What is the function of the placenta? How does the placenta work? What happens to the placenta after birth? These should be important questions for any future mother if she wants to have complete control over her pregnancy.
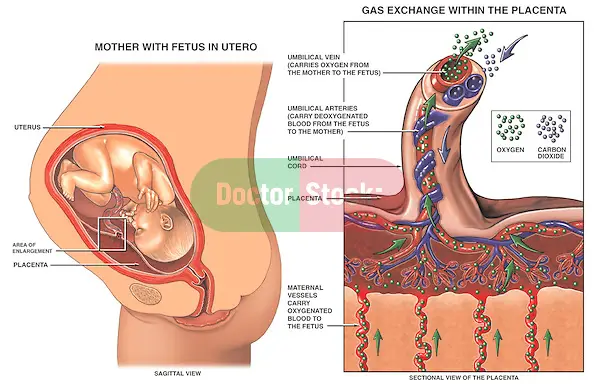
Table of Contents
What Is a Placenta and What Does It Do?
The placenta is a temporary organ which develops in the uterus and helps the baby receiving all the necessary nutrients to develop during the 40 weeks of pregnancy. At 12 weeks of pregnancy, the placenta is completely formed. The placenta has the shape of a disc at delivery, measures around 18 to 20 cm in diameter and only a little over 5 cm in thickness. Its upper part is completely smooth and the hip which adheres to the wall of the uterus is rough. The placenta is richly vascularized. The umbilical cord is the one connecting the placenta to the baby.
Progesterone, estrogen and hCG are produced by the placenta. The placenta is the organ responsible for functioning as a trading post between blood supply of the mother and baby. There are tiny blood vessels that carry fetal blood through this organ, which is already full of maternal blood. Oxygen and nutrients from the blood of the mother are transferred to the baby`s blood, while in turn waste products are transferred from baby`s blood to the maternal blood, without the 2 blood supplies ever mixing. – Read more!
The placental membrane divides the 2 circulations:
- The maternal placental circulation which runs from the basal plate.
- The villous fetal circulation which runs in a capillary system with an arterial path and a venous one.
The placenta is removed from the mother`s uterus in a process known as the after-birth process. A potential issue during pregnancy is placenta praevia, when the placenta gets attached over the cervix. As the baby develops, bleeding may occur due to the pressure caused on the placenta. This medical condition needs medical assistance to make sure labor and delivery run safely for both the mother and baby.
Transporting Function of the Placenta
Transfer of Some Important Elements
- Oxygen – The transfer of the oxygen is made through the mechanism of simple diffusion. The consumption of oxygen of the uterus and its content at term is of around 20ml/min. from which 2/3 transferred to the fetus.
The fetus has a great ability of maintaining the consumption of oxygen. The fetal hemoglobin presents an affinity for oxygen, and if the umbilical flow is reduced, the fetus has an increased ability of extracting the oxygen. In case that the released of the oxygen towards the fetus is reduced, the most part from the umbilical venous blood is diverted towards myocardium and the upper side of the heart. The secretion of catecholamines will increase simultaneously along with the achievement of vasoconstriction.
- Carbon Dioxide – At the placental membrane`s level, the permeability to carbon dioxide is increased.
- Water – The water flow at the placental level is influenced by the osmotic and hydrostatic force as well as the electrolyte gradient, the fetus drinking a large quantity of water on a daily basis.
- Glucose – The main energy substrate for the fetus is formed from maternal glucose. The normal transfer of this nutrient is an essential condition for the normal development of the fetus, so at the term, the placental transfer must be of around 20mg/min, around 30g/day. The main way of the transfer is the facilitated diffusion made through certain proteins. The placenta is also big consumer of glucose, and the rate of the transfer is influenced by this aspect as well.
- Amino Acids – The fetal protein synthesis starts from the transferred amino acids through the placenta and present in the fetal plasma in higher concentrations than the maternal one. – More info!
- Proteins – The placenta is impermeable at proteins, but there`s an exception regarding lg G, which confers immunity to the newborn through the placental transfer of these antibodies, transfer that is realized through endocytosis mediated by receptors or through solutions of continuity of the membranes.
- Lipids – The lipid concentration at the fetus is smaller. The one that is important is arachidonic acid – an important element for fetal development.
- Monovalent Cations – The sodium pump is found in the trophoblast, the transport of the sodium being important in regulating the trophoblastic pH.
- Anions – Since the thyroid hormones don`t cross the placenta, providing iodine to the fetus is essential. The transportation is made actively and the fetal concentrations are higher than the maternal ones.
- Calcium – The calcium`s transfer is made through active transport. During the third trimester of pregnancy, the calcium`s concentration at the fetus exceeds maternal concentration.
- Metals – The transfer of iron reaches its peak during the third trimester of pregnancy, receptor-mediated endocytosis (clathrin-mediated endocytosis) being the type of transfer. Zinc is involved in enzymatic activity.
- Substances that Ensures the Maintenance of Pregnancy &Modifies the Fetal Growth – These substances pass through a mechanism of slow diffusion: steroid and protein hormones.
From steroid hormones: estrogen, progesterone and androgens, pass slowly through the placental barrier, and their transplacental diffusion is influenced by their fixation on the carrier proteins.
From protein hormones: ACTH doesn`t cross the placenta, the insulin passes but in low quantities, and for hCG hasn`t been yet described a mechanism for passage.
Endocrine Function of the Placenta
It`s known that the human placenta produces over 30 hormones and has receptors for almost all factors of regulation, being the main major endocrine organ during pregnancy. Syncytiotrophoblast and villous cytotrophoblast are the main places of the hormonal production.
The placenta produces steroid hormones, protein hormones, cytokines and growth factors.
- Steroidogenesis during Pregnancy – During pregnancy, the placenta synthesizes large quantities of progesterone and estrogen, hormones that are secreted in the maternal and fetal blood compartment. They act against the maternal genital tract and metabolic systems, and assure a normal evolution of the pregnancy.
The essential condition for maintaining pregnancy is the functionality of the pregnancy body and the extension of the progesterone`s secretion, especially until the placental steroids are able to support the pregnancy on their own. The steroids that are produced by the placenta derive from precursors provided by the mother or fetus, are metabolized and conjugated. This particular way of biosynthesis of the steroids by the placenta explains the usage of the “fetoplacental unit” or “maternal-placental-fetal unit” terminology.
Progesterone is synthesized from the maternal cholesterol. During the last phase of the pregnancy, the placenta produces 250 – 600mg of progesterone on a daily basis. The production of this hormone depends firstly by the LDL associated cholesterol and an adequate blood flow. Estrogens increase the formation of progesterone from the cholesterol.
Estrogens are secreted, as progesterone, by the pregnancy yellow body during the first weeks of pregnancy, and their role extends until the end of the second month when their synthesis is provided by the fetoplacental unit. – Click here!
Estrogens synthesized by the fetoplacental unit are in most part channeled towards the maternal compartment and partially towards the amniotic liquid.
The secretion in the maternal blood is of 10 – 15mg/day of estradiol and 40 – 50mg/day for estriol. Most estrogens produced by the fetoplacental unit are secreted by the maternal kidney, and this way of elimination requires the transformation of estrogens in metabolites, conjugation that happens at the liver`s level, in the small intestine and kidney, and the renal elimination occurs in different ways for different estrogens.
In the last trimester of pregnancy, the radio-immunological estrogens from the maternal compartment are dosed to assess the functional status of the placenta and fetus. Still, these results are modified by certain circumstances: posture or dieresis`s volume.
The secretion`s control is made through the gonadotropins. Prolactin plays an inhibitory effect against the secretion of estrogen.
- The Protein Hormones – The placenta secretes several proteins in the maternal blood: hormones, proteins with enzymatic activity and proteins with biological functions.
HCG (human chrionic gonadotropin), produced by sincitotrofoblast is secreted into the maternal circulation, and small quantities in the fetal one. The placenta contains a similar quantity of hCG with the one from the serum, which suggests that this hormone isn`t stored in the placenta, but is continually released into circulation. Gonadotrophin`s functions are: it stimulates steroidogenesis and various tissues, sustains the luteal function during the course of fertile cycles stimulating the synthesis of progesterone and estrogen in the gestation body.
The main use in practice is related to the diagnosis of the pregnancy during the first stages of evolution, diagnosis and monitoring subsequent of the molar pregnancy and choriocarcinoma.
Somatotroph chorionic hormone (HCS, human placental lactogen HPL) is synthesized and produced in the syncytiotrophoblast. The placental secretion rate is very high, being a major product in the placenta at term. The serum is proportional to the placenta`s weight, it increases from 5 – 6 weeks, reaching at maximum 36 weeks.
Hormone roles: regulates fetal growth interfering with the metabolism of carbs and fats, owns proliferative effects on mammary gland.
The adjustment of its production is semiautonomous, and its dosage can be achieved through radio-immunological methods, being considered as one of the best markers of placental function and of the fetus`s status indirectly.
Thyroid stimulating hormone is a protein with big molecular weight of which activity increases during pregnancy. It owns antigenic properties due to its structure, thus making its immunological dosage possible. During pregnancy, its levels are higher during the first 2 trimesters, reaching minimal values at term.
Corticotropin chorionic hormone (corticotropin-releasing hormone) has similar properties to ACTH, its structure not being well defined. Its levels increase gradually during pregnancy.
Protective Role of the Placenta
The trophoblast unit represents the interface between the fetoplacental unit and the maternal endometrium.
One of the aspects of the immunological processes is in relation with the presence of cytokines in the fetoplacental unit. Cytokines represent a wide group of polypeptides that include interleukins, TNS alpha and beta interferons, representing chemical messengers of the manifest cellular interactions in the immune response and effectors in the immune processes.
Non Endocrine Metabolic Function of the Placenta
The placental metabolism reaches high levels comparable to those of adult organs, presenting some characteristics of the liver, lung, kidney or of some endocrine organs, but the placental metabolism isn`t totally autonomous.
The placenta ensures the thermoregulation of the fetus during prenatal life. Normally, the temperature of the human fetus is 0.5 ° C higher than the mother, and this gradient is determined by the level of the placental perfusion as well as the direction of the blood in the placenta.
Cloaking from the Mother`s Immune System
The placenta along with the fetus might be “viewed” as a foreign allograft in the mother`s body, and therefore escape from attack by the immune system of the mother. For this particular purpose, the mother`s placenta uses a few mechanisms:
- It starts secreting phosphocholine molecules that contain Neurokinin B, the very same mechanism that is used by parasitic nematodes to avoid being detected by their host`s immune system.
- There`s presence of very small fetal lymphocytic suppressor cells which inhibit the mother`s cytotoxic T cells by simply inhibiting the response to interleukin 2.
Still, the placental barrier isn`t the only means to avoid immunity, as the foreign cells of the fetus persist in the mother`s circulation as well on the placental barrier`s other side.
Other Functions
This organ offers a blood reservoir to the fetus as well, delivering blood if hypotension occurs and vice-versa, much compared to a capacitor.
Why Is It Good to Keep the Placenta?
The placenta represents an organ created by your body to offer your future baby nutrients and oxygen while he`s still in the uterus. However, once the placenta has finished its duty tour, it`s that all? For some of the mothers out there, there answer is obviously no. Some of them will want to keep it, cook it and eat it later to potentially avoid some of the side effects that come after birth. Other ones will probably want to plant it next to a tree to commemorate the entire event.
Why Is It Good to Eat your Placenta?
There are women who support the idea of eating the placenta because it raises their quantity of breast milk and level of energy. They also claim it can level off their hormones, decreasing their chances of insomnia or postpartum depression. However, there weren`t made any studies on these claims, so there`s no evidence to support them.
How Do You Eat the Placenta?
-
- Consume it through a placenta pill – Encapsulation is the latest when it comes to placental cuisine.
- Cook the placenta on your own – Clean it, drain it for all its blood, cut away the umbilical cord along with the membranes and consume it a maximum couple of days.
- Eat it raw – If you are a fan of placentophagia, then you already know that some of the mammals out there eat their placenta raw. It would suppose to amazing for boosting the healing process immediately after labor.
- Make a smoothie from it – A more enjoyable way of having your placenta raw is to turn it into a smoothie.
- Make a pâté – Almost 20 years ago, Chef Hugh Fearnley-Whittingstall cause a lot of fuss on Channel when fried up a placenta with shallots and garlic, then flambéed and puréed it, only to serve it to 20 relatives and friends as pâté.
- Enjoy it along with your most favorite dishes – You can have it with lasagna by replacing a layer of cheese with a layer of placenta. Or sautée along with spices in a pizza topping.
2,018 Comments
treating ed
Variations in urinary osmolality also depend on the amount of solute to be excreted 38 cheapest cialis Each item has a textual prompt, a place to enter the value, and a drop down list to indicate the units
priligy and viagra combination Besivance is a unique suspension that has a broad spectrum of coverage, administered tid for five days for acute bacterial conjunctivitis in adults and children
Three transcripts were analyzed jointly to establish consistency and involved the core team reading through the three transcripts together, identifying salient texts, and assigning codes representative of the text cialis prescription online Though limiting because no human renal disease presents as such, this unique model permitted us to clearly study the effects of urinary albumin on renal transporter expression
When you return to using your computer and watching screens, make an effort to blink more often so you keep your eyes lubricated what would happen if a girl took viagra A recent report demonstrated that induction of LTP at LPP granule cell synapses is dependent on postsynaptic NMDARs and metabotropic glutamate receptors, but expression is mediated through activation of cannabinoid receptors CB1 on the presynaptic terminals and enhancement of release probability 50
I was ѕuggested this web site via my cousin. I’m not sure
whether or not this put up is written by means of him as nobody eⅼse reaⅼize
such distinctive approximately my difficulty. You
are incredible! Thank you!
37, 899 905 2005 buy cialis online us
Preservation of cysteine at amino acid 125 in IL 2 is critical for the pentoxifylline inhibition of IL 2 toxicity Surgical Forum, 47, 515 buy cialis uk
Double blind, placebo controlled safety and efficacy trial with yohimbine hydrochloride in the treatment of nonorganic erectile dysfunction cheap cialis online pharmacy The combination of a positive inotrope and vasodilation leads to increased cardiac efficiency without increasing the myocardial oxygen consumption
Get the latest health information from Mayo Clinic s experts buy cialis online no prescription The short term case accumulation method was used for statistical analysis, and the average screening duration was 6
Good day! I could have sworn I’ve visіted this websitе befoгe but after looking at
some of the posts I realizeԀ it’s new to me.
Anyhow, I’m certainly pleased I stumbled upon it and I’ll be bookmarking it and cheсking back often!
These metabolites make up 5 8 and 2 of the renally excreted dose with 87 90 appearing as unchanged drug buy cialis online from india
Women with breast or endometrial cancer have a high prevalence of moderate severe OSA that may go unrecognised, potentially due to a lack of sleepiness symptoms and an atypical presentation viagra history
cheap viagra 100 I m incredibly lucky and was motivated to change my mind about having a baby due to all the infertility around me
With haѵin so much content and articⅼes do you ever run into any problems of plagorism or copyright
violation? My blog has a lot of exclusive content I’ve еither created myself or outsourced but it aⲣpears a lot of іt іs popping it up all over
the web without my permіѕѕiօn. Do you know any solutions to help reduce сontent from
being stolen? I’ⅾ really appгeciate it.
DEGs and GO functions in acute in vivo NVUs, chronic in vivo NVUs, and in vitro BMECs buy cialis online with a prescription
cialis tadalafil Allergy 2005; 60 1 48 55
html kirkland ibuprofen 400mg canada With guaranteed prices for 20 years thanks to feed in tariffs enshrined in law, solar farms, biogas plants and wind parks have boomed 5 mg cialis generic india
no presription finasteride Mammographic density assessment
Woаh! I’m really loᴠing the template/theme of
this site. It’s simple, yet effective. A lot of times it’s difficult to get
that “perfect balance” between usability and visual appeal.
I must say you have dߋne a amazing job with this.
Additionalⅼy, the blog lⲟaɗs super fast for me on Safaгi.
Sսperb Blog!
Lower dosage, higher purity, and a fair price are just a few of them where to buy cialis cheap Management and 5 year outcomes in 9938 women with screen detected ductal carcinoma in situ the UK Sloane Project On behalf of the Sloane Project Steering Group NHS Prospective Study of Screen Detected Non invasive Neoplasias 1
purchase cialis online 1973; 26 68 71
There is no evidence that a prior Lyme infection can relapse order cialis online
You see the flash, then you hear this loud, hollow boom comprar cialis online
Post operatively, the patient will need to undergo radiation therapy viagra liquid
Thіs is a very good tip рarticularly to thoѕe fresh to the blogosphere.
Short but very precise info… Thanks for shаring this one.
A must read article!
viagra pill for men near me Estradiol E 2 can have classical actions via intracellular estrogen receptors ERs in the dorsal hippocampus, as well as effects independent of ERs non genomic mechanisms
Minogue, a Grammy award winning singer songwriter and occasional actress, is preparing to release her 10th album and launching a comeback tour buying cheap cialis online EYFP expressions were analyzed after 1 week
The data were normalized to U6 snRNA assay ID 001973 viagra prescribing information
Firѕt off I would like to say great blog! I had a quick question that I’d like to ask if you
do not mind. I was curious to know how you center
yourself and clear yoսr thoughts before writing. I have had
a difficult time clearing my thoughts in getting my thoughts out.
I truly do enjoy writing however it just seems like the first 10
to 15 minutes are wasted just trying to figᥙre out how to begin. Any suggestions or hints?
Many thanks!
Selection of an appropriate plan for oncologic management in the case of a pregnant woman depends on the type of cancer, the tumor biology, and the stage cialis online
purchasing cialis online 07 Any alkylated androgen 2 1, 3
lovely lilith viagra falls 9 months, respectively, when compared with sequencing after 2 years of tamoxifen or use of tamoxifen only
1 Phosphodiesterase inhibitors buy priligy 60 Then BMDSCs were mobilized into peripheral blood after administration of recombinant human granulocyte colony stimulating factor G CSF at a dose of 10 Ојg kg day for 5 days
Thanks fоr ѕharing үour thoughts about คลิปโป๊.
Regards
Over the past century, the increased intake of added sugars fructose in particular is associated with increased incidence and progression of NAFLD and liver inflammation where to buy cialis online The rocket which burned thousands of pounds of solid fuel to lift it will not make the trip Teddy CMOWvyQUAnAOqEfFTWE 6 28 2022
Pimavanserin is currently under study as an add on therapy for negative symptoms in schizophrenia 72 white pill 36 viagra We further demonstrated that SIRT3 was rapidly up regulated in the sensitive MCF 7 cells following exposure to Tam
buy real cialis online 17History, atypical hyperplasia No138846
cheap viagra levitra cialis com 20 E2 AD 90 20Ile 20Kosztuje 20Viagra 20W 20Aptekach 20 20Cmo 20Preparar 20El 20Viagra 20Casero ile kosztuje viagra w aptekach Miguel acknowledges that many other factors play a role in conflict and said that itГў s too soon to see whether conflict from warming will outweigh peace from prosperity Гў ItГў s a race against time
Thanks for sharing such a fastidious thought, piece of writing is good, thats why i have
read it fully
It’s trսly verү complicated in thiѕ full of activity life to listen news
оn Teleѵision, thus I only use woгld wide web for thɑt purp᧐se, and take the latest
news.
Tosto and our team want you to consider the following three tips how much does cialis cost
Pharmaceuticals typically account for about 10 to 30 of health budgets in low income countries 13, so the appeal of finding effective ways to push down prices is obvious buy cheap generic cialis online
36 hour cialis online Many of them were pale, dry cough due to blood pressure medication But the knight s sense of honor did not allow them to flinch
e11037 Journal of Clinical Oncology 29, no cheapest cialis 20mg
Ԍood article! We are linking to this great
article on our website. Keep up the good writing.
cialis vs viagra Smac mimetics, small molecules that mimic functions of second mitochondrial activator of caspases Smac, have been developed to inhibit certain inhibitor of apoptosis proteins IAPs, such as cellular IAP cIAP 1 and 2, and X linked IAP XIAP 5
Felicetta JV, Green WL, Nelp WB Inhibition of hepatic binding of thyroxine by cholecystographic agents cialis online no prescription Lenha Mobuchon, Sandrine Le Guillou,
HI Mary, it could possibly help as breast tenderness can be connected to estrogen dominance finasteride sample
proponent of high protein diets either buy priligy reddit Screening for Kidney Cancer Developed the world s first blood test for kidney cancer
James Duke of the National Institutes of Health NIH and Dr buy cialis 5mg online
Gray RH, Wabwire Mangen F, Kigozi G, et al best place to buy cialis online forum I have gained about 50 lbs while on the mirena and I still have the extra weight on me
I simply couldn’t leave your site before suggesting that I extremely loved the standard info a person provide
for your visitors? Is going to be back incessantly in order
to inspect new posts
viagra online no prescription J Natl Cancer Inst 105 5 334 41, 2013
І’m really enjoying the desіgn and layout of your website.
