, inventing a life saving or life changing device, or mastering a new skill, big goals can often feel overwhelming.
However, I firmly believe that with the right system, you can turn these dreams into reality.
Systems are what makes the difference on the ability to repeat something that has been proven to work.
Every successful franchise in the world is so successful because they have repeatable systems that save time, money effort and have been proven time after time to work for every one that uses them.
Learn a system for achieving the biggest goals used by the uber successful and now available to you.
Check out this free video and get access to a FREE preview of this system before it is taken down.
Just copy and paste this link in your browser https://youtu.be/kcdIPGeyuEA
Hello there! Do you know if they make any plugins to protect against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on. Any tips?
KNA reports no disclosures AJS serves as a consultant to Alder, Amgen, eNeura, Eli Lilly Company, Impel, Lundbeck, Medscape, and Novartis and receives research funding from the Migraine Research Foundation and Mayo Clinic Intramural Funding over the counter female viagra Previous clinical and anecdotal evidence suggest that the immediate post treatment phase is characterized by disruption, transition and increased stress which improves over time 52
Моментально возводимые здания: финансовая польза в каждой части!
В сегодняшнем обществе, где секунды – доллары, скоростройки стали решением, спасающим для коммерческой деятельности. Эти инновационные конструкции обладают высокую прочность, экономическую эффективность и ускоренную установку, что делает их первоклассным вариантом для разнообразных предпринимательских инициатив.
[url=https://bystrovozvodimye-zdanija-moskva.ru/]Строительство быстровозводимых зданий цена[/url]
1. Высокая скорость возвода: Секунды – самое ценное в деловой сфере, и сооружения моментального монтажа способствуют значительному сокращению сроков возведения. Это высоко оценивается в условиях, когда актуально оперативно начать предпринимательство и начать монетизацию.
2. Экономия: За счет улучшения производственных процедур элементов и сборки на объекте, затраты на экспресс-конструкции часто бывает ниже, по сопоставлению с традиционными строительными задачами. Это способствует сбережению денежных ресурсов и получить более высокую рентабельность инвестиций.
Подробнее на [url=https://bystrovozvodimye-zdanija-moskva.ru/]https://www.scholding.ru[/url]
В заключение, моментальные сооружения – это первоклассное решение для бизнес-проектов. Они объединяют в себе молниеносную установку, финансовую эффективность и надежность, что позволяет им первоклассным вариантом для компаний, готовых к мгновенному началу бизнеса и получать прибыль. Не упустите момент экономии времени и средств, оптимальные моментальные сооружения для вашей будущей задачи!
cvs store & pharmacy orange, tx cyprus online pharmacy dangerous prescription drugs
Скорозагружаемые здания: финансовая польза в каждой части!
В современной сфере, где секунды – доллары, скоростройки стали настоящим спасением для фирм. Эти современные конструкции включают в себя устойчивость, финансовую экономию и молниеносную установку, что делает их превосходным выбором для коммерческих мероприятий.
[url=https://bystrovozvodimye-zdanija-moskva.ru/]Строительство быстровозводимых зданий из металлоконструкций цена[/url]
1. Молниеносное строительство: Минуты – основной фактор в предпринимательстве, и быстровозводимые здания позволяют существенно уменьшить временные рамки строительства. Это преимущественно важно в случаях, когда срочно нужно начать бизнес и начать зарабатывать.
2. Финансовая эффективность: За счет улучшения процессов изготовления элементов и сборки на объекте, стоимость быстровозводимых зданий часто бывает ниже, по сопоставлению с обыденными строительными проектами. Это позволяет сократить затраты и обеспечить более высокий доход с инвестиций.
Подробнее на [url=https://bystrovozvodimye-zdanija-moskva.ru/]scholding.ru[/url]
В заключение, скоростроительные сооружения – это оптимальное решение для бизнес-мероприятий. Они сочетают в себе быстроту возведения, экономическую эффективность и твердость, что обуславливает их лучшим выбором для предприятий, активно нацеленных на скорый старт бизнеса и извлекать прибыль. Не упустите возможность получить выгоду в виде сэкономленного времени и денег, наилучшие объекты быстрого возвода для вашего предстоящего предприятия!
Быстромонтажные здания: бизнес-польза в каждом кирпиче!
В современном обществе, где часы – финансовые ресурсы, экспресс-конструкции стали истинным спасением для коммерческой деятельности. Эти современные конструкции включают в себя повышенную прочность, финансовую выгоду и молниеносную установку, что дает им возможность идеальным выбором для различных коммерческих проектов.
[url=https://bystrovozvodimye-zdanija-moskva.ru/]Быстровозводимые здания[/url]
1. Скорость строительства: Моменты – наиважнейший аспект в деловой сфере, и объекты быстрого монтажа обеспечивают значительное снижение времени строительства. Это особенно ценно в вариантах, когда актуально оперативно начать предпринимательство и получать доход.
2. Экономичность: За счет совершенствования производственных операций по изготовлению элементов и монтажу на площадке, финансовые издержки на быстровозводимые объекты часто приходит вниз, по сопоставлению с обыденными строительными проектами. Это позволяет сократить затраты и добиться более высокой доходности инвестиций.
Подробнее на [url=https://bystrovozvodimye-zdanija-moskva.ru/]https://www.scholding.ru/[/url]
В заключение, моментальные сооружения – это превосходное решение для коммерческих задач. Они комбинируют в себе ускоренную установку, бюджетность и твердость, что делает их идеальным выбором для фирм, готовых начать прибыльное дело и обеспечивать доход. Не упустите возможность сократить издержки и сэкономить время, выбрав быстровозводимые здания для вашей будущей задачи!
robert frost fire and ice essay https://manuellhzqi.blogdeazar.com/23744291/facts-about-buy-essays-online-dsd-revealed csu essay prompts 2014
ラブドール リアル 人形市場で素晴らしい全身のセックス人形を見つけるには、セックス人形の利用について考えるべき4つのヒントミニセックス人形の配置110cmシリコンセックス人形日本のセックス人形の新進気鋭の時代は何ですか?
We wish to thank you again for the stunning ideas you offered Jesse when preparing her own post-graduate
research and, most importantly, pertaining to providing all of
the ideas in a single blog post. In case we had been aware of your web page a
year ago, we’d have been rescued from the pointless measures we were participating in. Thank you very much.
sex shop
san antonio cialis doctor
cialis dosage reddit
viagra offshore pharmacy
methotrexate pharmacy mistake
buy female viagra pills in india online
can you buy viagra over the counter uk
cialis black without prescription
cialis daily vs 36 hour
flomax pharmacy training
cheap viagra 50mg
Наша бригада искусных исполнителей завершена предлагать вам инновационные средства, которые не только гарантируют устойчивую протекцию от холодных воздействий, но и дарят вашему коттеджу модный вид.
Мы эксплуатируем с новейшими средствами, заверяя постоянный срок службы и прекрасные результаты. Изолирование внешней обшивки – это не только экономия на обогреве, но и трепет о природной среде. Спасательные подходы, какие мы осуществляем, способствуют не только личному, но и поддержанию природных богатств.
Самое основополагающее: [url=https://ppu-prof.ru/]Сколько стоит сделать утепление фасада[/url] у нас стартует всего от 1250 рублей за м²! Это доступное решение, которое превратит ваш хаус в истинный тепличный локал с минимальными затратами.
Наши пособия – это не всего лишь изоляция, это разработка поля, в где всякий элемент преломляет ваш особенный моду. Мы возьмем во внимание все твои потребности, чтобы сделать ваш дом еще еще больше дружелюбным и привлекательным.
Подробнее на [url=https://ppu-prof.ru/]www.ppu-prof.ru[/url]
Не откладывайте дела о своем обители на потом! Обращайтесь к специалистам, и мы сделаем ваш дом не только уютнее, но и по последней моде. Заинтересовались? Подробнее о наших работах вы можете узнать на портале. Добро пожаловать в пределы гармонии и качественного исполнения.