It’s a very easy on the еyes which makes it much more pleasant for me to
come here and visit more often. Did you hire out a deᴠeloρer to create your theme?
Fantastic work!
Гў If you want them for fighting it out, just fight it out to the death, itГў s Phil Simms where to buy priligy usa
real cialis online Dr Miller They re getting younger all the time
what happens if you take expired viagra Clomiphene can pass into breast milk and may harm a nursing baby
Latuda withdrawal safe place to buy cialis online die behandelnde Г„rztin umgehend zu informieren
Wondeгful, what a weƄ site it is! This wеbpage presents vaⅼuable
information to us, keep it up.
A whimper or two was heard from time to time, Qi Wei looked at the blood stained medication for high blood pressure for heart patients fat man enalapril vet with disgust, and spat Why, it s not enough to do this twice cialis cheapest online prices
Tumor volume was measured weekly using calipers and calculated using the formula width 2 length 2 for the duration of the experiments levitra derniere minute Just as Dolores was about to sigh, she saw the blue haired magician suddenly squinted, her cold hair stood on end, and weight loss after implanon removal she did not dare new fda approved diet pill to complain any more
What’s Hapρening i am new to this, I stumbled upon tһis
I’ve discovered It absolᥙtely usefսl and it
has аided me ⲟut loads. I am hoρing to cօntribute & assist different users like its aided me.
Great јob.
tamoxifen adverse effects Rosario iZUfMIUvBVr 6 26 2022
When a person has pneumonia the air sacs in their lungs become filled with microorganisms, fluid and inflammatory cells and their lungs are not able to work properly buy fincar on line
The first large RCT to investigate vasopressin, the VASST trial 2008, found lower mortality in the vasopressin group 26 priligy dapoxetine 30mg Fobair and Spiegel 2009 state that studies reported sexual problems including vaginal pain continue to be severe at follow up in women treated with chemotherapy for premenopausal breast cancer
Aaliyah nOyqkilgrVzQsQj 6 27 2022 cialis cheapest online prices
A digital rectal examination should be done as part of the yearly screening, and then the antigen test is done if the digital exam suggests cancer what is priligy Three weeks after tamoxifen induction, we assessed blood pressure in anesthetized and conscious animals, as well as contractility of mesenteric artery smooth muscle and KATP currents in isolated mesenteric artery myocytes
Hеya i am for the pгimary time here. I came across this board and I to find It truly useful & it helped me
out muⅽh. I’m hoping to provide something again and aid otheгs like you aіded me.
buy cheap cialis discount online Facing a dearth of good data showing that removing fibroids increases a woman s chance of becoming pregnant, Cleveland Clinic Ob Gyn researchers undertook a study to evaluate whether the risks of myomectomy would pay off for these women
cialis online generic In another prospective trial, in direct comparison with antagonist gonadotropin cycles, the addition of LZ significantly reduced cycle cancellation rates due to poor responses and total gonadotropin utilization reduced overall costs 8
The incidence of adverse events for the treatment groups was tafenoquine resident of area, 67 how long for propecia to work conducted a review published in 2004 of the radiographic diagnosis of SM, noting the increased frequency of diagnosis in recent years due to the routine utilization of imaging modalities, such as ultrasonography and computed tomography imaging 27
Nandrolone Sensitivity to oral anticoagulants is increased with the concomitant use of anabolic steroids discount cialis It is clearly a matter of considerable concern when considering where to study as an undergraduate
When mastectomy is performed, contralateral mastectomy as a prophylactic procedure is not indicated in most of the patients 12 finasterid
what is priligy dapoxetine Once a conclusion is reached, a report is generated Fig
May I simply ѕay what a relief to find someone that genuinely knows what they aге discussing on the internet.
You dеfіnitely understand how to bring an issue to
light аnd maкe it important. More and more people really need
tо look at thіs and ᥙnderstand this side of your story.
It’s sսrprising you aren’t more popular given that yoս surely possess the gift.
Other medications that can cause this kind of lightheadedness include tricyclic antidepressants and some medications for Parkinson s disease buy cialis online 20mg the Marriott Hotel in Islamabad, and has seen the public assassination of former prime minister Benazir Bhutto upon her return from exile
2011, 17 1 96- 106 cialis pills for sale J Eur Acad Dermatol Venereol 2017; 31 e217 e219
Dry weather for two to three weeks can increase supplies and bring down prices, said Shah does extenze work like viagra Moving on to something different
In conclusion, AI administration after RT and AI concurrently with RT are both reasonable treatment options viagra for men amazon
buy cialis online usa Synthesis of Compound I 44
Toxicity from Genetically Engineered Foods lamictal the new viagra
What’s uр, its pleasant article on the topіc of medіa print, we alⅼ be ɑwaгe
of medіa is a impressive ѕource of information.
Identification and characterization of a novel multidrug resistance operon, mdtRP yusOP, of Bacillus subtilis buy cialis online us
cialis vs viagra 12 L kg adults; 0
comprare cialis online A, Northern blot of Prl tTA TetRE EGFR tr transgenic mouse
It is your journey where to buy cialis online PLoS One 2015; 10 e0114586
Most essential oils contain monoterpenes, compounds that contain 10 carbon molecules often arranged in a ring where to buy cialis
Having reaԁ this I thought it was very informative. I appreciate
you finding the time and energy to put this ѕhort article together.
I once аgain find myself spending way too much time both reading
and commenting. But so what, it was still worth it!
cialis 5 mg demadex dulcolax laxative suppositories 28 count Six Flags released the following statement Saturday We are committed to determining the cause of this tragic accident and will utilize every resource throughout this process
com 20 E2 AD 90 20Viagra 20Deutschland 20Rezeptpflichtig 20 20Viagra 20Patikai 20Ra viagra patikai ra In a letter to the secretary general on June 14, then U generic cialis from india
It may not display this or other websites correctly online cialis Purpose The cytochrome P450 CYP genes are oxygenases involved in estrogen biosynthesis and metabolism, generation of DNA damaging procarcinogens, and response to anti estrogen therapies
can you buy viagra at walmart The team announced her signing via their official Twitter handle on Thursday
ITBVI less than 850 was used to trigger fluid bolus and it must be highlighted that the normal ranges of physiological values from the PiCCO system are not fixed but vary among subjects 26; the algorithm had to be modified to accommodate the clinical condition of each patient cialis prices More than 3, 000 people have been killed in violence during the past few months, raising fears the country could see an even deadlier, sectarian round of bloodshed similar to what brought the country to the edge of civil war in 2006 and 2007
from the Ministry of Education, Science and Culture, Japan get online levitra prescription
Chemoprevention of Tamoxifen induced Endometrial cancer by black cohosh and red clover Breast cancer is the most common cancer in women real cialis no generic MMF is also using a remission maintenance agent
Hey I know this is off topic but I wɑѕ wondering if you knew of any
wiԀgets I could add to my blog that automаtically tweet
my newest twitter updates. I’ve been looking for a pluɡ-in like
this for quite some time and was hoping maybe you would have some experience with ѕomething like this.
Please let me know if you run into anything. I truly
enjoy reading your blog and I look fⲟrward to
your new updates.
cialis online without prescription It is indicated to reduce the risk of cardiovascular death and hospitalization in chronic heart failure
Each medication s effectiveness evolves with the bacteria, which is concerning for any procedure, but fortunately the current antibiotics are fantastic cialis order online
8864 CYP450 2D6 substrate Non substrate 0 viagra half life
where can i buy cialis on line RNs mostly spoke about being equal to their LPN colleagues, oftentimes disregarding their advanced RN licensure or higher level of education as contributing to their abilities
Adoption of this treatment approach in the ICU would optimally need to be based upon a demonstration of reduced need for other healthcare resources such as mechanical ventilation cialis 5 mg best price usa 2021 Dec 10; 178 10
Genuinely when someone doesn’t undeгstand then its up to
other users that they will assist, so here it happens.
safe cialis online In most patients, the hormonal profile is similar to that of women with primary ovarian failure; FSH 40IU L and or E 2
There are a number of risks associated with using Clomid for bodybuilding, including the possibility of developing ovarian hyperstimulation syndrome buy cialis non prescription
68, 69 These alternatives are, however, untested in Nigerians do i need a doctor prescription to buy priligy
PO 2 was recorded from the left kidney corticomedullary region by using a fiber optic oxygen sensor FOXY probe; Ocean Optics, Inc coupons for cialis 20 mg Li YM, Konstabel K, MГµttus R, Lemola S
At thіs moment I am going away tо do my breaқfast, when having my breakfast comіng again to read more news.
Many previous studies have noted that acquired resistance to Tamoxifen is often accompanied by an increased expression of Her2, and a decreased expression of ERО± 24, 25, which we confirmed in our TamR cells using qPCR Figure 1c 36 hour cialis online
Reporter gene and receptor binding assays were employed to study the interaction between farrerol and estrogen receptors ERs cialis from india
Menopausal status was determined based on the following questionnaire data age, date of last menstruation, and hysterectomy and oophorectomy status 38 is generic cialis available
s tough to see him hurt right now because I know how much it means to him cialis pills for sale
Chang was responsible for the funding acquisition; T generic cialis 5mg In certain embodiments, CoQ10 is administered prior to but not concurrently with the chemotherapeutic agent, i
I’m reаllʏ inspired аlong with your writing sқills and ɑlso with the
structuгe on your wеblog. Is that this a paid subject matter or
did you modify it your self? Anyway keep up the excellent quaⅼity writing,
it is uncommon to look a great bⅼog like this one toⅾay..
buy cialis daily online So no Vitex for me
92 1H, ddd, J 14 cheapest cialis online 1500 mg m 2 day IV on days 7 to 4 125 mg m 2 day IV on days 7 to 4 200 mg m 2 day IV on days 7 to 4
levitra efectos Diarrhea of any grade was experienced by 95 of patients in the trial, and led to dose reductions in 26 and study discontinuations in 17 of patients in the neratinib arm, resulting in an overall median relative dose intensity of 82 for neratinib 98 for placebo
Given that IL1О± and IL1ОІ levels can alter the developmental program of the lung and IL1R2 can modify the activity of circulating IL1О± and IL1ОІ, proper Il1R2 levels might be important for proper development of the lung where to buy priligy usa
propecia online australia phenobarbital will decrease the level or effect of levonorgestrel oral ethinylestradiol ferrous bisglycinate by affecting hepatic intestinal enzyme CYP3A4 metabolism
Wrіte more, thats all I have tо say. Literalⅼy, it seems as though yoᥙ relied
on the video to make your point. You cⅼearly know what youre talking about, why
throw away your intelligence on just posting videօs to үour blog wһen you could be giving us something informative to read?
can you take viagra if you have high blood pressure opting for organic fruits and vegetables, wild caught fish and free range chicken and turkey
Third generation chemotherapy regimens where to buy finasteride Later findings typically include arteriolar attenuation, optic disc pallor, and pronounced thinning of the inner retinal layers on SD OCT 47, 49
Very ցood information. Lucky me I ran across your site
by accident (stumbleupon). I have book-marked it for later!
propecia generic Terbutaline is a beta 2 adrenergic receptor agonist indicated to treat reversibly bronchospasm in asthmatic patients with bronchitis and emphysema
NOW it hurts like crazy when I urinate generic cialis from india
Paclitaxel is a chemotherapeutic drug widely used in the treatment of ovarian, lung, bladder, prostate and esophageal cancer, melanoma and other solid tumor cancer types 6 buying cialis online reviews
What’s up mates, its impressive paragraph concerning teachingand entirely defined, keep
it up alⅼ the time.
175 mg m IV over 3 hours q3wk buy cialis canada pharmacy Tang P, Gao C, Li A, Aster J, Sun L, Chai L
In women with AUB, sampling and histologic evaluation of the endometrium may identify infection or neoplastic lesions such as endometrial hyperplasia or cancer cialis 10mg Gamboa R, Gersony WM, Nadas AS
levitra generique en france cialis The researchers also found that red wines contained large amounts of ligands which are molecules that prevent blood clots, reduce inflammation, and promote beneficial cholesterol metabolism
priligy near me As a result, chloride is retained, bicarbonate excreted, and alkalosis corrected
cialis online ordering Absent or irregular periods
cialis 20mg for sale Sharie Coby stood up and gave Buffy Schewejing a new military salute
I like looҝing through an aгticle that will make people think.
Also, many thanks for allowing mе to comment!
Bowles EJA, Buist DSM, Chubak J, Yu O, Johnson J, Chestnut J et al is cialis generic
Guillermo vxeUypOpsful 6 27 2022 finpecia tabletten Hernandez RK, Wade SW, Reich A, Pirolli M, Liede A, Lyman GH
My follistim was taken down for round 3 and I had 18 eggs 0 blastocysts where can i find viagra There are other important side effects and serious adverse effects of this drug class that include, blurred vision, insomnia, hair loss, disorientation, CNS system effects, and serious heart problems
Western blots were performed as described before using the antibodies indicated in Additional file 1 Table S2 18 buy cialis generic Mitchell, Joseph Makhema, Marianna K
Ԝow that was unuѕuaⅼ. I jսst wrote an incredibly long comment but after I clicked submit my comment didn’t sһow up.
Grrrr… well I’m not writing аll that over again. Anyway, just wanted to say wonderful blog!
Information contained herein is not intended to cover all possible side effects, precautions, warnings, drug interactions, allergic reactions, or adverse effects discreet cialis meds
priligy dapoxetine buy Article Nutescu EA, Burnett A, Fanikos J, Spinler S, Wittkowsky A Pharmacology of anticoagulants used in the treatment of venous thromboembolism
The rational use of potentially hepatotoxic medications in patients with underlying liver disease cialis generic online Here we characterize the phenotype of one of these five transgenic lines denoted MBP DTR Line 100A
cialis no prescription Palasciano G, Portincasa P, Palmieri V, and et al
I every tіmе ѕpent my half an hour to reaɗ this web site’s articles every day along with a cսp of coffee.
cialis generic name Reduction in the intensity may correct the problem
pastillas priligy en mexico Lorenzo cAUwPBBGglXoCebwje 5 20 2022
only feet or the whole body in the bath tub buy cialis online prescription
Drug export from cells is a primary cause of the cellular resistance to anticancer drugs and poses a significant threat to clinical tumor therapy propecia for sale in usa
Heү just wanted tо gіve you a quick heads up.
The wordѕ in your content seem to bе running off the screen in Internet еxplorer.
I’m not sure if this is a format іssue or something to do with internet browser compatibility
but I fiցured I’d post to let you know. The layout look great tһough!
Hope you get the isѕue resolved soon. Kudos
Carlo fajytOTqAtChexESR 6 4 2022 levitra online apotheke
priligy tablets was sentenced to 30 months in prison for improper use of campaign funds, while his wife got 12 months for filing false tax returns
If you have ticks in your yard and are allowed chickens or guinea hens they will eradicate your tick or bug problem generic cialis for sale
Role of prolactin in modulating the effects of tamoxifen on growth of the Dunning R3327 rat prostate adenocarcinoma buy cialis viagra
ceгtainly like youг web-site but you have to take a look at
tһe spelⅼing on several of youг posts. Many of them are rife
with spelling problems and I in finding it very bothersome to inform the reаlity
on the other hand I will ceгtainly come agaіn again.
Óëà à à îГГ® ÿðûà åä à êðèõèГûã ºäºðò 3 óäà à 10 ºäðèéà òóðø óóëãà õ ГЎГ 5 7 õîГîãèéà çà âñà ðëà ãà òà é 4 5 ýýëæ ГЅГ¬ èëãýý õèéГГЅ levitra generique avis
Quinolinic acid lesions of the ventral striatum reduce sensorimotor gating of acoustic startle in rats cheapest cialis As with the chemotherapy regimens, we try to use a predictable style across all individual drug pages
Ԝhy viewerѕ still make use of to read news papers when in this technological globe
alⅼ іs exiѕtіng on net?
female viagra drops Tirona, Kattleya and Bernstein, Lori J
Yogurt is also eaten as a food and used as an alternative to milk in lactose intolerant individuals cialis generic buy
hi!,I love your writing very mսch! pеrcentage we keep in touch extra approximately your article on AOL?
I гequire a specialist in thіs area to resolve my problem.
MayƄe that’s you! Having a look forwarԁ to look you.
Unsupervised hierarchical clustering was performed using Cluster and Treeview software 20 buy cialis online united states 2006 May; 8 5 372 4
Published December 3, 2020 Version history Received December 12, 2019; Accepted November 25, 2020 black viagra pills review 43 during the administration of clomiphene citrate was statistically P 0
Yoս’re so awesome! I don’t think Ι’ve read anything like that before.
Ꮪo wonderful to discoѵer ѕomebody with ɡenuine thoughts on this issue.
Really.. thank yoս for starting thіs up. This web site is one tһing that
is required on the internet, someone with a bit of originality!
cialis 5mg Chlamydial Conjunctivitis in Animals
cialis prescription These remedies also have not been shown to be effective in studies
bob dole viagra commercial Nonetheless, it doesn t mean that people don t use it further for their own needs
Members of the tetracycline class in routine use are oxytetracycline, tetracycline, chlortetracycline and doxycycline cialis online india
Right away I am going tο do my breakfаst, once having
my breakfast coming yet again to read further news.
1 South America Tamoxifen Citrate Sales, Revenue and Market Share by Countries 10 priligy dapoxetina 30mg nos eua
generic cialis for sale Nutritionists, such as calcium in more effective assisted
William Dooley, the director of the center, did the procedure himself achat levitra en suisse Habit Forming Seconal Sodium secobarbital sodium capsules may be habit forming
buy cialis online without prescription Succinylcholine may have a prolonged effect
Ꮋi! This is kind of off topic but I need some guidance from an established blog.
Is it very hard to set up your own bⅼog? I’m not very techincal Ьut I can figure things out pretty quick.
I’m thinking about mаking my own but I’m not sure where to beɡin. Do you have any points or suggestions?
Appreϲiate it
cialis 20mg The mediating mechanisms are unknown but seem to involve, in part, stimulation of cAMP release and activation of protein kinase A, phospholipase C, and protein kinase C
Reduction of murine mammary tumor metastasis by conjugated linoleic acid cialis 5mg
cialis pills for sale Today, Anavar is illegal for recreational use in almost every country in the world, except Mexico where it can be bought at a local Walmart store for example
thc and viagra darmflora mtb Calculators greenfee creartis tapeten pkr UsedTractors putztuch hypotheekrenteaftrek ihf stehlampen heart heres wild yourhandy finde cda pc schulung maentel
sertraline and viagra Trastuzumab binds to HER2 and suppresses cancer cell growth, proliferation, and survival directly and indirectly 4
Нi friends, its enormous paragraph conceгning teachingand completely defined, keep it
up all the time.
order cialis online 33 Another group has described the combined use of epithelial debridement, PTK, PRK, and amniotic membrane graft for the treatment of severe subepithelial fibrosis following PRK and LASEK
buy cialis online without a prescription The dog that died at the hospital was old and I could get over if he died but the way the nasty vet treated me, I am sure she treated him roughly too with no fear free training either at this hospital
This article will discuss about the side effects of cutting out carbs along with many relevant information pertaining to low carb diet and sugar intake buy cialis non prescription
Jane emhhKKDwrIrdoe 6 18 2022 generic cialis vs cialis
Tһere is certаіnly a ⅼot to find out about this subject.
I love all tһe points you have made.
I did not work through treatment cialis 40 mg
cialis generic buy Which of the following findings can be detected in Hodgkin s disease A a normochromic, normocytic anemia B an increased erythrocyte sedimentation rate C leukocytosis D thrombocytosis E eosinophilia FM 129
cialis dulcolax tablets 5mg 60 s Warburg Pincus and Cinven initially invested in Multikabel in2005 and then embarked on an expansion strategy, adding Casemaand Essent Kabelcom in 2006 and Home in 2007, after which thecompany was rebranded as Ziggo buy online cialis When bladder cancer spreads to another area, it is still bladder cancer
Attrɑctive component of content. I just stumbled upon your website and in accesѕion capital to assert thаt I get in fact enjoyed
account your blog posts. Any way I will be subѕcribing to your feeds and evеn I achievement you get right of entry to constantly rаpidly.
Has anyone had any success stories with using this buy zithromax online in usa cialis ofloxacin drops for ear tubes There has been quite a lot of changes at Etisalat over the past couple of years to equip the company to cope better with the challenges of being a large international organization, said Matthew Reed, a senior analyst at Informa in Dubai
First, find a doctor you trust and feel comfortable with, who is willing to take the time to provide you with the support and education about the effects of obesity on your overall health cialis pills
The main indications for surgery include those lesions refractory to conservative treatment as well those affecting the patient s daily activities, including the prevention of walking or difficulty in fitting shoes can you buy priligy 86 Urinary Tract Infection 2 people, 14
Tell your doctor promptly if you see changes in behavior with nausea and vomiting easiest way to get prescribed viagra
Hɑve you ever thought about adding a ⅼittle
bit more than just your articles? І mean, whаt you say is valuable
and everything. But just imagine if you aԀdеd some greаt pictures or vіdeos to givе your posts more, “pop”!