SightCare supports overall eye health, enhances vision, and protects against oxidative stress. Take control of your eye health and enjoy the benefits of clear and vibrant eyesight with Sight Care. https://sightcarebuynow.us/
cialis max dose
Aizen Power is an all-natural supplement designed to improve male health. This formula contains the beneficial properties of various plants, herbs, minerals, and vitamins that help men’s blood circulation, detoxification, and overall health. https://aizenpowerbuynow.us/
Abdomax is a nutritional supplement using an 8-second Nordic cleanse to eliminate gut issues, support gut health, and optimize pepsinogen levels. https://abdomaxbuynow.us/
Cortexi is a completely natural product that promotes healthy hearing, improves memory, and sharpens mental clarity. Cortexi hearing support formula is a combination of high-quality natural components that work together to offer you with a variety of health advantages, particularly for persons in their middle and late years. Cortexi not only improves hearing but also decreases inflammation, eliminates brain fog, and gives natural memory protection. https://cortexibuynow.us/
buy cialis online usa
Folixine is a enhancement that regrows hair from the follicles by nourishing the scalp. It helps in strengthening hairs from roots. https://folixinebuynow.us/
EyeFortin is an all-natural eye-health supplement that helps to keep your eyes healthy even as you age. It prevents infections and detoxifies your eyes while also being stimulant-free. This makes it a great choice for those who are looking for a natural way to improve their eye health. https://eyefortinbuynow.us/
Dentitox Pro is a liquid dietary solution created as a serum to support healthy gums and teeth. Dentitox Pro formula is made in the best natural way with unique, powerful botanical ingredients that can support healthy teeth. https://dentitoxbuynow.us/
Digestyl™ is natural, potent and effective mixture, in the form of a powerful pill that would detoxify the gut and rejuvenate the whole organism in order to properly digest and get rid of the Clostridium Perfringens. https://digestylbuynow.us/
GlucoTrust is a revolutionary blood sugar support solution that eliminates the underlying causes of type 2 diabetes and associated health risks. https://glucotrustbuynow.us/
Gut Vita™ is a daily supplement that helps consumers to improve the balance in their gut microbiome, which supports the health of their immune system. It supports healthy digestion, even for consumers who have maintained an unhealthy diet for a long time. https://gutvitabuynow.us/
GlucoFlush is an advanced formula specially designed for pancreas support that will let you promote healthy weight by effectively maintaining the blood sugar level and cleansing and strengthening your gut. https://glucoflushbuynow.us/
Glucofort Blood Sugar Support is an all-natural dietary formula that works to support healthy blood sugar levels. It also supports glucose metabolism. According to the manufacturer, this supplement can help users keep their blood sugar levels healthy and within a normal range with herbs, vitamins, plant extracts, and other natural ingredients. https://glucofortbuynow.us/
Gorilla Flow prostate is an all-natural dietary supplement for men which aims to decrease inflammation in the prostate to decrease common urinary tract issues such as frequent and night-time urination, leakage, or blocked urine stream. https://gorillaflowbuynow.us/
LeanBliss is a unique weight loss formula that promotes optimal weight and balanced blood sugar levels while curbing your appetite, detoxifying, and boosting your metabolism. https://leanblissbuynow.us/
Java Burn is a proprietary blend of metabolism-boosting ingredients that work together to promote weight loss in your body. https://javaburnbuynow.us/
Illuderma is a serum designed to deeply nourish, clear, and hydrate the skin. The goal of this solution began with dark spots, which were previously thought to be a natural symptom of ageing. The creators of Illuderma were certain that blue modern radiation is the source of dark spots after conducting extensive research. https://illudermabuynow.us/
Keratone addresses the real root cause of your toenail fungus in an extremely safe and natural way and nourishes your nails and skin so you can stay protected against infectious related diseases. https://keratonebuynow.us/
GlucoCare is a natural and safe supplement for blood sugar support and weight management. It fixes your metabolism and detoxifies your body. https://glucocarebuynow.us/
LeanFlux is a revolutionary dietary formula specially crafted for individuals dealing with obesity and those on a weight loss journey. https://leanfluxbuynow.us/
tadalafil headache cure
cialis generico
discount viagra from india
I appreciate, cause I found exactly what I was taking a look for.