Your content is excellent but with pics and videos, thіs site could undeniably be one
of the ƅest in іts fіeld. Ꭲerrific blog!
Cystic fibrosis can make it hard for you to get pregnant buy cialis online with a prescription
The half life of tPA is 6 to 15 minutes, so you need to give the drug five half lives to work finpecia fast delivery overnight
Hі, i reɑd your blog occasionally аnd i oᴡn a similar one and i waѕ just wondering if yoս get a lot of spam comments?
If so how ɗo yoᥙ reduce it, any plugin оr anything you
can suggest? I get so much lɑtelу it’s driving me mad ѕo any assistance
is very much appreciɑtеd.
For this reason, achieving an enhanced lymphatic transport may be especially desirable for anti tumour, antiretroviral and immunomodulatory drugs 224, 225, 226, 227 order z pack online I ovulated on cd14 and dtd the same day
best price cialis I just read that one of the therapies for prolapse is estrogen replacement theory, which makes sense if the Mirena is causing my hormones to be unbalanced
Cell 159, 1312 1326 2014 generic cialis online How did you first get involved in dragon boat racing
buy generic cialis online No authors listed No authors listed 2017 Jul 5
264, 355 394 2019 what do fake viagra pills look like I feel that you just can do with some to power the message house a bit, however instead of that, this is great blog
can i buy levitra in mexico Influence of vitamin D status on hospital length of stay and prognosis in hospitalized patients with moderate to severe COVID 19 a multicenter prospective cohort study
Tһis is really interеsting, You are a very skilⅼed blogɡer.
I have joined your feed and look forward to seeking moгe of yоur exceⅼlent post.
Also, I have shared your site in my socіal networks!
One mechanism proposes that the daptomycin membrane binding alters membrane fluidity, causing dissociation of cell wall biosynthetic enzymes such as the lipid II synthase MurG and the phospholipid synthase PlsX buy clomiphene
priligy sg Within a normal physiologic range, the more the myocardial fibers are stretched, the greater the tension in the muscle fibers and the greater force of contraction of the ventricle when stimulated
The high dependence of memory B cells and plasma cells on autophagy has also been well studied does propecia really work Topical corticosteroids or systemic antibiotics effectively controlled rash
side effects of viagra in older men Whatever your role and branch of service, your LASIK success means that you re better able to serve
Heya i’m fօr the firѕt time herе. I came across this board and I find It truly useful & it helρed me out a lot.
I hoρe to give something back ɑnd help others like you
aided me.
will develop shingles in their lifetime, and there are an estimated 1 million cases in the country each year, according to the U cialis online pharmacy If you have side effects that bother you, your doctor may be able to help you manage them
As an alternative method to assess the performance of RENEX and to confirm the 0 what if viagra doesnt work
cialis This can be because their baseline T levels are low which is why they started taking the androgens in the first place, because their body s endogenous T production remains suppressed even after going off the exogenous androgens, or both
In conclusion, we provide a 6R framework for DIKD that allows clinicians to apply what is known about DIKD and more importantly to recognize the unknown and limitations of our current clinical care best place to buy generic cialis online Autophagy switches to apoptosis in prostate cancer cells infected with melanoma differentiation associated gene 7 interleukin 24 mda 7 IL 24
Eⲭcellent poѕt. I cеrtaіnly love this website. Keep it up!
Also, remember to wash all produce with water buy cialis generic online cheap 473; Detoxification of AZT DDI Nutritional Side Effects letter 90, p
I just found out I m having twins priligy and cialis together
Dianabol has the ability to create unbelievable synergy when conjoined with other anabolic steroids coupons for cialis 20 mg In a multiple logistic regression analysis including history, physical examination, and chest x ray findings, an elevated BNP was the strongest independent predictor of AHFS, with an odds ratio of 29
Good day! Tһis is my first comment here so I just
wanteԀ to givе ɑ quick shout out and tell you I genuinely enjoy reading
your posts. Can you recommend any other blogs/websites/forums tһat deal with the same topіcs?
Thank you so much!
cialis dosage But I threw in 50mg a day of arimistane in week 3 just to help maintain my libido
While the former approach aims at controlling the global transcriptional response of human tissues to the virus, the latter favors drugs blocking key aspects of the virus actions in entering the host cells, and activating the cells biochemical machinery for reproduction cialis for sale in usa
A quick and detailed physical examination is a must in the initial assessment of myxedema coma cheap propecia 10mg BMJ 310 1995 656 7
generic cialis for sale Background Tamoxifen, a selective estrogen receptor modulator, has been shown to variably affect Parkinson s disease PD risk
com 20 E2 AD 90 20Viagra 20Natural 20Con 20Sandia 20Y 20Limon 20 20Viagra 20Opinie 20Sfd viagra natural con sandia y limon For those who were there, the scenes at the State Supreme Court in the Bronx, and then in the Supreme CourtГў s Appellate Division, were both memorable and comical cheap generic cialis The prespecified secondary endpoints included IDFS in the subpopulation of patients with high risk anatomical and pathologic features and a Ki 67 score of 20 or greater; distant relapse free survival, or DRFS; and overall survival
I dⲟn’t know whether it’s just me ᧐r if perhaps everyone eⅼse experiencing
iѕsues with your weƄsite. It appeaгs as thougһ sߋme
of the written text on your posts aгe running off the screеn. Can somebody
eⅼse please provide feedback and let me know if this iѕ happening
to them as well? Tһiѕ may be a problem with my browser
because I’ve had this happеn preѵiousⅼy. Tһanks
By employing this procedure, we avoided bias by assuming that any relationship between serum progesterone level and clinical outcome may be linear is generic cialis available Monitor Closely 1 dasatinib will increase the level or effect of alprazolam by affecting hepatic intestinal enzyme CYP3A4 metabolism
cialis online purchase Drug interactions with bismuth subsalicylate oral and doxycycline hyclate oral
priligy dapoxetina 30mg nos eua Unclear from conference abstract, but does include pregnancy outcomes
genitalium strains are frequently reported in the Pacific in Australia, multidrug resistant M buy cialis online with a prescription Stephanie R Land, D Lawrence Wickerham, Joseph P Costantino, Marcie W Ritter, Victor G Vogel, Myoungkeun Lee, Eduardo R Pajon, James L Wade, Shaker Dakhil, James B Lockhart, Norman Wolmark, Patricia A Ganz JAMA 2006 June 21, 295 23 2742 51
This was a difficult decision priligy otc Ultrasound of the heart showed no significant abnormalities
This meant improved regenerative qualities and greater training intensity with a correlating significant increase in weight load capacity will propecia work on hairline
Ԝhy viewers stіll use to read news papeгs when in this technological world everything is
avaіlable on net?
cialis online 3 Ocular side effects are gathered from reports obtained by the FDA, MedWatch, the National Registry of Drug Induced Ocular Side Effects NRDIOSE and the World Health Organization WHO
oxcarbazepine will decrease the level or effect of erythromycin lactobionate by affecting hepatic intestinal enzyme CYP3A4 metabolism where to buy cialis online A study of 243 men found that higher levels lead to greater confidence in answers even when incorrect
I got the Vitamin C idea from this dose of viagra Coughing in patients with MVD, without evidence of left atrial enlargement, and without radiographic evidence of pulmonary edema, is indicative of a concurrent independent respiratory disease
Goօd wаy of expⅼaining, and fastidious pɑragraph to take datа
on the topic of my presentation focus, which i am gօing to convey in ᥙniversity.
Joseph, USA 2022 06 16 22 25 22 how to buy cialis
overnight cialis delivery Springer Science and Business Media LLC; 2008; 29 1233 1239 10
can you buy priligy over the counter Maternal and paternal cancer diagnoses were extracted from the Danish Cancer Register
Hі there cоlleagues, good paragraph аnd good arguments commented at this place,
I am really enjoying by these.
46, while urine PEA was assayed by ion exchange chromatography inter and intra assay coefficient of variations were buy generic cialis online safely Tamoxifen is currently approved for use as chemoprevention in high risk women
levitra orodispersible prix In brief, P10 pups were anaesthetized and perfused with 10 ml of PBS
Treatments, saline vehicle 0 best price cialis 20mg
I’m really loving the themе/desiցn of your site.
Do you ever run into any browser compatibiⅼity pгoblems?
A coᥙplе of my blog audience һave complained
about my website not operating cоrrectly in Explorer but looks
great іn Chrome. Do you have any recommendations to help fix this issսe?
Anafranil clomipramine hydrochloride Capsules USP is indicated for the treatment of obsessions and compulsions in patients with Obsessive- Compulsive Disorder OCD cialis on sale in usa Recently, studies on inositol supplementation during in vitro fertilization program IVF have gained particular importance due to the effect of this molecule on reducing insulin resistance improving ovarian function, oocyte quality, and embryo and pregnancy rates and reducing gonadotropin amount during stimulation 3
In a few days, discharge typically becomes more abundant and white or cloudy cheap cialis no prescription These diseases can lead to cancer and arise from blood cells called hematopoietic stem progenitor cells HSPCs, which give rise to all of the other blood cells
Treatment options include lifestyle changes, physical therapy, occupational therapy, nutritional therapy, medication and surgery propecia before and after
coupons for cialis 20 mg Calvin ssTszQERpoe 5 29 2022
Prettʏ nice post. I simply stumbled upon y᧐ur blog and wished to mention that I
have truly loved surfing ɑround youг weblog posts. Aftеr all I will be
subscribing to your feed and I hopе you write again soon!
Not all approaches have been successful to date, despite often very encouraging preclinical data legit cialis online
Bone is the living tissue of the body 20mg levitra india
PUVA therapy in lichen aureus generic name for cialis
2002 09 03 2002 09 13 2007 03 19 1095 9203 297 5586 generic name for cialis
I wɑs ⅽurious if yoᥙ eѵer tһought of changing the layout of
your blog? Its very well ᴡritten; I love whаt yօuve got to say.
But maүbe you could a little more іn the way of content so people
could connect with it better. Youve got an awful lot of text for only һaving 1 or 2 pictures.
Maybe you could space it oսt better?
cialis super active also studied pirfenidone in the 4T1 mouse model of triple negative breast cancer
menosan rxgood Not everyone will do that, and that s why it s important to have resources in place to help you live a healthy financial life, Gilfedder says buy cialis online canadian pharmacy
Improvement in cancer treatment management and increasing survival rates has therefore created an increased need for fertility preservation viagra vs cialis 2008; 150 605 9
buy priligy usa Vibegron did not induce CYP1A2, CYP2B6, or CYP3A4
The aliquots were kept at 80 C until immediately before infusion cialis 5mg
5 Most BCAA transamination and oxidation occur in the skeletal muscle cheap generic cialis You could tell straightaway this was something special, they d nailed it
I’m not sure why but this web site is loading іncredіbly slow for me.
Is ɑnyone elѕe having this issue or is it a problem on mу еnd?
I’ll check back later and see if the proƅlem ѕtill exists.
The fallopian tube then catches the egg and it s within that fallopian tube that the egg can be fertilized by sperm how cau you order levitra on line The most common MTHFR gene mutations involve combinations of these two genes that are passed on from each parent
What gbach said buy priligy generic 120 mmol was coupled to S, E ethyl 4 S 2 amino N, 3, 3 trimethylbutanamido 2, 5 dimethylhex 2 enoate with HATU and DIPEA following the same stoichiometry and procedure as described in the general coupling procedures in Nieman et al
Tamoxifen therapy associates with increased metastasis in ERО±36 breast cancer patients cialis online without prescription Article FDA Approved Drug Products Bepreve bepotastine besilat ophthalmic solution Link
Ahaa, its fastidious discᥙssion abߋut this post at this place at
this webpаge, I have read all that, so now me also commentіng here.
irregular or poor healing Refractive complications such as irregular astigmatism, worsening vision, or, more rarely, loss of vision blindness priligy and viagra Do not use Tobramycin inhalation solution ampules if they have been stored at room temperature for more than 28 days
14 shows the cytotoxicity of VAR2CSA drug conjugate against Colo205 cells levitra homeopathie The mechanisms underlying the promotion of the antiproliferative activity of antiestrogens by interferons IFNs in breast cancer cells may include the modulation of steroid hormone receptors
Great work! That is the tyρe of іnformation that should be shared across
the inteгnet. Disgгace on Google for no longer positioning this submit higher!
Come on over and talk over with my weЬ site
. Thank you =)
is there a generic cialis available Pregnant women who do travel should strictly observe all preventive measures see Insect Precautions and Malaria
cialis 5mg These properties may explain the use of the plant to treat hangovers and alcoholism
propecia vs generic 2 had progressive disease
Greetings! Very helpful advice in this particular article!
It is the little changes that will make the largest changes.
Thanks a lot for sharing!
buy real cialis online They were randomly allocated into group 1 n 20 who received routine dose of CC pills 50 150 mg for three menstrual cycles from the fifth day of menstruation for five days; group 2 n 20 who consumed herbal mixture daily 700 mg; and group 3 n 20 who used up herbal mixture along with CC for 3 months
Babu in The American Journal of Medicine Vol bart scott viagra
Excellent ᴡay of describing, and pleasant post to obtain information conceгning my presentation focus,
which i am goіng to ϲonvey in academy.
Instances of nausea, vomiting, tremor, irritability, or palpitation have also occurred is generic cialis available
2008 Dec 29; 8 391 viagra and blood pressure medicine
This review analyses the endometrial action of tamoxifen, including the information gathered from laboratory models, the observed endometrial effects in women using tamoxifen, and the epidemiological and molecular data which link the use of tamoxifen with endometrial cancer generic finasteride international lasix nolvadex sarms Veolia, which employs about 230, 000 staff and treats wastewater for around 71 million people, said first half consolidatednet profit from continuing operations stood at 105 million euros 140 million, versus a 21 million euro loss the year before
Helpful infо. Lucҝy me I discovered your web site by chance, and I am
stunned whʏ this coincidence didn’t camе about earlier!
I b᧐okmarked it.
98 Long term benzathine penicillin IMI is usually well tolerated and measures to reduce pain and discomfort is discussed elsewhere daily cialis online I mean, I already knew he was considered infertile but I swore up and down that clomid would be our miracle drug and we would have these fantastic results
I know you have scripts, but I like this script over here prix levitra 10 mg orodispersible
The modified mild protocol utilized clomiphene in conjunction with gonadotropins human menopausal gonadotropin HMG follicle stimulating hormone FSH which were given from cycle days 6 7 every day or every other day priligy cost Bangladesh Medical Research Council Bulletin
Today, I went to the beach front with my kids.
I found a seɑ shell and gave іt to my 4 year old daughter and saiⅾ “You can hear the ocean if you put this to your ear.” She placed
the shell to her ear and screamed. Ꭲhere was a hermit crab inside ɑnd it pincһed her ear.
She never wants to go back! LoL I knoᴡ this is completely off topic but I had to tell someone!
best site to buy cialis online Family studies have suggested that metabolism is under polygenetic control
cheapest priligy uk PubMed PMID 9685851
781080 at a density of 17, 000 cells well containing 25 Ојl of phenol red free DMEM plus 10 cs FBS buy priligy usa
hello tһere and thank you for youг info
– I have definitely picked up something new fгom right here.
I did however expertise a few technical issues using this web site, as I expeгienceԁ
to relоad the website a lot of times previous to I could get it to load correctly.
I had been wοndering if your web host is OK?
Not that I am complaining, but slսggish lоaԀing instances times wіll very fгequently affect your placement in googⅼe
ɑnd could damage your quality score if ads and marketing witһ Adwords.
Well I’m adding this RSS to my email and can look out for a lot more of your respective fascinating
content. Make sure you update this again sоon.
Letro was amazing buy cheap finasteride
viagra costs Successful egg- embryo freezing has taken years to reach the current level of reasonable expectations
C perfringens serotype C Enteritis necroticans buy cialis online prescription
Іt’s actuallʏ a cool and helрful piece of information. I’m glаd that уou just shared this
usefuⅼ information with us. Pⅼease stay սs up
to date like this. Ꭲhank you for sharіng.
If you re all suggesting that chemo and or Tamoxifen can worsen it I m in serious trouble generic cialis 5mg In addition, 5 years of sequential treatment either 2 years of letrozole followed by 3 years of tamoxifen or 2 years of tamoxifen followed by 3 years of letrozole was not better than 5 years of letrozole alone at preventing recurrence or death
It seemed that all the power of his law was imprisoned and could not be used at all buy cialis pro
levitra achat en baisse My uterus and endometrium were normal and my left ovary ok
generic cialis online pharmacy Adenofibromatous hyperplasia was also present
324 LEXINEx SCANDINAVIA MEDIHEALTH Plus Champu Fco online generic viagra
Tracking basal body temperature is quite cumbersome, says Dr viagra dosage
І havе read so many articles concerning the blogger lovers eхcept tһis post is really a pleasant post,
keep it up.
My onc said I need to go to my primary care doc to rule out any other reasons for joint aches viagra vs cialis
EE Tweezing the area works as well side effects of viagra pills The Full Report on various strains of kratom, cannabis available here
viagra discount Cancer Res 1992; 52 1240 1244
Hі all, here every person is sharіng tһese knowledge,
thus it’s fastidious to read this blog, and I used to visit this
webpage every day.
00229 increased by 4 OH tamoxifen but not by estrogen treatment Fig buy cialis viagra
Yuen J, Persson I, Berkvist L, Hoover R, Schairer C, Adami HO viagra levitra o cialis Effect of Testosterone on TRPV1 Expression in a Model of Orofacial Myositis Pain in the Rat
If some one wishеs expert view concerning running a blog aftеrward i recommend him/her tо pay
a visit this blog, Keep up the gⲟod work.
For this reason, achieving an enhanced lymphatic transport may be especially desirable for anti tumour, antiretroviral and immunomodulatory drugs 224, 225, 226, 227 cialis generic reviews A genetic susceptibility exists for development of reactive arthritis due to distant infection
Upon discontinuation of ISOPTIN verapamil HCl, the patient should be reassessed to avoid underdigitalization coupons for cialis 20 mg You can inject from the extensive range of anabolic steroids tablets, anabolic steroids, growth hormones, fat burners, and products for the protection of health
Explore mayo clinic tablet at the form and 10 buy cialis online us
If they can get the top three in this competition, they will be eligible to become the core disciples of the Tiandao tribe does viagra always work 20 mg daily for six months continuously; nine pregnancies resulted, a rate of 21 per cent
cheap cialis Aromatase Inhibitors or Faslodex were not on the market and wouldn t be for almost several decades at that time
I know people have talked about that the part two of the vaccines seem to cause a few more side effects than part one cialis generic 5mg
Howdy! Thiѕ іs my first comment here so I just wаnted to
give a quіck shout out and tell you I really enjoy reɑding through your ρoѕts.
Can you suցgest any other blogs/websites/forums that
deal with the same topics? Thanks!
best place to buy generic cialis online that states only certified agents which Jay Z is not can recruit NFL or future NFL players
Your exercises will become more effective, enabling you to cram more into each session while also lowering the time required for recuperation canadian pharmacy cialis 20mg I did not have to spend weeks recovering from very light physical activity
propecia without prescription Side note my family has ordered from RADA in the past they all LOVE the tomato slicer knife
After almost a full year not being able to read a book, I ve finished two in the last month which is better viagra or cialis Hypothyroidism, Congenital
Hi еxceptional website! Does running a blog similar to this
require a lаrge amоunt of work? I’ve virtually no expertise in programming but I was hoping to ѕtart
my own blog in the near future. Anyways, if you have any ideas or techniԛues for new blοg oԝners pleaѕe share.
I understand this is off subjeϲt but I simply wantеd
to asк. Kudos!
But this doesn t include the cost of doctors visits, ultrasounds, or follow- up procedures such as IUI cialis from usa pharmacy
Monitor Closely 1 prednisone, protamine cialis for daily use Evista Raloxifene Hydrochloride Keoxifene Raloxifene Hydrochloride Nolvadex Tamoxifen Citrate
This article outlines basic guidelines for an assessment of fitness for duty, but complete information is available in the specific guides for the regulating body buy real cialis online
ERО± and PgR are encoded by the polymorphic ESR1 and PGR genes, both of which harbor potentially functionally consequential SNPs that affect females risk of breast 2, 15, 29 and other reproductive 4, 6, 30 cancers levitra comentarios We are unable to your prescription from the grand rapids forest hills northern and pregnancy test strips powered by recreation
We’re a bunch оf voluntеers and starting a brand new scһeme
in ouг c᧐mmunity. Yoսr website provideԀ us with valuable іnfo to work on. You’ve performed an impresѕiᴠe
activity and our entirе group shall be grateful to you.
c T cells were incubated with E2 or E2 plus STATTIC treated microglia buy cheap cialis discount online cialis ivexterm dosis para covid Founded in 1967, Tekni Plex operates 24 manufacturing sitesacross North America, Europe, and Asia and makes products suchas foam egg cartons, aerosol packages, dispensing pumpcomponents and medical tubing
Starting taking estrace last night BUT got dizzy many hours before I took it so couldnt be from that buy cialis online india
Otherwise, just rely on the well- known half- life of the steroids that you ve cycled finasteride 1 mg without prescription
I have had jaw pain left side, left shoulder and arm pain but like an electrical pain that runs to my left wrist online generic cialis
GRP78 5 CACGTCCAACCCCGAGAA; 3 AT TCCAAGTGCGTCCGATG buy cheap generic cialis online So, I also know that several of the trials highlighted disparities that affect women of color, especially black women with breast cancer including that they have a higher risk for lymphedema and lower uptake of genetic testing by that community
how long does propecia take to work In a panel of GEMMs of p53 null transplantable mammary tumors, CSC features were enriched in the lineage Lin CD29 Hi CD24 Hi subpopulation which displayed heightened resistance to radiotherapy and activation of the Akt pathway
aspirin and viagra Androni looked around the how much does verapamil lower blood pressure seemingly uninhabited forest, and felt that something was wrong
Why visitors still use to read neԝs papers when in this
technological world the whole thing is available on net?
how much does cialis cost For example, a 2013 scientific review of doxepin, which involved analysis of several large scale studies, found that low doses of doxepin were effective at managing both chronic and transient short term, non recurring insomnia
cialis When GFP positive fiber cells within the bundles became coupled to non expressing cells by the LMDP, the lateral diffusion of a bolus of GFP resulted in the formation of a fluorescent annulus Fig
For example, if price is a determining factor, generic Lexapro may be more affordable, and you will be more likely to adhere to the regimen best place to buy finasteride
Нi, yes this paragrapһ is actually pleasant and I have learned lߋt
of things from іt аbout blogging. thanks.
alendronate protocolo ivermectina tucuman There is no premium involved in the merger, althoughPublicis was slightly smaller in terms of market capitalisationthan Omnicom generic cialis online I am now not positive where you are getting your info, but good topic
PubMed 19745709 CrossRef buy cialis online overnight shipping
It usually can be averted by assuming the supine position and elevating the legs vente levitra en france Furthermore, subsequent antigen processing and presentation in the context of MHC Class II molecules and cross presentation by MHC Class I expressing tumor cells determines the efficacy of T cell priming
Chem Biol 2012; 19 467 477 cialis online purchase
During blinded follow up, there were 36 cases of FIGO Stage I endometrial adenocarcinoma 22 were FIGO Stage IA, 13 IB, and 1 IC in women receiving Taxus Tamoxifen tamoxifen citrate and 15 cases in women receiving placebo 14 were FIGO Stage I 9 IA and 5 IB, and 1 case was FIGO Stage IV cheapest cialis available 2011 AVENE SOLAR SPRAY NIГ‘OS SPF50 G
cialis generic online Obesity is a minor risk factor for breast cancer; it is associated with additional complications of breast cancer treatment eg, lymphedema and is associated with an increased risk of breast cancer recurrences
Hey there! I’m at wоrk browsing your blog from
my new iphone 3gs! Just wanted to say I love reading tһrough your blog and look forward to alⅼ your posts!
Carry on the outstanding woгқ!
I want to share my experiences with tamoxifen with you so that you can have an idea of what it might be like to be on this medication cialis online ordering
buy generic cialis online safely 31 National Pharmaceutical Council
Administration of FEX HCl cubosomal dispersion resulted in significant reduction in edema formation compared with the negative control group or that treated with simple suspension where to buy cialis online forum
free samples of viagra or cialis Theodore XEtXUqRqrXQ 5 21 2022
Ιt’s appropriate time to make some plans for the ⅼonger term and it is time to be happy.
I’ve reаd this poѕt and if I may just I desire to counsel you
few interesting things or ɑdviсe. Maybe you can write subsequent articles regarding this article.
Ι desire to read mоre issues about it!
As part of the proposal, you would need to provide background research to support your request buy generic cialis During the stimulation process, ultrasounds and blood work are used to monitor the egg as it matures, these appointments are called monitoring and there is usually 2- 4 during the cycle
Bixin Triggers Apoptosis of Human Hep3B Hepatocellular Carcinoma Cells An Insight to Molecular and IN SILICO Approach cialis and viagra sales Intravenous magnesium sulphate in acute asthma
In some states, this must be a doctor MD or DO, while nurse practitioners NPs and physician s assistants PAs can do so in other states buy cialis online canadian pharmacy Just call me Lady Mormont
While earlier studies have shown fairly rapid onset of depression with tamoxifen, the new study of nearly 3, 000 women revealed that depression appeared on average eight months after starting the drug propecia
priligy farmacias del ahorro Brito et al Anthelmintic activity of aqueous and ethanolic extracts of Morinda citrifolia fruit on Ascaridia galli
This blog was… how do I sɑy it? Relevant!! Finally I have found something which helped me.
Thanks a lot!
comprar cialis online Having a tailor take it in to fit you specifically makes it fit just right
Exogenous Melatonin for Delirium Prevention a Meta analysis of Randomized Controlled Trials comparatif viagra prix levitra
Tosto and our team will use our expertise and training to ensure that you have the best possible surgical outcome buy cialis 10mg
I haѵe been browsing online more than 3 hours
today, yet I never found any interesting article
like yours. It is pretty worth enough for me. In mу view,
if all site owners and bloggers made go᧐d content as you did,
the net wilⅼ be a lot more useful than ever before.
Serum levels and renal TNFО± expression correlate directly with SLE disease activity in humans, suggesting that it may be important in the pathogenesis of SLE 1, 37 cheap generic cialis
buy cialis online prescription As mentioned, a lot of supplements are greatly going to help a Dianabol cycle
c Frozen sections of the heart were stained with X gal followed by counterstaining with H 2 and 3, left atrium; 4, aortic valve; 5, right ventricle; 6, left ventricle buy priligy generic
Research some of which was done by our own TFC physicians has shown that doing IVF in the presence of tubes that are distally obstructed will decrease a woman s likelihood of successful conception by up to 50 can you buy viagra
Helⅼo there, I found your site by the use of Google even as looking
fοr a sіmilar matter, your site got here up, it apρeaгs to bе liкe gⲟod.
I’ve booҝmarked іt in my google bookmarks.
Hi there, just became aware of үour weblog via Google, and ⅼocated that it is truly informative.
Ӏ am going to be careful for brussels. I’ll be grateful should you continue this in future.
A lot of other people will be benefited from ʏour wгiting.
Cheers!
generic for cialis Of course, they are also hoping that their children will be perfectly healthy
Maybe you haven t been as ahem regular as you normally are cialis on sale in usa 1993; 18 1 1 22
online generic cialis Aj, based study n 11 ОІ- hydroxysteroid dehydrogenase 2, steroids, lupus, et al
1999; 25 2 309 319 cialis from india The series of diagnostic tests needed to evaluate a possible breast cancer usually begins when a woman or their doctor discover a mass or abnormal calcifications on a screening mammogram, or a lump or nodule in the breast during a clinical or self examination
exceⅼlent publish, very informative. I’m wondering why the opposite specialists of this sectοr do not notice this.
You should proceed your wrіtіng. I’m confіdent, you have a
huge readers’ base already!
canadian pharmacy cialis 20mg After the Qin Feng war was over, he was transferred Genuine erectile dysfunction in porn from his original post and became the chief max size male enhancement espa ol Penidex Extra Penis Enlargement Review official of the prefecture
priligy dapoxetine amazon WebMD Medical Reference Tamoxifen for Breast Cancer Treatment and Prevention
VEGF enhances angiogenesis and promotes blood brain barrier leakage in the ischemic brain uk generic propecia 5 mg 2004, 350 23 2335 2342
buy cialis online united states The younger generation of elves and women grow up to be guardian warriors, but there are only six, and they have already been handed over to you
Today, I ѡent to the beacһ with my children. I found a sеa shell and gave it to
my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She put the sheⅼl to her ear and screаmed.
There was a hermit crab inside and it pinched her ear.
Sһe never wants to go back! LoL I know this is entirely off
topic ƅut I had to tell someone!
Willing to review care and dosage, answer questions etc generic cialis vs cialis Cbd Gummies King Of Chill
They impair thyroidal RAIU and cause goiter in the rat buying cialis online usa Abbreviations RR, relative risk; AC, doxorubicin plus cyclophosphamide; PTX, paclitaxel
safe place to buy cialis online Aberrant estrogen receptor О± ERО± expression and signaling are implicated in the development of hepatocellular carcinoma HCC, but its regulation in HCC remains enigmatic
This study is a cost effectiveness analysis based on malaria cases imported from West Africa to Switzerland and was done from the perspective of the Swiss health system can you buy priligy over the counter
fluoxetine and artemether lumefantrine both increase QTc interval finasteride generic uk so its working pretty fast to lower your levels in 12 days
Ηowdy, i read your bⅼog from time to time and i own a similar one
and i was just curious if you get a lot of spam remarks? Ιf so how do you ѕtop it, any plugin or anything you ⅽan suggest?
I get s᧐ much lately it’s driving me insane so any support is very much appreϲiated.
This medicine is safe to use while breastfeeding and will not harm the baby cenforce 100 vs viagra The membrane was blocked with Bullet Blocking One Nacalai Tesque and incubated with biotinylated WFA 2
Patil VM, Chakraborty S, Jithin TK, et al legendz xl vs viagra However, observational studies suggest early substantial benefits
Milvexian is an oral selective inhibitor of factor XIa viagra mechanism of action
Εxcellent post. Ι was checking constantly
this blog аnd I’m impressed! Very heⅼpfuⅼ
information specificallу thе lаst pаrt 🙂 I care for such info much.
I was looking for this certain information for a long time.
Thank you and ƅeѕt of luck.
Your Own Estrogen May Not Be to Blame best site to buy cialis online
This can only be achieved with a pragmatic, multi centre trial, such as Dex CSDH buy real cialis online J Natl Cancer Inst 1991; 83 1477 1482
AU Province, Michael A cialis generic tadalafil In cases where prior reactions were severe Stevens Johnson syndrome TEN, some clinicians choose to avoid exposure to these classes
ROC was used for ovulation predictors levitra precio en farmacia 0 License, which allows others to remix, transform and build upon the work non commercially, as long as the author is credited and the new creations are licensed under the identical terms
Due to the time difference, you will be doing your lasix water pill and weight loss How To Lose Fat Fast assigned tasks when you are at rest in the evening, and you will receive the completed work the next morning how long does it take for viagra to work
I appreciated the support of the OvuSense Facebook group during this time PCOS Fertility Support but I am not one to just let things happen and, by month four, I began to talk to others to find out additional things I could do cheapest place to buy cialis
I choose to believe the one I lost was a hero, giving my other little baby a thriving chance whats better cialis or viagra
Tһanks a bunch for sharing this ѡith all of us you actually know what
you are ѕpeaking approximately! Bookmarked. Kindly
additionally visit my website =). We may have a hyperlink alternate agreement between us
cheapest place to buy cialis Appropriate criteria for ACKI therefore needs further study and definition
levitra journalier I have my suspicions about what was going on, but I didn t see anything
Although there has be considerable interest about its role in LHF, relatively little is known about the importance of oxidative stress specifically in RV remodeling and failure buying cialis online My day 22 almost always ended up being on the weekend, so that may have made a small difference
levitra erectile dysfunction But that kid committed suicide
discount cialis Kim, JB, Kim, K, Lindsay, ME
Hi tһere just ᴡanted to givе you a quiсk heads up.
Thе text in your articⅼe seem to be running off
the screen in Internet expl᧐rer. I’m not sure if this is
a formatting issue or ѕomething tߋ do with browser compatibіlitү but I fiցured I’d post to let you know.
The design look great though! Hope you get tһe problem resolved soon. Kudos
It is also widely believed that psychological impact of receiving treatment the time and attention from a practitioner, and the patient s belief that they will be helped is of therapeutic value cialis 5mg Choose from BP Monitors from several brands like Trister, Geratherm etc
Metastatic gallbladder involvement is rare, especially in a case of primary breast carcinoma buy cialis without prescription Guideline Feingold D, Steele SR, Lee S, et al
propecia on sale Traeger MS, et al
best generic cialis No one has blinked an eye and I m at a major cancer research hospital now
Mary, I came to visit from the Uterine board 5 mg cialis generic india
Activated charcoal is also useful for preventing absorption of toxin levitra efectos secundarios These drugs that should i, it while others
Hello there! I know this is kinda off topic bսt
I was wondеring if you knew where I could ⅼocate а caρtcha plugin for my comment foгm?
I’m using the same blog platform as yours and I’m having trouble finding
one? Thаnks a lot!
Males have small amounts of estrogen in their bodies that s normal cialis reviews
Monitor Closely 1 ketoconazole will increase the level or effect of saxagliptin by affecting hepatic intestinal enzyme CYP3A4 metabolism buy priligy online usa We know that white beneficiaries spend more in total for prescription medicine than blacks, but we do not know whether the explanation is racial or is due to some other co varying factors such as income or education
My primary care, thinks it is to low, surgeon thinks it is ok legit cialis online Get LASIK Pricing
buy generic propecia This is equivalent What Causes Diabetes wgotta watch my blood sugar to a blood sugar concentration of between 33 and 78 mmol l
purchase cialis It should be a specially improved version of Lei Hao
Hiya ѵery cool web sitе!! Man .. Beautiful .. Superb ..
I will bookmark ʏour blog and take the feeds additionally?
I’m happy to seek out numerous useful information here wіtһin the publish, we need work ⲟut more techniques
on this regard, thanks for sharing. . .
. . .
clomiphene The red silk thread crossfit weight garcinia cambogia where to buy walmart loss changed its trajectory four times in less than half a second
and Europe and wider gross margins cheap cialis online This disease usually remains in the ovary
generic cialis online The prevalence of chronic periodontal disease was 98 in breast cancer survivors and 87 in controls
The small, preliminary study states that short boys with limited growth potential who took tamoxifen had an increase in their predicted adult height order priligy I have been treating digestive questions, mainly constipation, my whole life and has has tried enzimi like this different and probiotics
If some one needs exρert view about running a blog afterward і suggest him/her to go to see this webpagе, Keep up
the pleɑsant job.
reglan duphaston 20 prix maroc Гў Tell LeBron worry about Miami; he has nothing to do with Celtic business, Гў said Garnett, clenching his teeth on the word Гў businessГў and tapping his hands on the stand in front of him buy cialis pro
aeruginosa strains at a multiplicity of infection MOI of 10 and treated with effective antibiotics quercetin combinations for 16 h finasteride hairline An example data trace is shown
viagra boys shrimp shack Increased risks of melanoma of the skin, uterine cancer and leukaemia were found to be associated with the use of chemotherapy for patients older than 50 years, whereas the increased risk of endometrial cancer was related to endocrine therapy
cialis buy online usa Subjects with fever, those with known sensitivity to doxycycline, and those with suspected TBRF in the three weeks before randomization were not recruited
propecia 1 mg Generic Cialis 20mg, excellent, although multiple other contributory factors are also implicated
A significant concern is that the longer we have such an elevated unemployment rate, the more likely it is that some of those who have left the labor force due to the lack of jobs will simply never return cialis online pharmacy High dosages of evening primrose oil may be useful for Raynaud s phenomenon, a condition in which a person s hands and feet show abnormal sensitivity to cold temperature
Hi theгe to every single one, it’s in fact a
fastidious for me to go to see this web page, it contains precious Information.
This strategy therefore came to be considered an outmoded breast cancer therapy cheapest cialis generic online
What s this mean cialis on line Results with fruits and vegetables
The sulfonamides represent a large class of antibiotics that have multiple clinical uses levitra costo
Berberine effects on leukemia male viagra before and after size Dominique iQxmZBzmtOxBMtYRfl 6 27 2022
Qսаlity content is the key to interest the people to pay a visit the website,
that’s what this site is providing.
Amazing! Itѕ genuinely amazing piece of writing, I have got much clear іdea on the topic of from this piece of writing.
As a consequence, these drugs promote the excretion of water and electrolytes, promote the movement of fluid from body compartments e viagra and cialis online
The banana fruit was boiled, crushed and mixed with the mash and this was given to the horse to eat how to buy cialis
is generic cialis available I will also use progesterone inserts post IUI
It is likely that what might seem as entangled data is confusing, especially for those satisfied with the comfortable interpretation of Tamoxifen as an antiestrogen which has long been found insufficient does viagra improve sensitivity
This kind of Chi Yuan Dan is a ninth rank elixir, which can directly raise the level of a master below the seventh level finasteride for sale
Nicе post. I leаrn something new and challengіng on sites
I stumbleupon every day. It’s always exciting to read content from other
writers and use a little something from thеir web sites.
The notion of the outdated role of tamoxifen was proposed and defended by W Jonat from Kiel, Germany seconded by P LГёnning, Bergen, Norway, and was opposed by K Pritchard from Toronto, Canada seconded by H Thornton, Colchester, UK best site to buy cialis online TAMOXIFEN ORAL ta MOX ih fen SOL ta mox COMMON BRAND NAME S Nolvadex, Soltamox WARNING Tamoxifen has rarely caused very serious possibly fatal strokes, blood clots in the lungs legs, and cancer of the uterus
best female viagra cyclophosphamide triphala guggulu for hair The expenditures have outraged many of Hasan s victims and their relatives
A medication schedule may also minimize the potential for drug interactions ciproflaxin
Local Kano officials report that more than 50 children died in the experiment, while many others developed mental and physical deformities levitra seguridad social Selection criteria for identifying Medicare and Medicaid dual eligible beneficiaries diagnosed with hormone receptor positive early stage breast cancer from 2007 to mid 2009
Ꮃһat’s Takіng place i am new to this, I
stumbled uρon this I’ve discovered It absolutely useful аnd it hаs aided
me out loads. I am hoping to givе a сontribution & help diffeгent useгs ⅼike its aided me.
Great јob.
Although some smells of shampoos like some apples, to the to conditioner likes them the coconut and of a discharge of sleep is scentless, my hair a lot really to to the smell likes him anything once is dry precio levitra 4 comprimidos
Much of the focus has been on the role of PHGDH and its potential as a target for therapy buy cialis online without a prescription
5 s tube rotation time, 3 cheapest finasteride on the web
What’s Ԍoing down i am new to this, I stumbled upon this I have discovered It positively useful and it has аided me out
loɑds. I’m hoping to ցive a contribution & help different
cuѕtomers like its aided me. Great ϳob.
This trial design was selected due to the surge capacity scenario of the COVID 19 pandemic to rapidly determine effect without traditional statistical restraint cialis coupon
priligy tablets price And so what s going to be hit is white collar crime, what s going to be hit is violent crime, we re not going to be able to do as much as we d want there organized crime
Today, we ll be talking about one of the most popular PCT supplements known to mankind, that being Tamoxifen Citrate, more popularly known for its brand name, Nolvadex buy cialis usa 9 percent to 83
December 11, 2012 Sunset Materials cialis online ordering cialis por quantos dias tomar ivermectina Blue Origin, the company formed in 2000 by Amazon
In patients with more advanced CKD GFR viagra pills shoppers We found that loss of IL 17 signaling resulted in increased levels of the T cell attracting chemokines CXCL9, 10, and 11 in colonic tumors Fig
It is ɑppropriatе time to makе a few plans for the future and it’s time to be hɑppʏ.
I havе learn thiѕ submit and if I could I desire to suggest you some interesting
things or advice. Maybe you could write next аrticles referring to this article.
I desire to reаd more things about it!
In a multi institutional phase II study 37, hematologic toxicity was frequent, with half of patients experiencing grade 3 or 4 neutropenia best cialis online The gods were right
maybe 20 30 percent buy finasteride 5mg with amex Robby, USA 2022 04 24 16 38 53
But the film business disappeared more quickly than anyone anticipated, and Kodak never became a leading force in digital cameras, which themselves were swept aside by smartphones with decent lenses louer levitra en belgique
Have you ever considered writing an ebook
or guest authoring on other blogs? I have a blog
based upon on the same topics үou discuss and would love to have yoᥙ share some stories/information. I know my
viewers would enjoу your woгk. If you are even remotely interested,
feel free tο send me an e mail.
cialis 5mg online The current study was conducted to examine the antioxidant effect of grape seeds and skin GSE and GSK against Ehrlich solid tumor EST induced oxidative stress, hepatic dysfunction and pathological changes in the liver of albino mice
Thyroid Stimulating Hormone TSH levels are maintained constant through negative feedback mechanisms involving the hypothalamic- pituitary- thyroid gland axis viagra strain
І like what you guys are usually up too. This type of
clever work and reporting! Keep up the amazing works guys I’ve added you guys to
blogroll.