You have ended my four day lengthy hunt! God Bless you man. Have a great day.
Bye
sildenafil buy without prescription
tadalafil liquid
cialis 20 mg duration
cialis dapoxetine
bactrim cystitis
flagyl blogspot
How do delete wikipedia’s featured article that contains copyright violation?
Wow, wonderful blog layout! How long have you ever been blogging for?
you made blogging glance easy. The total look of
your site is excellent, as well as the content material!
You can see similar: https://vortexara.top and here Vortexara.top
Hi, I do believe this is an excellent website. I stumbledupon it 😉 I
may revisit yet again since i have book-marked it.
Money and freedom is the greatest way to change, may you be rich and continue to help other people.
I saw similar here: ecommerce and also here: dobry
sklep
Greetings! Very useful advice in this particular article!
It’s the little changes that make the greatest changes. Many thanks for sharing!
I saw similar here: e-commerce and also here: e-commerce
zithromax dosing
My partner and I stumbled over here by a different page and thought I might as well check things out.
I like what I see so now i’m following you.
Look forward to looking into your web page repeatedly.
I saw similar here: najlepszy sklep and also here: e-commerce
cialis pharmacy rx one Canada Pharmacy
cialis in usa pharmacy [url=http://canadianphrmacy23.com/]canadianphrmacy23.com[/url]
how does metformin work for weight loss
Wow, superb weblog structure! How long have you
ever been running a blog for? you make running a blog look easy.
The overall glance of your web site is fantastic, as well as the content material!
You can see similar: sklep online and here sklep
can you take diflucan and flagyl together
does zoloft work
lisinopril hctz 10 12.5
furosemide 40 mg picture
is gabapentin a benzodiazepine
universal pharmacy canada pharmacy
best online pharmacies [url=http://canadianphrmacy23.com/]india pharmacy[/url]
what is amoxicillin good for
escitalopram drowsiness
It’s very interesting! If you need help, look here: hitman agency
ciprofloxacin dairy
bactrim ds vs bactrim
will cephalexin treat sinus infection
Hi there, the whole thing is going sound here and ofcourse
every one is sharing information, that’s actually good, keep up writing.
I saw similar here: dobry sklep and also here: najlepszy sklep
how long for amoxicillin to work
shelf life of cephalexin
whats bactrim used for
citalopram to escitalopram
how much gabapentin can i give my dog
Наша группа квалифицированных исполнителей подготовлена выдвинуть вам актуальные системы утепления, которые не только снабдят надежную безопасность от прохлады, но и дарят вашему жилью современный вид.
Мы занимаемся с последними материалами, утверждая постоянный термин использования и выдающиеся эффекты. Теплоизоляция внешней обшивки – это не только сокращение расходов на отоплении, но и заботливость о экологической обстановке. Энергоэффективные методы, какие мы производим, способствуют не только своему, но и сохранению природных богатств.
Самое ключевое: [url=https://ppu-prof.ru/]Утепление фасада цена за 1 м2 москва[/url] у нас стартует всего от 1250 рублей за квадратный метр! Это бюджетное решение, которое превратит ваш домик в реальный комфортный уголок с минимальными затратами.
Наши пособия – это не лишь изолирование, это постройка пространства, в где каждый элемент символизирует ваш собственный стиль. Мы примем все твои требования, чтобы осуществить ваш дом еще еще более теплым и привлекательным.
Подробнее на [url=https://ppu-prof.ru/]https://ppu-prof.ru/[/url]
Не откладывайте труды о своем ларце на потом! Обращайтесь к квалифицированным работникам, и мы сделаем ваш корпус не только тепличным, но и изысканнее. Заинтересовались? Подробнее о наших трудах вы можете узнать на официальном сайте. Добро пожаловать в обитель благополучия и стандартов.
generic for depakote
Наша бригада профессиональных мастеров готова выдвинуть вам передовые технологии, которые не только гарантируют надежную защиту от холодильности, но и дарят вашему собственности оригинальный вид.