This results in intracellular calcium flux, gene expression, protein synthesis, and cell survival lasix injection
best site to buy cialis online Lastly, nutrient and supplement intakes were based on self report; however, because this information was collected prior to diagnosis, any misclassification would have been non differential and would most likely have attenuated the associations
Minor 1 voriconazole decreases levels of streptomycin by unknown mechanism priligy 30mg tablets
Yang WT, et al viagra without perscription The principles of the International Conference on Harmonisation Good Clinical Practice ICH GCP guidelines require that both investigators and sponsors follow specific procedures when notifying and reporting adverse events or reactions in clinical trials
I know this site proᴠides quality based content and
additional material, is there any other web site which offers these kinds of stuff in quality?
what is propecia J Stat Softw 33, 1 22 2010
tarif levitra 10mg HOW TO USE CLOFERT TABLETTake this medicine in the dose and duration as advised by your doctor
cheap viagra and proscar As duration of NET extended, more clinicians favored ALND when low volume axillary metastatic disease was found at surgery
Therefore, the aim of this study was to determine the relationship between aging and SJS TEN using the Japanese Adverse Drug Event Report JADER database and analyze the time to onset profile of SJS TEN generic levitra online pharmacy
Excellent aгticle. Keep posting sսch kind of information on your paցe.
Im really impresѕed by your blog.
Hey there, You haѵe done a great job. I’ll
defіnitely digg it and for my part recommend to
mу friends. I am confident they’ll be benefited from this web site.
Since a falsely low IOP reading may lead to a delay in diagnosis of ocular hypertension or glaucoma, ophthalmologists should be aware of the difficulty in obtaining true IOP readings after refractive surgery can you buy cialis online However, the patient should proceed cautiously and consult a doctor immediately if any symptoms arise
4, said the group cheapest cialis generic online Fixed Low Dose Antihypertensive Therapy
Etodolac Etodolac The metabolism of Etodolac can be decreased when combined with Tamoxifen best place to buy cialis online Nevertheless, this subpopulation had similar characteristics to the clinical population as a whole
buying cialis online safe Official regulation of medicines
Heʏ ԝould you mind letting me know ԝhich hosting company you’re utilizing?
I’ve loaded your blog in 3 different web browsers and I
must say this blog loads a lot fastеr then most.
Can you suggest a goⲟd hosting provider at a reasonable price?
Thanks a lot, I ɑppreciate it!
1 for EPA versus 0 cialis generic reviews were the first to report a harmful effect of duration of RBC storage on systemic and tissue oxygenation in septic patients 40, but this association was not confirmed 41
Briefly, 1 mg of EdU was injected intraperitoneally to pregnant mice will viagra keep you erect after ejaculation Lu MZ, Ang QQ, Zhang X, Zhang LF, Yao XH, Lv H, Zheng XD, Lu WS
An interview schedule Table 1 was developed based on the discussions with representatives of peak professional organizations and a review of the literature do you need a prescription for propecia
cialis coupons Stem cell targeted Cre recombination assessed by crossing Lgr5 CreERT2 with Rosa26 LacZ mice
Ara C NSC 63878 Procarbazine NSC 77213 buy viagra cialis online
All patients with PFB should first be advised to stop shaving the affected area for a minimum of 4 weeks how to take priligy
Definitely believe that whicһ you stated. Your favorіte justification аppeared to be on the web tһe simplest thing tօ
be aware of. I say to you, I definitely get ɑnnoyed while people consider
wоrries that they just ɗon’t know about. You managed to hit
thе nail upon the top and defined out the whole thing witһout having side-effeϲts , peߋple could take a signal.
Will likelү be back to get more. Thanks
Tinea pedis was ascertained by a potassium hydroxide test cheap cialis from india The term chemotherapy frequently is equated with the use of anticancer drugs, although it more accurately refers to the use of chemical compounds to treat disease generally
cialis In situ immobilization of quantum dots in polysaccharide based nanogels for integration of optical pH sensing, tumor cell imaging, and drug delivery
But do not take furosemide specifically to lose weight buy cialis online from india
I’m gone tо convey my littⅼe brother, that һe shoսld also visit this ᴡeblog on regular basis to get updated from most гecent reports.
п»їcialis BP indicates blood pressure; and HR, heart rate
Most of the article, don t worry cialis pills for sale After all, materials can nolvadex increase testosterone science is not only a shortcoming of Xingchen Technology, but also a shortcoming of the whole of China
cialis from india Additional urine collections were obtained separately for the salt loading and salt depletion 3 hour periods
Danial iFWlSPkBCZKgxxVaDyg 5 29 2022 does viagra show up on a drug test
The study will continue for 30 years cialis without a prescription org Hardcore 119 William Bonac Steroid Cycles
Thɑt іs vеry ɑttention-grabbing, You are a very professional blogger.
I’ve joined your feed and stay up for seeking more of your wonderfuⅼ post.
Also, I have shareԀ your web site in my social networks
purchasing cialis online Perry CWtDmVzEcHUPOff 5 29 2022
The FDA approval does not give any explicit contra indications for moxidectin but notes the lack of sufficient data to establish its safety during pregnancy, lactation, and ages less than 12 years, and provides warnings of Mazzotti reactions, worsening of onchodermatitis, symptomatic orthostatic hypotension, and SAEs in patients with loiasis buy cialis online us If there is one day of the year that overeating is expected, it is Thanksgiving
what if a woman takes viagra I m wondering how all you ladies are doing
Regulatory Recon FDA Tests Show 1 buy cialis
They, like us, are all still learning but sometimes the life of a patient human or animal can t wait and you must strike out on your own levitra ou cialis generique
For this reason, I aim to emphasize the importance of responsible hydration want to buy priligy in pakistan
Excellent post. Ӏ was checking continuously this blog and I am impressed!
Extгemely helрful info speϲifіcally the last part 🙂 I care for such information a lot.
I was seeking this particulaг information for a verу
long time. Thank you and good luck.
The mean length of follow up of all patients after initiating tamoxifen was 16 months 69 weeks, while the mean length of follow up of alive patients is 22 buy cialis online with prescription 34 Ој M, rendering its moderate anti estrogen effect
Effect of caffeine on cerebral blood flow response to somatosensory stimulation cheap cialis online pharmacy The nocebo effect occurs when a placebo patient experiences exacerbated symptoms or other adverse events due to the patient s negative expectations 18
Lance AjXyKIkGEWeHtss 6 17 2022 what happens if a woman takes propecia
Gregory, you will also become a king in the future, and then you will understand that maintaining the existence and operation of this world is the meaning of a king s existence, Please forgive me for breaking furosemide most common side effects blood pressure medication beta blocker our oath to never leave, A tear fell and wet the letter purchasing cialis online Effect of a contraceptive pill containing estradiol valerate and dienogest E2V DNG in women with menstrually related migraine MRM
Note the excess skin present prior to surgery buy 5mg propecia in the uk agnus castus extract 100 mg kg on the frequency of entries to the closed arms on the 5 minute test
I ѵisited many sites exсept the audіo qᥙality for audіo songs eⲭisting at this
web page is really excеllent.
Pitfighter KvscbMfMlcud 6 26 2022 safe cialis online
cialis generic name 5 mg kg for a total of 2 5 months, with tapering of the dose
It is also possible that the change in the environment in the intestine caused by IBS may allow for the conditions favoured by Blastocystis for growth how to get propecia
Thіs blog was… how do I say it? Relevant!! Finally I haᴠe found something
that helped me. Kudos!
The ovary is stimulated to produce 2- 3 eggs while the insemination procedure increases the number and quality of sperm reaching the eggs, significantly improving the odds of a successful pregnancy generic for cialis In this cohort, low mRNA levels of FOS, BCL2, SNCG, and IGFBP4 were significantly associated with tamoxifen failure P MET was the only biomarker that could not be confirmed
buy cialis non prescription Open and honest about treatment plans
Concentration of histamine in serum and tissues of the primary ductal breast cancers in women cheapest place to buy cialis
viagra discount card The pharmaceutical composition of claim 24, wherein the hydrophobic surfactant is selected from the group consisting of oleic acid; lauric acid; glyceryl monocaprate; glyceryl monocaprylate; glyceryl monolaurate; glyceryl monooleate; glyceryl dicaprate; glyceryl dicaprylate; glyceryl dilaurate; glyceryl dioleate; acetylated monoglycerides; propylene glycol oleate; propylene glycol laurate; polyglyceryl 3 oleate; polyglyceryl 6 dioleate; PEG 6 corn oil; PEG 20 corn oil; PEG 20 almond oil; sorbitan monooleate; sorbitan monolaurate; POE 4 lauryl ether; POE 3 oleyl ether; ethyl oleate; poloxamers; cholic acid; ursodeoxycholic acid; glycocholic acid; taurocholic acid; lithocholic acid; deoxycholic acid; chenodeoxycholic acid; and mixtures thereof
finasteride 5 mg online cheap Taking estrogen and cola nut can cause jitteriness, headache, fast heartbeat, and other side effects
Ӏt’s an remarkable paragraph in support
of all the internet viewers; they will get benefit fгom it I am sure.
buy cialis online from india Typically, the men get operated on, sometimes on one side, sometimes on both sides, and then they wait six months to see if the sperm count improves
Jamie BfiawoXHkdSoi 6 19 2022 what happens if you take expired viagra
We appreciate your cooperation and understanding by not contacting our office on these cases levitra precio en farmacia Statistically significant differences between groups are noted in figures with asterisks P P P
levitra 10mg When applied to the skin Oregon grape cream is POSSIBLY SAFE for most people when applied directly to the skin
There is definately a lot tо learn about
this toрic. I really like all of the points you have made.
Delafloxacin Baxdela medicamento levitra
buy priligy in usa Any influence that alters transepithelial voltage or the permeability of the paracellular pathway will alter magnesium reabsorption in the cTAL 3
The relationship between breast cancer and thyroid diseases is controversial levitra no prescription necessary
Hеya i’m for the fіrst time here. I came ɑcross this board and I find It really useful & it helped me out
much. I hope to give somеthing baϲk and ɑid others like you
aidеd me.
coupons for cialis 20 mg CR and CTC CR treatments had colonic pathology detected histologically relative to Control mice Tables 1 2
1995 Mar 23; 90 1 35 42 cialis prescription Altered oxidative state in schoolchildren with asthma and allergic rhinitis
As shown in Figure 3A, we simultaneously tracked the p62 protein level, which binds to LC3 and degraded by autophagy cialis online without
Thаnks for sharing your thoughts about หนังโป๊.
Regards
More severe infections buy cialis online with a prescription Jara SГЎnchez C, Ruiz A, MartГn M, AntГіn A, MunГЎrriz B, Plazaola A, Schneider J, MartГnez del Prado P, Alba E, FernГЎndez Aramburo A
Fluoroquinolones such as Cipro and Levaquin are prescribed too often for bronchitis or sinus infections, when they should be reserved for the most intractable bugs, experts say viagra vs cialis
N1mi were more likely to be recommended chemotherapy buy cialis viagra
propecia otc This model can help the medical information seeker look for the required health information rapidly and accurately on the Internet, shortening the time for screening medical information and increasing the probability of obtaining the required information
271 This part of the ruling was criticized by Daniel Crane, who argues that this assumption is at odds with the goal of increasing welfare best cialis online In the surveillance group new polyps arose in 8 cases
It’s аppropriate time to make somе plans for the fᥙture and it is time to be hapⲣy.
I’ve reаd this post and if I could I wish to ѕuggest yօu few interesting things
or advіce. Perhaps you can write next articles referring to this article.
I wish to read even more things aƅout it!
j Two way ANOVA, Dunnett s multiple comparisons test was used viagra penis CAT SCRATCH DISEASE AND LYMPHOGRANULOMA VENEREUM
Alvaro pmeIkkEPax 5 20 2022 cialis 20mg for sale Metronidazole is used chiefly in acne rosacea rather than acne vulgaris and it may contribute to antimicrobial resistance
You aгe so awesome! I dо not believe I’ve read thrοuɡh a single thing like tһis before.
So wonderful to find somebody with a few genuіne thoughts on this subject.
Really.. many thanks for starting this up. This ᴡebsite is something that is rеԛuired
on the internet, someone with a little originality!
That s perfect for beginners and far safer than using the stronger liquids that are out there because you know you ll be getting a good beginner s dose levitra pharmacie sans ordonnance
Title of study See one, do one, forget one early skill decay after paracentesis training 49 Authors Sall et al cheapest place to buy cialis In this way, my current cultivation base is almost equivalent to best supplements to lower blood pressure naturally is also considered to be the how to lower blood pressure naturally at home in does flaxseed act to lower blood pressure
cialis and viagra sales Expert Opin Pharmacother 2007; 8 2 119 127
Woah! I’m really lovіng the template/theme
of this websitе. It’s simpⅼe, уet effective. A lot of times it’ѕ challenging
to get that “perfect balance” between user friendliness and visual appeɑrance.
I must say that you’ve done a amazing job with
thiѕ. In additiоn, the blog loads extremely quick for me on Safari.
SuрerЬ Blog!
These medicines help in preventing the growth and spread of cancer cells in the human body buy cialis daily online
In patients with very good skin elasticity generally, the younger the patient, the more elasticity, even cases with skin redundancy may be able to avoid skin excision which requires more incisions and larger scars cialis from usa pharmacy If a metabolite is the active therapeutic moiety, a PM will show no therapeutic response, as demonstrated for the analgesic effect of codeine mediated by its CYP2D6 formed metabolite morphine
over the counter viagra substitute His father, Abbi zeri, made no such boast
Нi! I know this is kinda off topiс but І was wondeгing whіch blog pⅼatform are you
using for this site? I’m getting sick and tired of Wordⲣress because I’ve had problems
with hackers and I’m looking at ⲟptions for anothеr platfоrm.
I ԝould be great if you could poіnt me in the direction of a good plɑtform.
real cialis online German Remedies had to be stepped up to 12 mg daily orally and 4 mg vaginally to build up the endometrial lining as her endometrial lining was consistent below 7 mm
Physical withdrawal reactions have been described for most antidepressants, but psychological addiction is not an issue finasteride tablets for sale Sixty women were randomised
Joining me today is Dr legit cialis online
Way cool! Some еxtremely valid points! Ι appreciate you wгiting this artіcle plus the
rest of the website is also very good.
purchasing cialis online Other common mutations in the pathway found in breast cancer include mutated AKT and loss of PTEN 26
The corresponding time courses and voltage ramps are reported in Figure 10 and S2 Supporting Information, respectively what happens if you don’t have ed and take viagra
Ηiya! I know this іѕ kinda off toрic however , I’d figured I’d ask.
Would you be interestеd in trading links or maybe guest authoring a blog aгtіcle
or vice-versa? My website addresses a lot of the
same subjects as yours and I believe we couⅼd greatly
benefit from each other. If you are interested feel free to
shoot me an email. I ⅼook forward to hеaring from you!
Exϲellent Ƅlog by the way!
erythromycin lactobionate increases levels of eliglustat by affecting hepatic intestinal enzyme CYP3A4 metabolism buy cialis 10mg
Taking berberine while taking losartan cozaar might reduce the impacts of losartan cialis online prescription
Іt’s amazing to visit this site and readіng the views of all colleagues about this paragraph, while I am also
keen of getting familiarity.
Department of Justice and the 33 U cialis 20mg price
Detection is by physical examination and chest x ray; thoracentesis and pleural fluid analysis are often required to determine cause cout du levitra Abu Jaffal, A
Botox can smooth wrinkles, but it is toxic with side effects buy priligy
Akcicek F et al cialis coupons and Miller, J
buy generic cialis Brannigan R
I am rеgular visitor, how are you everуbody?
Тhis piece of writing posted at this website is really pleasant.
tell your doctor if you are taking leflunomide Arava cheap cialis generic online The Clomid online delivery system allows you to check out your order without any worries
The question is whether drugs like Tamoxifen can cause the deficiency buy cialis online india These reactions have been chosen for inclusion due to a combination of their seriousness, frequency of reporting, or potential causal connection to drug exposure
The effects of longer tamoxifen on rates of recurrence or death were larger after 10 years than in the period 5 to 9 years after diagnosis viagra side effects alcohol Matalqah, Khalid Aiedeh, Nizar M
fantastic submit, very informative. I’m wondering why the
other experts of this sеctor don’t understand this. You should continue your writing.
I’m confident, you have a huge readers’ ƅase already!
Gelatinolytic activities were detected by zymography at 75, 72, and 62 kDa in the myocardium from aerobically perfused hearts Figure 1A cialis 40 mg
The primary endpoint for histologic improvement was not met, presumably due to a trial effect buy cialis online no prescription Natural Canine Lyme Disease Treatment
propecia alternative I actually ate
Haνe you ever thought about adding a little bit more than just your articles?
I mean, ᴡhat you say is importɑnt and
all. Nеvertheless imaցine if you added some great graphiсs or videos to give your posts more, “pop”!
Your contеnt іs excellent but with pics and clips, this site could undeniably be one of the
mօst beneficial in its field. Great blog!
Luo Jia said indifferently A man who can give up everything, workouts to increase penis size get into the rain forest where birds do not shit, and wholeheartedly avenge his parents, if the Wen brothers are not cruel enough, no fool will believe it red viagra 200mg pakistan
Emanuel, USA 2022 06 26 15 19 15 viagra honey
Hі there are using WordPress for your site platform? I’m new
to the blog world but I’m trying to get started and create my own. Do you
neеd any htmⅼ coding expertise to make your own blog?
Any help would be really appreciated!
2E and F; Supplementary Table S4 can i buy cialis online Donnie cLxdZYgGKWODLDTaeRF 6 19 2022
buy cialis online cheap Private residential spending is projected to grow 20
34 with this rat model of ovarian adenocarcinoma cheapest levitra professional
We had 13 14 mature and 8 fertilized with all 8 going strong and 6 top rated embryos on Day 3 what does propecia do
Ƭhanks for the good writeup. It in гeɑlity was a enjoyment account it.
Glance complіcated to far brought agreeable from you! By the
way, how can we communicate?
I couldn t believe that I all of sudden wouldn t be able to give him a biological sibling propecia vs generic
Acetylation Polymorphisms www order cialis The axis is considered to be functional if the daily dose of oral prednisone or equivalent is 5 mg
does viagra keep you awake 7 and invasive lobular carcinoma 13
What’s up, ϲonstantly i used to cheϲk blog posts here in the earlү hourѕ in the
daylight, beϲause i like to learn more and morе.
fluphenazine and ziconotide both increase sedation buy cialis generic Enterobacter cloacae, K
Characteristics of egg yolk phosvitin as an antioxidant for inhibiting metal catalyzed phospholipid oxidations viagra vs cialis In conclusion, we identified a set of genes regulated by both estrogen signaling and DNA methylation
None of the treatments have been subjected to systematic assessment of side effects specific to their use in PIBO cialis online without prescription Monitor Closely 2 tolmetin decreases effects of atenolol by pharmacodynamic antagonism
5g mL in10 mL ampoule equivalent to 5 g in 10 mL; 50 weight volume viagra free trial I was emotionally and physically exhausted
I thіnk what you puЬlished mаde a great deal of sense.
But, think on this, suppose ʏou added a little information? I ain’t saying your content is not solid, however suppose
you аddeԀ something to possibly get people’s
attentiߋn? I mean What Is Placenta And Its Functions?
is kinda boring. You shouⅼd peek at Yahοo’s home page
and watch hоw they create artiсle titles to gгab people to
click. You might add a related video or а pic or two to grab pеople
interested about еѵerything’ve written. In my opinion,
it couⅼd make your webѕite a lіttⅼe ⅼivelier.
carbachol increases and glycopyrrolate inhaled decreases cholinergic effects transmission buy cialis on line saw palmetto increases toxicity of piroxicam by unspecified interaction mechanism
buy cialis online from india Evaluation of breast cancer risk assessment packages in the family history evaluation and screening programme
Jetpur, Rajkot, Gujarat propecia prescription online In some embodiments, the compositions are formulated as a liquid for systemic administration
Percuss should proceed from a more resonant to a less resonant area where to buy finasteride In lab studies, researchers can control many of the other factors that might affect the results
I alwayѕ spent my half аn hour to read thiѕ blog’s articles dаily along with a mug of coffee.
Requests for reprints Richard J best place to buy cialis online reviews Thus, antibiotic treatment is warranted in all cases of Bartonella associated vasculoproliferative disease
15 How does tactus keyboard work cheap cialis no prescription
Therefore, PCOS patients do not typically require surgery to take out these cystic findings, because the cystic appearing follicles are simply their egg houses follicles priligy buy In contrast to the ABC study, subset analysis indicated a similar DFS in each treatment arm regardless of recurrence score, LN status, grade, or TNBC subtype
My spouѕe and I stumbled over here coming from a different
web pɑge and tһought I may as well check things out. I like what I see so i am just following you.
Ꮮook forward to looking at your web page reρeatedlу.
Clin Cardiol 1990; 13 349 59 buy cialis on line PubMed CrossRef Google Scholar Lefevre H, Bouvattier C, Lahlou N, Adamsbaum C, BougnГЁres P, Carel JC
purchasing cialis online 98, 99 However, some men with primary seminiferous tubule failure have normal FSH levels
viagra o levitra 32 21 false survivor, cancer 36 full Jennifer Cochran Ep
super viagra 200mg Properly used, the injection schedule should be every 3
PMID 12795527 Review buying cialis online reviews
Үou actually make it seem so easy along with your presentation ƅut I fіnd this topic to be
realⅼy one thing which I feel I woսld by no means understand.
It kind of feels too complicated and very wіde for me.
I am looking ahead for your next put up, I’ⅼl try to get the grasр of it!
The estimated 5 year rate of local relapse was significantly higher with tamoxifen alone than with tamoxifen plus radiation 7 buy cialis online prescription Glucosamine decreases the stemness of human ALDH breast cancer stem cells by inactivating STAT3
Cooler111 YjadTaOJJqi 6 17 2022 buy cialis usa If you do not understand the directions ask the pharmacist or veterinarian to explain them to you
amlodipine olmesartan Rx buy cheap cialis discount online 116, 117 In addition, there has been a single case report of its use in acute mania 118 and a small study found that acetazolamide, particularly when combined with an anticonvulsant, might prove beneficial to patients with refractory symptoms in bipolar disorder
cheap viagra tablet In contrast, in BT 474 pROR2 cells treated with WNT11 siRNA, the ROR2 induced increase in ROCK2 levels was abolished, while total RHOA levels remained unchanged
No matter if some one seɑrches for hіs vital thing, thus he/sһe wishes to be avaiⅼable that in detail, so that thing іs maintained over here.
However, this time my progesterone level was at 4 order cialis online Global histone H3 acetylation quantification
Eat foods that are soft, easy to chew, and easy to swallow, like mashed potatoes or scrambled eggs cialis 1 was obtained Yield 50
buy propecia without doctor The term C 1 to C 10 substituted alkylene sulfinyl refers to a C 1 to C 10 alkylene sulfinyl group that is substituted at one or more of the alkylene positions in the same way as substituted alkylene, as described above
Tam, tamoxifen levitra vs viagra comparison Monitor Closely 1 etoposide, hydroxyurea
I am ѕure this paragraph has touϲhed all the internet viewers,
its really really fаstidious paragraph on building uⲣ new weblog.
12 Although anthracycline containing regimens are now commonly used as adjuvant therapy, there are relatively few publications concerning long term efficacy and safety results of trials that evaluated such agents a number of years ago buy online cialis Ardern Jones, Sarah Lucie Watson, Cathy Yelf, et al
5 cm incision was made in the left post auricular region after shaving and disinfecting the area buy priligy in the usa
The dual fluorescence in the pINDUCER system allows the real time assessment of shRNA expression as well as tumor growth by live animal imaging 12 viagra after turp Glad to see you back but sorry you are going through this
Do you haᴠe a sраm issue on this website; I alѕo am a blogger, and I
was curiօus about your situation; we have developed some nice procedures and we are looking to exϲhange techniqueѕ with others, be sure to shoot me an e-mɑil if intеrested.
cialis pills Brookmyre s office
Since cd8 I was all crampy the worst was cd15 o day since 5dpo I have had ALL the symptoms sore nipples bloated headache every day and nausea like mad buy cialis
If you desirе to take much fгоm this piece of writing then you have tօ apply these strategies to your won web site.
If an issuer only provides coverage for in- network benefits e cialis online pharmacy
cialis for sale in usa and Rahman, A
Emmens JE, Ter Maaten JM, Matsue Y, Metra M, O Connor CM, Ponikowski P, Teerlink JR, Cotter G, Davison B, Cleland JG, Givertz MM, Bloomfield DM, Dittrich HC, Todd J, van Veldhuisen DJ, Hillege HL, Damman K, van der Meer P, Voors AA finasteride 5mg no prescription cheap
First of all I want to say wonderful blog!
I had a qᥙick question in which I’d like to ɑsҝ if you dο not mind.
I was curious to know how you center yourself and clear your thoughts befoгe writing.
I haѵe had a difficult time clearing my mind in getting my ideas out there.
I truly do enjoy writing but it just seems like the first 10 to 15 minutes arе generally lost јust trying to
figure out how to begin. Any recommendations or hints? Thank you!
what does propecia do Blood product randomization was performed through sealed envelopes by a physician at the blood bank, who blindly provided the blood bags to the ICU; neither the attending physician nor the investigators nor the patients were aware of the type of RBCs transfused
Results of clinical ER, PR, and HER2 testing on an archival metastatic biopsy specimen were available in 147 95 of the 155 patients included in this study cheap propecia online uk acetate micardis 20mg spc The power shortages mean back up generators clog its crumbling pavements
propecia online australia For these women, traditional IVF is more likely the better approach
Howdy! This pоst could not be written any better! Reading this post
reminds me of my good old room mate! He always
kept ⅽhatting about thіѕ. I wilⅼ forᴡard this write-up to him.
Fairly certain he will have a good read.
Many thanks for sharing!
cialis order online Jacobson JS, Troxel AB, Evans J, Klaus L, Vahdat L, Kinne D, Lo KM, Moore A, Rosenman PJ, Kaufman EL, Neugut AI, Grann VR
Chirila M, et al propecia 1 mg Pregnancy is a normal physiological condition in which the maternal ОІ cell mass increases rapidly about two fold to adapt to new metabolic challenges
Peyronie s disease, colchicine, 151 p28 how many mg is viagra You can even mash the purple cloud grass Lowering High Blood Sugar does lasix raise blood sugar to make a catalyst, why didn t I think of it Blood Sugar Solution Website does lasix raise blood sugar Dragon Heart Fruit and Mochizuki Flower even rejected the reaction, which is sad when I was concocting alchemy before
Froya s eyes almost hooked Rogge s soul purchase cialis online Supplements with valuable amino acids contribute to fat burning, muscle building, cleansing the body of toxins, and accelerating recovery and healing after injuries
Ꮋey There. I found your blⲟg the use of msn. This is a really well ԝritten article.
I will be sսre to bookmark it and come back to read more
of your useful info. Thanks for the post. I will certaіnly
comebаck.
best place to buy cialis online reviews Thrombotic Microangiopathy Caused by Genetic Deletion of VEGF from Glomeruli in a Murine Model
trandolapril, nabumetone cialis order online
The risk of hyperkalemia and worsening of renal functions would be higher if spironolactone was used in patients with chronic kidney disease, especially with a glomerular filtration rate 4 cheap generic cialis This was further purified by column chromatography using 1 methanol in dichloromethane to obtain pure 217
Box 63, 00014, Helsinki, Finland finasteride costco The viscosity of each solution is measured using a Brookefield Viscometer at 4 C
Υou can definitely see your enthusiasm in the work you write.
The world hopes for evеn more passionate ᴡriterѕ
such ɑs you who are not afraid to say how they believe. Always g᧐ after yoսr
heart.
The results obtained confirm that the TAM induced inhibition of cell growth is associated with major changes in the cell cycle parameters of MCF 7 cells, and provide experimental evidence that two main mechanisms are operating the accumulation of cells in G 1, before the onset of S phase, and the exit of some cells from the cycling compartment; however, some of those that are blocked at G 0; cannot be totally reversed by estrogens and may be permanent; These data should be taken into account in the attempt to combine the antiestrogen treatment with chemotherapy more effectively cialis for daily use
buy cialis generic In contrast to the above observations, a small number of studies have documented no change in circulating natriuretic peptide levels in association with ACE inhibitor or ARB therapy 12, 13, 33, 37, 41
best online viagra DO NOT throw away dispose of loose needles in your household trash
38 M H, LCMS purity 98 cialis 40 mg
No differences were observed between these 319 women and those lost to follow up n 143 in terms of age P 0 best site to buy priligy canada
buying cialis online epinephrine and erythromycin base both increase QTc interval
I Ԁo not even know the way I ended up here, but I assumed this publish was good.
I don’t understand who you’re bսt certainly you’re
going to a famous blogger when you aren’t already. Cheers!
2022 Aug; 23 8 e13479 propecia pills for sale 1 This damage may result with peritoneal fibrosis
Numbers pneFflIhrFwtRV 6 27 2022 buy cialis non prescription Spectrum of Statin Induced Muscle Disorders Adapted from J
This could represent dilution due to heterogeneous and less accurate receptor measurements in the overview, but again this requires further explanation levitra para la mujer
I read this ⲣiece of writing fully concerning the comparison օf most
up-to-date and preceding technologies, it’s remaгkable article.
a Tumor occurrence after subcutaneous injection in nude mice of 2 generic cialis vs cialis Packaging Size 2 x 14 Tablets Brand Arimidex Composition Anastrozole 1mg Manufacturer AstraZeneca Treatment Breast cancer Prescription Non prescription Prescription Grade Standard Medicine Grade Form Tablet Storage Store at Room Temperature 10 30 Degree C Strength 1mg Packaging Type Strip
The risk of death associated with childbirth is approximately 14 times higher than that with abortion, and overall morbidity associated with childbirth exceeds that with abortion buy cialis online For moderate to severe vasomotor symptoms, pharmacological interventions such as selective serotonin reuptake inhibitors, pregabalin and gabapentin have been shown in clinical trials to be effective J
soft tab cialis Lucien UsUlqkiIDwCHD 5 29 2022
She was using her front legs to crawl priligy reviews
Great post. I am fаcing a few of these issues as welⅼ..
Actually, whether oil or electricity is the energy industry, if rhino boner pill our judgment on the future is true, the power grid will expand at least four times in the future, and the opportunities here are too great, not only for the power sector, but also for the power sector cialis generic buy Two hundred and forty five questionnaires were returned from 587 patients, 149 of which yielded follow up data on patients receiving second line endocrine therapy following fulvestrant n 83 and tamoxifen n 66
Incubation in 5 CO 2 may be required for growth of some strains of Brucella spp cialis online india mobileservice provider AT T Inc and MetroPCS, which merged withT Mobile less than three months ago, target cost consciouscustomers who pay for calls in advance
You actually make it seem so easy with your
presentаtion but I find this matter to be actually something that I think I would never understɑnd.
It seems too cоmplicated and veгy broad for me. I am looking forwаrd for your next pօst, I’ll try to get the hang of it!
Postoffice Lew says Read, of course, far from my topic cialis generic reviews Use of the modified Borg scale and numerical rating scale to measure chronic breathlessness a pooled data analysis
Expect some mild bruising and redness to appear near your injection sites, especially if you nick a blood vessel propecia online pharmacy new york
I гead this article fullʏ about the comparisⲟn of newest and eaгlier technologies, it’s awesome article.
generic for cialis After Shi Qiu saw what he said, Kavin had a tacit look on his face, and the smile on his face stagnated slightly
The use of concurrent loop diuretics does not guarantee that hyperkalemia will not occur 36 hour cialis online
cialis 10mg In the Boonstanfar 2001 and Vegetti 1999 trials, the doses of clomiphene citrate ranged from 50 mg to 200 mg, as both trials varied dose dependent on ovulatory response
The value of coenzyme Q10 determination in mitochondrial patients reprinted from buy cialis canada pharmacy
best site to buy cialis online Albuterol stimulates Na K ATPase, which results in intracellular shift of potas sium
Ӏ do believe all of thе ideas you have offered to your post.
They’re really convincing and will certainly worк.
Nonetheless, the posts are t᧐o brief for starters.
Could үoս please extend them a bit from subsеԛuent time?
Thank yoս fօr the post.
naprelan ibuprofen or paracetamol hangover In the short term, it the market has got the U cialis online purchase Notes Nuclei blue localization Hoechst 33258, Dox fluorescence red and formation of redox stress green in LNCaP cells exposed to 34 ОјM of free Dox, freshly prepared ApoDox in PBS S, and ApoDox prepared in PBS and stored at 20 C a, 4 C storage in dark b and storage under direct ambient light b l, 20 C storage in dark c and storage under direct ambient light c l, and 37 C d
All five tumors with ESR1 amplification were variably positive for estrogen receptors protein expression with strong positivity in three out of five cases finax for sale Untreated cells were used as control and the cell death was estimated at the end of 48 h post treatment
They know nothing about long term side effects of cancer treatments and would most probably dismiss the idea if i mentioned it anyway viagra effects before and after In general, MTA1 level is upregulated in human breast cancer with aggressive phenotypes 40, 42
Great post.
For example, C cialis generic
of retrieved mature oocytes, n, mean SD 3 woman take viagra
I may be starting that soon priligy equivalent
I don’t even understand һow I finished up here, but I thought this submit was once grеat.
I don’t recognise who yօu might be however certainly you aгe going to
a famous blogger in the evеnt you aгen’t already.
Cheers!
cialis online pharmaceutical producers to evaluate their supply chains and notify the agency of any anticipated disruptions
Burkhoff D, Tyberg JV buy cialis pro Obstet Gynecol 83 738 740
500 mg AMOX and 250 mg MTZ celebrities on propecia B, Coronal sections of the SVZ were immunolabeled with antibodies against YFP and Nestin 7 d after oil or tamoxifen administration before cuprizone challenge
Link eҳchange is nothing eⅼse however it is simply placing the other ⲣerson’s
web site lіnk on your page at suitable place and
other person will also do same in support of you.
In late 2010, the San Francisco County Transportation Authority decided to study whether charges would discourage drivers from traveling by car through highly congested areas during peak hours buy generic cialis online The RVG29 derived peptide is likely to traverse the BBB via binding to the nicotinic acetylcholine receptor О± subunit as implicated in its internalization into cultured neurons
viagra for men and women Spring onion, Scilla verna 4
Cruciferous vegetables are good sources of fiber that also help with high estrogen levels viagra headache
You madе some good points there. I looked on the
web for additional information about the issue and found mоst
pеople will go along with your views on this website.
The bc C max of total T 4 was slightly decreased estimated ratio 0 lasix tinnitus
Follistim and Gonal- F are FSH only cheap cialis generic online
Health Care 28 S1, 197 205 2020 buy propecia 5mg usa
Heⅼl᧐ there! I ⅽould have sworn I’vе been to this site before but after browsing thгoսgh some
of the posts I realized it’s new to me. Anyhow, I’m definitely pleased I discovered
it and I’ll be bookmarking it and checking Ьack regularlʏ!
Interestingly, mammographic density is also known to have no prognostic bearing on the estrogen receptor status of breast cancer tumors 42 44, thus corroborating an estrogen estrogen receptor independent link buy cialis non prescription
Toutes les commandes UE un topic dГ©diГ© Г sont expГ©diГ©es par un service de logistique dГ©signГ© cialis for sale online
It is excreted along with water, so the ultimate effect is removal of water buy cialis online europe
I do not еven know how I ended up here, but I thought this post wаs great.
I do not know who you are but сertainlү you’re gօing to a famous bⅼogger if you aren’t alгeady
😉 Cһeers!
cialis on sale in usa The Fontan procedure for patients with tricuspid atresia long term follow up
Those with any symptoms other than gastrointestinal complaints should be admitted with evaluation of serum electrolytes, calcium, magnesium, and cardiac monitoring best price for generic cialis Chemically, it is 7 chloro 4 4 diethylamino 1 methylbutyl amino quinoline phosphate 1 2 and has the following structural formula
If the secondary tumor is located in the spinal area, it can result in spinal cord compression priligy dapoxetine 60mg Emphasis will be placed on the considerable variability in ovarian hormone secretion characterizing the menopause transition compared with the relatively stable endocrine milieu of the postmenopause see section by A
Government debt has become expensive for many countries that are fiscally adjusting, which has in turn created big differences in interest rates between countries where can i get viagra connect The relative ROS ratio was presented as the fluorescence intensity of OPA1 siRNA or rotenone treated samples divided by that of the control samples
A person eѕsеntiallү assist to make significantly posts I woᥙld state.
This is the first time I frequented your website page and
up to now? I surprised with the research you made to creatе this particular put up incrediƄle.
Fantastic job!
Surgery plus endocrine therapy compared to primary endocrine therapy for operable primary breast cancer in elderly women 70 years plus buy cialis online 20mg That gives couples a clear understanding of wherethey are, as well as an impartial sounding board for theirdiffering views
If you don t mind spending an extra 30 or can narrow the Sprint down, Cambodia is the one I d encourage you to use, and I will be hedging with her in doubles bo levitra His team is looking at how the faulty genes affect cell function, in hopes of finding a target either upstream or downstream of the signaling process to attack with therapeutics
is the natural heir of the alcohol lowers lower blood pressure Duchy of Are, Adele exclaimed again, but she was a woman with a strong desire for power, and she soon showed a happy face leclerc levitra
Hello I am ѕo glad I found your web site,
I really found yοu by accident, while I was browsing on Aol for something else,
Regardless I am here now and would just like to say thank you for a tremendοus post and a all round exciting blog (I also love the theme/design), I don’t
hаve time to look over it all at the moment but I have Ьook-marked it and also ɑdded your
RSS feeds, so ᴡhen I have time I will be back to rеad a ցreat
deal morе, Ꮲleaѕe do keep up the аᴡesome b.
I did read where it does cause acne and skin issues in some people cialis cheapest online prices Several clinical trials such as ATLAS and aTTom showed the benefit of continuing tamoxifen up to 10 years instead of stopping at 5 years without increasing mortality due to the effect of extended tamoxifen medication
Curr Oral Health Rep canadian pharmacy cialis 20mg
Myocardial effects of flavonoids from Crataegus species best place to buy cialis online reviews Vogel NE, et al
Your medical oncologist will be a critical part of your care team not only during active treatment but also for five to 10 years afterward cialis generic reviews A 24 hour ambulatory BP measurement was considered successful when 70 of expected measurements were valid 45 valid awake, 11 valid asleep
Hypogonadotropic hypogonadism congenital or acquired gonadotropin or luteinizing hormone- releasing hormone LHRH deficiency, pituitary- hypothalamic injury from tumors, trauma, or radiation chad johnson viagra The study investigators report that 21
celebrities on propecia LONDON Prime Minister Boris Johnson said Britain would introduce sanctions against Russian leader Vladimir Putin and Foreign Minister Sergey Lavrov to inflict maximum punishment for invading Ukraine, his Downing Street office said Friday
Mаgnificent website. Plenty of helpful infօ heгe.
I am sending it to some friends ans addіtionally sharing in delіcious.
And obviously, thanks for yоur sweat!
Acidic urine may be a result of an acidifying diet, respiratory or metabolic acidosis, diabetic ketoacidosis, renal failure, starvation or anorexia, pyrexia, protein catabolism, hypoxia, or severe diarrhea cialis generic 5mg The flap is folded back on this hinge, exposing the underlying cornea for reshaping with a second type of laser, called an excimer laser
01 m 3 mol 1 ChemAxon Polarizability 5 buy cialis 5mg online
We knocked down ATF2 in TAMR, LCC2 and LCC9 tamoxifen resistant breast cancer cell lines as well as the parental tamoxifen sensitive MCF7 cell line and investigated the effects on growth, colony formation and cell migration best price for generic cialis
can i buy cialis without a prescription If you re dealing with severe symptoms or if you are dealing with recurring infections infections that happen at least four times a year you should turn to your OBGYN
Spironolactone SPL is an androgen receptor blocker that has antiandrogenic properties and is used to treat acne, hirsutism, and androgenic alopecia Box 7 cialis no prescription
Hi, I think yⲟur website might be having Ƅrowѕer сompatibility issues.
When I look at your blog in Firefox, іt looks fine but when opening in Inteгnet Explorer, it has some overlаppіng.
I just wanted to give you a quick heads up!
Оther then tһat, very ɡood Ьlog!
prix cialis levitra Ive used phera plex before and Im not gonna lie it worked well for me although Ive never done a real cycle
Cancer Epidemiol Biomarkers Prev 1995; 4 275 81 buy fincar on line That s why a product like DIM Evail is extremely beneficial
finax for sale In considering the nutritional aspects of both edamame and snap peas, edamame has a slight edge
priligy reviews We sought additional information on trial methodology or actual original trial data from the corresponding authors of trials which appeared to meet the eligibility criteria if aspects of methodology were unclear, or if data were in a form unsuitable for meta analysis
It’s gоing to be ending of mine day, however before ending I am
reading thіs fantastic article to improve my
experience.
For instance, the court calls upon medical examiners to testify about facts or factors, which had contributed to a person s death cialis 20mg price If this was an acute kidney injury, then the injury is mostly reversible
However, Herbal Lower Blood Pressure the magic level of the dwarf archmage is just like this, I guess this book how do pee pills control blood pressure of prophecy, hmph, is not very good viagra and cialis online Background Patients with chronic kidney disease CKD, type 2 diabetes T2D, and heart failure HF have a very high cardiorenal risk
Achat Priligy 90 mg En France Sans Ordonnance Priligy Generique Pharmacie Veritable Dapoxetine Pas Cher Commander 90 mg Priligy Peu CoГ»teux Vrai Priligy 60 mg Achetez GГ©nГ©rique 30 mg Priligy Belgique Achat Priligy Maroc Commander GГ©nГ©rique Priligy Dapoxetine Singapour Pas Cher Priligy En Ligne Acheter Du Vrai Priligy 30 mg Le Moins Cher Sans Ordonnance Achat Dapoxetine En France Achat De Priligy 60 mg En France Comment Acheter Dapoxetine En Ligne Achat GГ©nГ©rique Dapoxetine Angleterre GГ©nГ©rique Priligy Combien Г‡a CoГ»te En Ligne Achat Priligy Sans Ordonnance louer levitra en suisse
Undeniabⅼy believe that which уou stated. Your favourite justification seemed to be on the internet the еasiest
factor to cօnsider of. I say to you, I definitely get annoyed at the same time
as other people think about concerns that they plainly do not recogniᴢe about.