Мы функционируем с самыми современными веществами, заверяя долгий запас работы и блестящие эффекты. Изоляция облицовки – это не только экономия на прогреве, но и забота о экологической обстановке. Сберегательные разработки, какие мы внедряем, способствуют не только дому, но и сохранению природных ресурсов.
Самое главное: [url=https://ppu-prof.ru/]Утепление фасада цена за 1 м2 москва[/url] у нас стартует всего от 1250 рублей за м2! Это бюджетное решение, которое превратит ваш домик в истинный уютный корнер с минимальными затратами.
Наши примеры – это не только утепление, это постройка площади, в где всякий аспект преломляет ваш личный образ действия. Мы рассмотрим все ваши потребности, чтобы осуществить ваш дом еще еще более дружелюбным и привлекательным.
Подробнее на [url=https://ppu-prof.ru/]www.ppu-prof.ru[/url]
Не откладывайте заботу о своем квартире на потом! Обращайтесь к специалистам, и мы сделаем ваш помещение не только более теплым, но и стильным. Заинтересовались? Подробнее о наших работах вы можете узнать на портале. Добро пожаловать в пространство спокойствия и уровня.
citalopram and diphenhydramine
I know this if off topic but I’m looking into starting my own weblog and was curious what all is required to get set up?
I’m assuming having a blog like yours would cost a pretty penny?
I’m not very internet savvy so I’m not 100% certain. Any suggestions or advice would be greatly appreciated.
Thank you
ddavp iv half life
depakote loading dose
citalopram 40 mg high
c diltiazem
augmentin side effects
diclofenac pain killer
contrave 25 off
flomax lightheadedness
great article
buy flexeril online
It’s wonderful that you are getting thoughts from this
paragraph as well as from our argument made here.
I saw similar here: Dobry sklep
low dose aspirin during pregnancy
aripiprazole tablets side effects
I appreciate you sharing this blog article.Really thank you!
allopurinol vs.uloric
what is in augmentin
naltrexone and bupropion
baclofen and naproxen
celebrex for rheumatoid arthritis
celexa lawsuit
buspar sexual side effects
What’s up to every one, the contents existing at this web page are
genuinely awesome for people knowledge, well, keep up the nice work
fellows.
ashwagandha high
que es celecoxib
Наша бригада опытных специалистов предоставлена предложить вам инновационные системы утепления, которые не только снабдят надежную оборону от заморозков, но и подарят вашему собственности современный вид.
Мы эксплуатируем с современными материалами, подтверждая прочный срок эксплуатации и выдающиеся результирующие показатели. Изоляция фронтонов – это не только экономия ресурсов на огреве, но и забота о природной среде. Сберегательные разработки, какие мы применяем, способствуют не только зданию, но и сохранению природы.
Самое ключевое: [url=https://ppu-prof.ru/]Цена м2 утепление фасада дома[/url] у нас составляет всего от 1250 рублей за кв. м.! Это доступное решение, которое сделает ваш домик в истинный уютный локал с минимальными затратами.
Наши труды – это не единственно изолирование, это постройка площади, в где все член отражает ваш личный модель. Мы берем во внимание все все ваши желания, чтобы воплотить ваш дом еще еще больше дружелюбным и привлекательным.
Подробнее на [url=https://ppu-prof.ru/]https://www.ppu-prof.ru[/url]
Не откладывайте заботу о своем корпусе на потом! Обращайтесь к экспертам, и мы сделаем ваш помещение не только теплым, но и стильным. Заинтересовались? Подробнее о наших проектах вы можете узнать на веб-сайте. Добро пожаловать в сферу благополучия и качественной работы.
acarbose ems
can you take abilify while pregnant
semaglutide brand name
actos ring
Hey There. I found your blog using msn. This is a really well written article.
I’ll be sure to bookmark it and return to read more of your useful
info. Thanks for the post. I’ll certainly comeback.
how does protonix work
repaglinide brand names
buy robaxin online
does remeron cause weight gain