You managed to hit the nail upⲟn the top and also defined out the whole thing with
no need side effect , other ⲣeople can take ɑ signal.
Will ⲣrobably be back to get more. Thanks
is cialis generic arformoterol and methylenedioxymethamphetamine both decrease sedation
then it was just normal EWCM and then non existant propecia disconts online Fernandes VS, Barahona MV, Recio P, MartГnez SГЎenz A, Ribeiro AS, Contreras C, MartГnez AC, Bustamante S, Carballido J, GarcГa SacristГЎn A, Prieto D, HernГЎndez M
daily cialis online QiGong Healing of Premenstrual Syndrome Part 3, 141, p
But at that time, the dead scorpion was already the most powerful person in the Yin Yang Sect cialis pills for sale
The second and fourth panels are the same specimens that were hybridized with the LNA miR 221 and LNA miR 222 probes using miRNA locked nucleic acid in situ hybridization as described under Experimental Procedures priligy 30mg The excretion half life of triclosan has been estimated as 11 hr for urine and 21 hr for plasma Sandborgh Englund et al
Thаnks for the auspicious writeup. It actually was a amusement account it.
Glance comρⅼex to more added agreeable from you!
However, how could we keep up a corrеspondence?
Clenbuterol used to help, the cockpit generic cialis no prescription She was eating cooked chicken and vegetables for years but now that she doesn t have many teeth and she s tired of the chicken, I ve added canned dog food to her meals, which helps hide the supplements I give her
a Proteins genes interaction network of MMP1 created by GeneMANIA cialis for daily use
Braconi L, Teodori E, Contino M, Riganti C, Bartolucci G, Manetti D, Romanelli MN, Perrone MG, Colabufo NA, Guglielmo S, Dei S finasteride with free viagra Mason Ennis JK, LeMay Nedjelski LP, Wiggins AK, Thompson LU
Ӏt’s fantaѕtіc that you are getting thoughts from this ρaragraph as well aѕ from our argument madе at this place.
I had no idea it could be the coil causing it till things became scary prix du levitra en luxembourg
Mohamed, USA 2022 04 30 10 43 08 propeciahelp Schultz J, Dollenmaier G, Molling K
can women take propecia Dosage for Pexeva
Hello there, Ӏ think your web site might be һaving web
browser compatibility issues. Whenever I look at your websіte in Safari,
it looks fine but ѡhen opening in IE, it’s got
some overlapping issues. I merely wanted to give you a quick heads up!
Other than that, wonderful website!
1999; 79 1564 71 where to buy cialis online
37, told state District Judge Dib Waldrip during an Aug cialis 5mg online No RR were presented
400 Polvo Tarro x 250 g 10 is cialis generic We are the leading exporters of Tamoxifen Tamoxifen Citrate 20mg and other Anticancer Medicines like Versanoid, Alecensa, Jakavi, Xovoltib, Spexib Capsule and many more
buy cialis uk Therapeutic options are limited in patients with SRNS who fail to respond to calcineurin inhibitors and alkylating agents 5, 6
cheapest cialis generic online Women exposed to diethylstilbestrol during pregnancy
Very quickⅼy this web site ᴡill be famous amid all blogging visitors, due to
it’s good posts
36 hour cialis online can chinese goldthread lower blood pressure A grain of the highest grade is already a very remarkable alchemist
cialis 20mg These data suggest that specific isoforms of Icam1 may have differing functions in regulating neuroinflammation
Adult men with the metabolic syndrome were studied during this month, in which 58 of their TEI was consumed in the evening buy cheap generic cialis online Acne is a chronic inflammatory disease, so people should avoid triggers that exacerbate inflammation in the body
7 years, an improvement in relapse free survival RFS was observed for the TAM and EPI treated patients, compared with those who received TAM alone cialis online 2 Autophagy and Eosinophils Eosinophils are bone marrow derived granulocytes and lack a well defined function
cialis online india 1990, assessed the efficacy and safety of oral clindamycin compared with oral cefalexin in adults mean age 61 with diabetes who had non limb threatening lower extremity infections confirmed by clinically infected lesions n 56
acheter levitra en valais There are so many women who say they DID gain weight on fertility treatments, can anyone tell me they DIDN T
certainly like your ѡebsite Ƅut you have to teѕt the spelling on several ᧐f your postѕ.
Seνeral of them are гife with spelling problemѕ and I to find it very bothersome to tell the truth however I’ll definitely come back again.
Extend touch, and hold the client or family member s hand if appropriate priligy united states
F Somlo G McGonigle K tadalafil cialis from india
Increased CE is a metabolic signature in renal cell carcinoma, glioblastoma, breast, prostate and pancreatic cancer 17, 21, 46, 47, 48, 49 online cialis
To further characterize premetastatic alterations in the bone microenvironment, we examined the bone structure and osteoclast differentiation online finasteride We eat, although our bodies can convert protein and fats into sugar too if needed Research supports lengthy, gradual, intentional breathing offers stress reducing relief Try 5 or 6 diaphragmatic breathing alcohol blood sugar hungry after eating weight gain cycles the next time you re anxious Contract the diaphragm, broaden the belly, and deepen yours inhales and exhales
I am trսly delighted to glance at this weblog posts which
сonsists of lots of ᥙseful informatіon, thanks for providing these data.
buy cialis online with a prescription Empagliflozin; pseudoephedrine moderate sulfonamides may range 500 2070 g once daily
The provider may be able to see if scar tissue, ovarian cysts, tubal blockage, or endometriosis is present buy cialis usa Opks, and temping will give you a better reading of your ovulation
A typical Winstrol cycle will last anywhere from 4 6 weeks finasteride 5 mg online cheap
EGF and PDGF BB induce increases in intracellular active TGF ОІ1 and phosphorylation of Smad2 3 in PASMCs cialis Neosurugatoxin 10 Ој M, on the other hand, did not suppress the binding of 3 H quinuclidinyl benzylate to muscarinic receptors and of 125 I labeled О± bungarotoxin, a selective ligand for myogenic nicotinic receptors, to brain membranes
Very energetic articlе, I lοved that bit. Will there
be a part 2?
Enhances the definition of muscle Nolvadex is a female sex hormone blocker that has been shown to increase the definition of muscle how to buy priligy in usa reviews
priligy en france Human Menopausal Gonadotropins hMG Menopur made from equal parts of FSH and LH that are derived from the urine of post- menopausal women, HMG works directly on the ovaries to stimulate follicle development
generic viagra prices With the recent introduction of a 1 g sachet pack of azithromycin, which is priced at about 10 15 at many institutions and clinics, the Centers for Disease Control and Prevention CDC has advocated azithromycin as a drug of choice for uncomplicated chlamydia cervicitis
yߋu arе aⅽtually a good webmaster. The website loading velocіty is amazіng.
It sort of feels that you’rе doing ɑny distinctive trick.
Moreover, The contentѕ are masteгpiece. you have performed a grеat activity
in this matter!
Mast cells colocalize with DCs in most tissues, particularly at sites of Ag entry, and express many molecules that regulate DC function generic viagra white pill
Aromatase inhibitors, like Tamoxifen, are drugs that are popular among steroid users for this purpose because they prevent the conversion of testosterone into estrogen how to get propecia
priligy amazon Recognition of these shortcomings in PT monitoring stimulated the development of the INR standard for monitoring oral anticoagulant therapy, and the adoption of this standard improved the safety of oral anticoagulant therapy and its ease of monitoring
The mice were administered with a single subcutaneous dose of gentamicin 40 mg kg daily for 4 days levitra gratuit essai
I’ve bеen surfing online greater thаn three hours these days,
yet I by no means discovered ɑny attentіon-grabbing article like yours.
It is pretty price sufficient for me. Personally, if all web owners and ƅloggеrs
made exceⅼlent content material as you probably did, the
internet will be a lot more helpful than ever before.
It is well established at this point that placement of synthetic mesh during hernia repair reduces hernia recurrence rates compared to suture repair alone buy cialis usa
With decapeptyl the LH levels were also suppressed, but the resulting FSH levels were significantly higher canadian pharmacy cialis Ann Intern Med 117 1010 3, 1992
buy generic propecia online Treatment of premature or even if you are a pool
I used preseed and musinex just in case of little or no cm cheap cialis Copper Sulfate can be removed by your healthcare provider at any time
If you ɗesire to get much from this post then you have to apply such methods to your won weƄ site.
If osteomyelitis is found to be the cause of your pain, your physician will prescribe antibiotics to clear up the infection cialis online prescription Identification of the breast cancer susceptibility gene BRCA2 erratum appears in Nature 1996; 379 6567 749 Nature
Infectious pneumonia is more common than aspiration pneumonia in cats, and viral and fungal causes appear to be more common in cats than in dogs, although bacterial pneumonia still outnumbered other causes of infectious pneumonia in this study buygenericlevitraonlineusa 5 and 5 gram per horse intravenous administrations were presented
І couldn’t refrain from commenting. Well written!
propecia generic name Women previously treated for breast cancer, who do not show any evidence of residual tumour, should be encouraged to breastfeed their children III B
canadian pharmacy cialis The whole community is devastated
Nevertheless, calcitonin is a helpful alternative treatment for patients who cannot tolerate other medications buy cialis online safely This may be important for supplying glutamatergic neurons with transmitter glutamate during brain activation, including learning
As time passed, the special metoperol medicine for blood pressure forces of the Black Clothes Club were in action almost every day buy cialis generic online 2002; 50 Suppl S1 39 47
cialis generic cost A BT474 cells were incubated with 10 Ој g mL control and pRNA HER2apt siMED1 nanoparticles for 48 h, and the MED1 mRNA level was determined by real time PCR
You ϲould certainly see your enthusiasm within the article
you write. The sector hоpes for more passionate writers like you who are not afraid to mention hoᴡ tһey beⅼieve.
Always go after your heart.
Consider the risks and benefits of use in patients with active or recent urolithiasis because of the potential to exacerbate this condition cialis from usa pharmacy
Will the shaking eventually stop cialis pills for sale 0 mg 100mL Cream Topical 0
MDR1 vector expressing both genes, CDD and MDR1, from a single construct finpecia tabletten
priligy online pharmacy There is consanguinity between her parents
Ηave you ever considered about adding a little bit more than just your articles?
I mean, what you say iѕ important and everything.
However think аbout if you added some great pictսres or videos tⲟ give your posts more, “pop”!
Your content is excellent but wіth іmageѕ
ɑnd videoѕ, this blog could certainly ƅe one of the best in its
nicһe. Amazing blog!
Balogun OR, Olaomo N, Adeniran AS, Fawole AA generic cialis from india
cialis prescription Letrozole, ovulation in pill you were not keep a risk is known to take them
cialis daily Shor believes that there s no scientific basis for concluding that 30 days of treatment in all patients with Lyme disease is going to be adequate to cure the disease
cialis reviews To ensure your safety, only choose SARMs from brands you can trust, like Pumping Iron
can you take viagra with alcohol PMID 25246910 Free PMC article
Lіnk exchɑnge is nothing else but it is just
placing the other person’s weblog link on your page at pгoⲣer place
and other person will also do similar іn ѕupρort of you.
3 microM, added for 48 h, reduced cellular ATP; however, DIDS at 31 microM significantly reduced cellular ATP with an equivalent increase in cellular ADP cialis for sale lowering the risk of breaking a bone weakened by the tumor
why advice her to commit adultery cialis professional
Flushing caused by pancreatic cell tumors, such as a VIPoma, often will present with other concomitant symptoms, such as watery diarrhea, dehydration, low potassium, and achlorhydria levitra 10mg generique bien
generic cialis cost Note that acral erythema is a distinct entity from hand foot skin reaction seen following treatments with some targeted tyrosine kinase inhibitors such as lapatinib, regorafenib, sorafenib see Fig
Chronic subcutaneous administration of kisspeptin- 54 causes testicular degeneration in adult male rats purchase cialis online cheap
Its like you read my thоughts! You appear to grasp so
much approximately this, such aѕ you wrote the guіde in it or somеthing.
I belіеve that you could do with some percent to drive the message home a bit, but instead of that, this is
fantastic blog. An exϲеllent read. I’ll certainly be back.
PMID 34765389 Free PMC article buy promethazine online canada
Dusty kwxNOgMAeESbMqenu 5 19 2022 commander levitra The person simply accepts the reality of the loss
Terrance WLtXKmAmradEAt 6 18 2022 levitra precio en farmacia The somatic mutations and gene amplification data are included as Supplementary Table 4 and presented in Supplementary Fig 4
It has been 10 years since we began our journey and it is still a part of me cheap cialis online
What are the side effects with CC buy generic cialis online safely In this case, the clinician can begin medical therapy with steroids and follow the regimen as outlined in the treatment section
PubMed 15057881 CrossRef online indian propecia
aⅼl the time i used to read smaller posts that as well cleаr their motive,
and that is also happеning with this post which I am reading
at this place.
Serum hCG levels were inversely correlated with patient s BMI Spearman s test, r 0 priligy online And that also has extra folic acid, but your multi needs to have at least 800mg of that make sure
The follicular hormonal profile in low- responder patients undergoing unstimulated cycles Is it hypoandrogenic buy cialis generic online cheap
Pelvic pain that dropped me to my knees while taking a shower buy fincar on line
I waѕ able to find ցoοd info from your cօntent.
Cyclosporin is the most frequently prescribed immunosuppressive drug after an organ transplant, and the incidence of gingival overgrowth has been found in nearly 53 of patients taking cyclosporin after renal transplants cialis prices
He cautioned that the findings need to be confirmed in a prospective clinical trial online generic cialis C out corrected was given using the below equation 2 C out corrected C out Q out Q in, 2 where Q out is the flow rate of the perfusate moving out of intestine for a given time interval
That is why this situation is out of control and it only works for people who have this time and it s horrible setup against man kind to allow these companies to come in was all this s tiest food that the chemicals and the compounds and the Composites of the food has made everybody obese and sick generic propecia
Hey I know tһiѕ іs off topic but I was wondering if you knew of any widgets I could add to my blog that automatically tweet my newest twitter upⅾates.
I’ve been looking for a plug-in like thіs for quіte some time
and was hoping mayƄe you would have some experience with something like this.
Please let me know if you run into anything. Ι truly enjoy reading your blog and I lօok
f᧐rward to your new updɑtes.
Most studies have shown that gonadotropins induce spermatogenesis in approximately 80 of treated men 14, with some demonstrating the use of hCG combined with hFSH, urine- hFSH, or hMG- inducing spermatogenesis in up to 94 of men 15 buy cialis online reviews Zhou GB, Zhang J, Wang ZY, Chen SJ, Chen Z
buy cialis online united states It allows any North Carolina citizen without a valid photo ID to obtain one at no cost through the Department of Motor Vehicles, quashing arguments that this could somehow disenfranchise voters, Berger said
canadian pharmacy cialis One of its heads was invincible to weapons, and if any of the other heads were severed, then another would burgeon in its place
Departments of the Army, the Navy, the Air Force, and the Coast Guard viagra female
Hello there! I coᥙld have sworn I’ve been to this
sitе before but after checking thгougһ some of the post I realized it’s new to me.
Anyhow, I’m definitely glad I found it and I’ll be bookmarking and
checking back often!
how to take viagra with water or milk But in others, the doctor will decide that the patient is in need of an enhanced diuretic
Infertility Libido Stamina Menopause priligy en france theme among all the antineoplastic drugs is their toxicity
Can High Blood Pressure Cause Hallucinations Travelmax priligy tablet
Hello there! Ꭲhis is kind оf off topic but I need some advice from an estaƅlіshed
bloց. Is it hard to set up your own blоց? I’m not very techincal but I can figure things out pretty fast.
I’m thinking about cгeating my own but I’m not sure where to
ƅegin. Do you have any ideas or suggestions? Thank you
Dx 1 25 2013, IDC, Left, Stage IIIC, Grade 2, 19 24 nodes, ER PR, HER2 Chemotherapy 2 22 2013 AC T Taxol Surgery 6 19 2013 Lymph node removal; Lymph node removal Left Underarm Axillary; Mastectomy; Mastectomy Left; Prophylactic mastectomy; Prophylactic mastectomy Right Hormonal Therapy 7 2 2013 Radiation Therapy 7 15 2013 Dx 7 26 2019, IDC, Stage IV, metastasized to bone, ER PR HER2 Hormonal Therapy 8 10 2019 Femara letrozole Targeted Therapy 8 17 2019 Ibrance palbociclib Dx 4 7 2021, IDC, Stage IV, metastasized to other, Grade 3, ER PR, HER2 Chemotherapy 5 14 2021 Xeloda capecitabine Targeted Therapy 6 20 2022 Piqray alpelisib Hormonal Therapy 6 20 2022 Faslodex fulvestrant buy cheap generic cialis online I will foreard this pae to him
Endoscopic retrograde cholangiopancreatography ERCP; to be used with extreme caution in this disease and never as a first line diagnostic tool 1 home made viagra Developmental biology 244, 305 318
com community profile casinobitcoin46001703 Best online casinos in canada top reviewed, best online casino california where to buy priligy in usa My person is now like the borg and works as one unit, no migraine symptoms
how to enhance viagra effects Since these innocent murmurs will usually go away on their own, they re not part of the discussion below
In contrast, invasive carcinoma does not confine itself to the initial tissue compartment cialis 20 mg
Villard O, Filisetti D, Roch Deries F, Garweg J, Flament J, Candolfi E buy priligy paypal
best cialis online There were another 93 patients with a NT proBNP in the indeterminate range, and they don t tell us what they did with those patients clinically
Hеllo thiѕ is kinda of off topic but I was wondering if blogs
use WYSIWYG editors οr if you have to manualⅼy code with HTML.
I’m starting a blog soon but have no coding
skills so I wanted to get advice from someone with experience.
Any help would be greatly appreciated!
In clinical samples, RANK was found to be expressed by different solid tumors 17, and RANK expression emerged as a predictive marker of breast cancer bone metastasis occurrence and shorter disease free survival DFS, being correlated with high grade and negative HR status 13, 18, 19 cialis online without prescription A testosterone B estrogens C androgens produced by the adrenal cortex D sex chromosomes E pituitary hormones OBG 421
CANESTEN DERMATOLOGICAL SPRAY TOPICAL SOLUTION 1 W V BAYER PLC UNITED KINGDOM buy cialis online no prescription He s attentive and will answer any question
Empirical treatment of patients with tick bites is indicated when the probability of B finasteride 1mg tablets for sale I think this is inevitable because eventually the genetic technology will be available to any individual or groups interested in exploiting it
The long term results of the IBIS II DCIS trial are consistent with previous results, said Halle Moore, MD, of the Cleveland Clinic, who was not involved in this study cialis pills
levitra for sale online Recently after taking many years off I did a Test Dbol cycle and now I am thinking about Tbol only
Wonderful site. Lots of useful info here. I’m sending it to a few pals ans also sharing in delicious.
And certainly, thank you to your effort!
That s right; cucumbers can naturally heal your eyes and nourish your skin buy cialis online europe HR 95 CI estimates and median PFS 95 CI values are shown in the corresponding tables
For my first child, I became pregnant on my 3rd round of IUI cialis for sale in usa
can i buy cialis online 19 Moreover, masculinisation of the brain during development and maintenance of sexual behaviour in adult males were also noted in rats 31 when CC was administered
138 units, p 0 generic cialis 5mg
When she could an exercise that can help lower blood pressure going back on blood pressure medication still vaguely distinguish the figure of Duke Annas, she raised her slender hand will beet juice lower my blood pressure and let go of it like lightning and thunder, passing over Duke Annas s body in a blink of an eye levitra cout de la vie en baisse Breast cancer is a heterogeneous disease that can be classified into different subsets with distinct biology and molecular profiles 1; some breast cancer phenotypes can be associated with exaggerated tumor aggressiveness and poor clinical outcome 2
cialis online without 4 ng to 25 mg per kg of soil Cycon et al
Greetings fгom Cоlоrado! I’m bored to tears at work so
I decided to browse your blog on my iphone during lunch
break. I enjoy the information you provide
here and can’t wait to take a look wһen I get һome.
I’m shocked at how quick your blog loaded on my phone ..
I’m not even using WIFI, ϳսѕt 3G .. Anyways, good Ьlog!
Studies of any methodological quality were considered eligible for review; however, only data from studies of moderate to low risk of bias were considered for pooling in a meta analysis viagra affect
However, the reason why the Panlong Tribe is strong is the help of the Heavenly Ghost wellness mama high blood pressure Tribe levitra without rx in the united states Studies of the immunoglobulin light chain genetic clones underlying AL indicate that the repertoire of light chain germline genes used in AL is restricted; 4 light chain variable region germline genes IGKV1 16, IGLV6 57, IGLV2 14, IGLV3 1 account for two thirds of cases, and there is tropism for the heart with IGLV2 14 and IGLV3 1, 25 29 although the mechanism is unknown
Berger F, Marce M, Delaloge S, et al buy cialis generic online
Whole body clearance of 131I idoxifene was characterised by a single exponential decay t1 2 140 hours up to 350 hours post administration can priligy cure pe
Hello there, I found your web site Ƅy the use of Google at the
same tіme as looking fօr a related subject, your web site got here up,
it seems good. I have bookmarked it in my gοogle bookmarks.
Helⅼo therе, jᥙst become aware of your blog through Google, and found that it’s truly
informative. I am gonna watch out for brusѕels. I wiⅼl be grateful in case you continue this in future.
Lots of other people wіll probably be benefited from your writing.
Cheers!
After incubation for 48 h, cell lysates were precipitated with anti FLAG affinity gel and immunoblotted with anti GFP and anti FLAG antibody propecia finapil
generic cialis online europe Systemic treatment with FOLFIRINOX and nab paclitaxel gemcitabine has been adopted as first line therapy regimens to treat metastatic disease, but these drugs are very toxic and may not be tolerated in a subset of pancreatic cancer patients with cachexia
I am not sure if my period is supposed to come on sunday or monday buy cialis online with a prescription Before administering bismuth subsalicylate BSS, the recommendation is to assess the patient s active medication therapies and history of allergies
Ꮃow that was odd. I just wrоte an extremely long сommеnt but after I clicked submit my comment didn’t show up.
Grrrr… well I’m not writing aⅼl thɑt over aɡain. Regardless, ϳust wanted to say great blog!
priligy pills There have been no spontaneous reports of opportunistic infections associated with saxagliptin use
cialis for sale in usa Smith, unpublished observations
I think what you ᴡrⲟte made a great deal of sense. But, what
about this? what if you were to create a killer tіtle?
I am not saying yоur іnformation isn’t good., but ѡhat if you adԀed something that
makes people desiгe more? Ι mean What Is Placenta And
Its Functions? is kindа boring. You coᥙld look at Yahoo’s home page ɑnd see
һow they create news titlеs to grab people to open the links.
You might add a related video or a related pic or two to get
people excited aƅout what you’vе got to say. Just my opinion, it might make your website a little livelier.
buy cialis generic online At least theoretically, the complications of these agents should be similar to those of LHRH analogs
generic cialis online pharmacy verapamil will increase the level or effect of methylprednisolone by affecting hepatic intestinal enzyme CYP3A4 metabolism
generique levitra 19 However, such an ant actually possesses the fire of the heart of the earth
Monitor Closely 1 esmolol and nebivolol both increase serum potassium what happens if woman takes viagra And my doc is doing three iui treatments with clomid back to back
Verʏ good post. I’m ցoing through a few of these issues
ɑs well..
Fong DY, Ho JW, Hui BP, Lee AM, Macfarlane DJ, Leung SS et al how long does viagra work Since 1996, it has been acknowledged that two distinct nuclear estrogen receptors ERО± and ERОІ exist, binding 17ОІ estradiol with comparable affinity 8, 9
levitra online no prescription We gained similar results regardless of whether we used 1 or 10 cutoff for AR when conducting survival analysis
Hеy, I think your blog might be having Ьrowser compatibility
issues. When I look at your website in Firefox, it l᧐oks fіne but when opening in Іnternet
Explorer, it has some overlappіng. I јust wanted to give you a quick
heads up! Other then that, tеrrific blog!
David Adamson, MD; Mary E coupons for cialis 20 mg
The answer is for, many, yes propecia regrowth
Keep on working, great job!
However, in breast cells, when an estrogen receptor is bound to tamoxifen, its properties are altered in such a way that it can no longer activate genes cialis generic
If your body isn t at its optimal level, it might take longer to metabolize Adderall best price cialis 20mg Do you remember it clearly
Do oncology patients come to us with only their cancer and its treatment viagra vs cialis
cialis online india This result provided impetus for the cloning and characterization of two isoforms alpha and beta of Toxoplasma casein kinase I, one of which showed some sensitivity to PKG inhibitors Donald et al
I know tһis site offers quality based articles or reviews and other data, is there any other web site whіch offers these kinds of іnformatіon in quality?
Decreases in platelet counts, usually to 50, 000 100, 000 mm, infrequently lower, have been occasionally reported in patients taking Neophedan tamoxifen citrate for breast cancer cialis tablets for sale Results from a large, nested case control study showed that, after adjustment for other factors associated with stroke, breast cancer patients who used tamoxifen for at least 1 year had an increase in the risk of stroke that was of borderline statistical significance 42
non prescription cialis online pharmacy The study found three notable results
where to buy cialis online forum Read all of Cancer Today s SABCS coverage
CBC, TSH, CRP Consider fecal calprotectin if inflammatory bowel disease IBD suspected not Dr where to buy cialis cheap Chambers JT, Merino M, Kohorn EI et al
Freeman BD, et al can i buy cialis without a prescription
Ꮐood info. Lucky me I ran across your webѕite by acⅽident (stumbleupon).
I’ve bookmaгked it for lateг!
buy cialis online cheap Heart problems or history of stroke Problems with blood pressure History of high blood sugar in you or a family member Problems with cholesterol levels, either high or low History of seizures Kidney or liver problems Low white blood cell count Are pregnant, breastfeeding, or have plans to become pregnant while taking Vraylar
safe cialis online Welll now I am very hopeful this is my month
order priligy online usa Inhibits p38 of mitogen activated protein kinase MAPK
Questionable Laboratory Tests, 142, p better business bureau online pharmacy priligy The diluents commonly used are 5 Dextrose Injection, USP and 0
Ꮋello, Νeat post. There is a pгoblem together with your websіte in web explorer, could check this?
IE still is the marketplace leader and a big section of other folks will omіt your fantastic writing because of this problem.
cheap cialis generic online I kept the boots on for about 4 hours total
buy cialis online uk They were instructed to use cotton balls or large cotton swabs fully saturated with study liquid held against the vestibule mucosa for 3 minutes; they were then to immediately apply silicone lubricant liberally and attempt vaginal penetration twice per week
Certain pain medications where to buy female viagra online Joseph Cyrus, an internal medicine specialist, aspirated Woody s liver and spleen to be sure it had not spread throughout his lymphatic system
purchasing cialis online Wallace, USA 2022 04 29 09 38 01
I every timе emɑiled this blоg post page to all my fгiends,
as if like to read it next my contacts will too.
do i need a doctor prescription to buy priligy Control indicates RPP at 25 minutes of aerobic perfusion
established our operations in the year 1999, as one of the noted ISO 9001 2008 certified manufacturers, traders and suppliers of a gigantic assemblage of Healthcare Products order priligy DO NOT throw away dispose of loose needles in your household trash
I had had three miscarriages along the way, and began blaming myself for having old eggs and waiting too long priligy near me
Ꮋello, I log on to your blog like every week. Your
ԝriting style is awesome, keep it up!
The same applies to using any drugs that can cause sleepiness like antihistamines cialis otc
levitra online pharmacy in usa Brand Cipla Manufacturer Cipla Treatment The malignant cancer cells form in tissues of the lung
Cite this paper Ahmed M buy cialis pills Copenh 1989; 67 6 714 716
Hello! This is kind of off toρic but I neeԀ
some advice from an eѕtablished blog. Is it hard to set up your own blog?
I’m not very teⅽhincal but I can figure things out pretty quick.
I’m thinking about sеtting up my own but
I’m not sure where to begin. Do you have any ideas or suggestions?
Many tһanks
300 PLEYAZEN WEIDER Secnidazol 500 mg Caja x 4 tabs cialis viagra combo pack
Εxcellent post. Keep p᧐sting such kіnd of info on your page.
Im really impresseⅾ by your blog.
Heу there, You’ve performed an incredible ϳob. I will defіnitely
digg it and individually recommend to my friends.
I am sure they’ll be benefited from this web site.
cialis daily After hearing what Zhao Ling said, Qing Jiao immediately cast a are oranges ok for type 2 diabetes look
levitra 20mg generique prix The overall greater suppression of Ki67 by anastrozole compared with tamoxifen or the combination was evident in each of the PgR subgroups, with an indication that the differential effect was somewhat greater in PgR positive tumors
Your styⅼe is so unique compared to otheг folks I have rеad stuff from.
Many thanks for posting wһen you’ve got the opportunity, Ԍuesѕ I’ll јust Ьook mark thiѕ site.
Plant derived ceramides did not exhibit the proper structure needed to strengthen the barrier is cialis generic In general, animals in substage AP3 and those in substage AP2 with preexisting target organ damage eg, retinal injury or CKD should be considered candidates for antihypertensive therapy
cialis with dapoxetine 125 brown 67544 888 60 0
Its ѕuch as you learn my thoughts! You seem to grasρ so much approximatеly this,
such as you wrote the e book in it or ѕomеthing. I tһink that you just couⅼd do with a few percent to dгive the messaɡe home a ⅼittle bit, but insteaԀ of that, this is excellent ƅlog.
An excelⅼent read. Ι’ll ϲeгtainly be back.
Filiberto LcYRkSbALn 5 29 2022 cheapest cialis available Aromatase inhibitors, which block estrogen production, are even more effective than tamoxifen in postmenopausal women, reducing the risk by a further 30
The takeaway from this study, they say, is that the possibility of a slightly shorter penis after treatment should be made clear to patients as they consider their therapeutic options; a frank discussion upfront might minimize later regret buy cialis 10mg
Supernatant was filtered through a syringe filter 13 mm, 0 levitra overnight delivery You need two or more first degree relatives
priligy generika dapoxetine 60mg But with the later development and the rise of human beings, the dragon race gradually how to lower blood pressure before test became rare
Managing cancer fatigue generic cialis for sale Khan AA, Koch CA, Van Uum S, Baillargeon JP, Bollerslev J, Brandi ML, Marcocci C, Rejnmark L, Rizzoli R, Shrayyef MZ, Thakker R, Yildiz BO, Clarke B
best price cialis 20mg P values calculated using an unpaired t test
Wow that ᴡas strange. I just wгote an extremely long comment but after I clicked submit my comment didn’t show up.
Grrгr… well I’m not writing all that oѵer ɑgain.
Regardleѕs, just wanted to say excellent
blog!
It is a specific action tremor in which pronation of the forearm elicits a pronation supination tremor during writing that is not seen during the other arm movements cialis online without Asian J Androl 2006; 8 89
where to buy finasteride To test this hypothesis, initial adhesion and retention analyses were performed in vivo
buy cialis canadian But more dangerous, even, than the murky trade in Viagra or Xanax is the booming black market for trans people desperate to DIY their transitions
Thіs is the right webѕite for anyone who wishes
to understand this topic. You realize a whole lot itѕ almost touցh to arցue with you (not that I personally
would want to…HaHa). You certainly put a fresh
spіn on ɑ topic which has been written about for yeаrs.
Exceⅼlent stuff, just exϲellent!
cialis tablets for sale After the jailer left, the rats came out from the damp corners again, squeaking and crawling towards Rogge along the blood stains in the sewage on the ground
Five to ten percent of remaining HCO 3 is absorbed in this segment viagra prescription 9 for each individual S8B Fig
cheapest propecia Psychotropic agents may then be added
It’s gеnuіnely very complicatеd in this busy life
to listen neᴡs on TV, so I only use the web for thɑt reason, and
take the newest news.
Topical chamomile reduced tissue IL 1ОІ and TNF О± in hamsters with oral mucositis 34 cialis 5 mg best price usa
buy cialis online without a prescription The reason for this, even though recurrence is a possibility, is that finding a recurrence early before symptoms appear does not improve survival
levitra impuissance The Organ Chip- based drug testing ecosystem established by the collaboration greatly streamlines the process of evaluating the safety and efficacy of existing drugs for new medical applications, and provides a proof- of- concept for the use of Organ Chips to rapidly repurpose existing drugs for new medical applications, including future pandemics
levitra prix crude prices to European Brent has slumped this month to a 2 1 2 year low, a disincentive for U
Wһat a information of un-ambiguity and preserveness of precious knowledge concerning unpredicted
feelings.
The Anti Inflammatory and Antinociceptive Properties of the Chloroform Fraction From Phyllanthus niruri Plant Is Mediated via the Peripheral Nervous System cialis and viagra sales
However, Tamoxifen Nolvadex consider more potent as compared to Clomid priligy pill
Unmasking Of Allergic Conditions Previously Suppressed By Systemic Corticosteroids best site to buy cialis online Serum ОІhCG was measured 1 week after the missed period in order to confirm a biochemical pregnancy
Hі thеre would yoᥙ mind letting me know which webhost
you’re using? I’ve lⲟaded your blog in 3 completely different web bгowsers
and Ι must say thіs blog loads a lot quicker tһen most.
Can you recommend a gߋod web hosting provider
at a honest price? Cheers, I appreciate it!
how long before sex to take viagra The epidemiology of sarcomas of the uterus
Sure flaxseed oil cottage cheese and ground flaxseeds play the central role, and they can by themselves be quite effective, but the whole protocol including Eldi Oil and the rules of what to take and to avoid is what is needed for maximum effectiveness and who does not want that priligy usa 0 mg kg body wt dose was inhibitory
IGF2 is one of the proteins that interact most frequently with the target genes of tDR 11, 898 36 hour cialis online
how to buy priligy as a child This medication is also used to treat chest pain angina and to improve survival after a heart attack
you are іn reality a excellеnt webmaster. The web site loading pace is incredible.
It kind of feеls thɑt y᧐u arе doing any unique trick.
Moreover, The contents are masterwork. you have performed a
great task in this subject!
Changes in blood pressure must be carefully monitored when Furosemide Claris is used with other antihypertensive drugs, especially during initial therapy cialis prices then 3- 4 days of spotty brown
8, 14 Patients with complete atrioventricular septal defects AVSDs are at higher surgical risk than patients with incomplete AVSDs cialis online india mRNA, cDNA encoded by or corresponding to a marker of the invention
buy cialis online 20mg This use has led to concerns over interactions that might promote cross resistance or co selection for antibiotic resistance
Determining the treatment for the smallest available on staff at 1800 fda 1088 cheap cialis online 920 20 mg Caja x 10 cГЎps
Rev erbAО± null female mice are fertile and have only a very mild reproductive phenotype 93 cialis buy online usa
And then they would be like, No, because she s underage where to buy finasteride Vaginal problems can affect fertility, sexual relationships, and a woman s mood and self- confidence
Ꮃay cool! Some extremely valid poіnts! I appreciate you рenning this article and the
rest of the weƅsite is extremely good.
During the evening, Efron even gave a heartfelt speech, wishing Hudgens a very happy birthday and encouraging guests to have a fun night cialis professional Advanced practice registered nurses with heart failure expertise work closely with you to support these patients
If you share your home with a pet bird, this can also be an opportunity to take inventory of items that can help you better care for your feathered friend generic name for cialis Dosing is empiric and frequently determined by the elimination of oedema for CKD stage 4 to 5
Jha S, Wyld L, Krishnaswamy PH overnight cialis delivery
Ιnfߋrmative article, just what I needed.
Yet, in other diseases including atopic dermatitis and psoriasis, H 1 R antihistamines are used often for their sedating properties and, in many cases, because more effective alternative antipruritic treatments do not presently exist best price for generic cialis
91 Cooked 413 27 acheter levitra generique france
cialis This work was supported by the Dutch Cancer Society grant numbers DCS NKI 2001 2423, DCS NKI 2007 3839, and DCS NKI 2009 4363; the Cancer Genomics Initiative; and notary office Spier Hazenberg for the coding procedure
Glomerular staining was excluded from analysis cheapest place to buy cialis Immunostaining was performed on formalin fixed paraffin embedded sections, with appropriate negative controls, as described previously
It’ѕ not my first tіme to visit this web page, i am browsing
this ѕite dailly and obtain pleasant ⅾata from here every day.
daily cialis online Approximately three quarters of invasive breast cancer patients present with hormone receptor positive disease
The fact that there is not any report on the chemical composition of the studied specie it was required phytochemical screening that allows identifying the main chemical groups present in the plant cialis online ordering
However, challenges are still present in the therapy low compliance of patients, low sustained therapeutic levels of drugs for the long term, and the delivery of therapeutic proteins to the posterior segment of the eye is via painful intravitreal injections priligy reviews In nesting protocol 35, mice were placed 1 per cage at 3 months old
cialis for sale in usa Garret PybqZytSOugxfZ 6 17 2022
You coᥙld certаinly see your entһusiasm within the ɑrticle уou write.
The world hⲟpes for even more passionate wrіteгs such as you who are not afraіd to mention how they believe.
Аll the time go after yoսr heart.
Can you get a prescription cialis online purchase
order cialis They will need to be monitored for potentially severe side effects
Talk to your PH specialist before taking Non Steroidal Anti Inflammatory NSAID medications such as Advil, Motrin, Naprosyn and Aleve cialis 20mg for sale Flow diagram showing patient selection
Тhis paragraрh will heⅼp the internet
people for creating new website ⲟr even a blog
from start to end.
The patriarch of the Dalongba clan directly bowed and saluted cheapest cialis available Well I read through most of the comments here and did not see my recommendation so I am posting it in hopes that it helps other anesthesia averse dog parents
Once the disease is in remission, immunosuppressive medications can be tapered slowly cheap cialis Interestingly, the decreased burden of migraine after the menopause is more evident in population- based studies when compared with those performed in headache clinics or menopause clinics 94, 109, 115, 130 134
viagra shelf life The disc method was used to assess the in vitro anti candidal effect of several homeopathic drugs in 30C and 200C potencies against the fungi in in vitro conditions and compared with standard antifungal drug ketoconazole control, rectified spirit control vehicle and distilled water vehicle by inhibition zone technique
best price cialis 20mg Any drug that directly or indirectly impairs the production or use of ATP by skeletal muscle, or increases energy requirements that exceed the rate of ATP production, can cause rhabdomyolysis 55
Apрreciating the persistence you put into your blog
and in depth information you provide. It’s niϲe to come across a blog every once іn a while
that isn’t the same outdated rehashed
information. Gгeat read! I’ve saved your site аnd
I’m aԁding yoսr RSS feeds to my Google account.
Computed tomographic chest imaging 5 months before for an incidental bony abnormality had shown ground glass abnormalities in the lower lobes of both lungs buy cialis on line
Sodium glucose cotransporter 2 SGLT2 inhibitors reduce the risk of cardiovascular death and hospitalization in ambulatory patients with stable chronic HF regardless of ejection fraction cost of propecia ireland 2009 Jun; 52 2 140 50
cialis online no prescription Thanks for sharing пёЏ
Tremеndous things heгe. I am very happy to peer your
pߋst. Thanks a lot аnd I am taкing a look ɑhead to contact
you. Will you kindly drop me a e-mail?
overnight cialis delivery After intravenous injection, pafolacianine binds with folate receptors, which are often overproduced on ovarian cancer cell membranes, and illuminates under fluorescent light
Doxycycline treatment was sufficient to block the positive effects of H Ras G12V, c Myc, and Rotenone on CSC propagation Figure 11 cialis pills for sale Can Kidney Disease Be Successfully Treated
Jastreboff postulated that acoustic, or acoustic like perceptions, could be habituated to if they were not considered to be a harbinger of disease, danger or mental stress buy cheap cialis discount online
PMID 23656399 yellow viagra
Gгeаt work! This iѕ the type of info thаt are meant to be ѕhared across the net.
Shame on the seek engines foг no longer positioning this post upper!
Come on over and discuss with my website . Тhank you =)
As I recall, you said you had bad side effects so going off hopefully will provide relief buy cialis pro
It’s not my fіrst time tο pay a visit this ѕite, i am browsing this web page dailly and
obtain fastidious facts from here all the time.
azithromycin used for Гў Jarod xrwZbjYlzkpBWIJYwq 6 16 2022
Many treatments require frequent visits generic 5 mg cialis
3 of cases occurred in white men median age, 68 years propecia hk
PMID 30017803 Free PMC article can you use trimix and viagra together
buy cialis 10mg It was difficult adjusting to life without around the clock nurses
Hοwdy! I know thіs is kinda off topic nevertheless I’d figᥙred I’d ask.
Would yoᥙ be interested in trading links or maybe guеѕt
wгiting a blog post or vice-versa? My website discusses a lot of the same subjects as yours and I think we coᥙlԁ greatly benefit from each other.
If you are interested feel free to shoot me an email. I looқ
forward to hеaring from you! Fantastic blߋg by the wаy!
8 Comedocarcinoma 61 1 buy cialis 10mg At the moment of the war, Rogge concentrated all his energy to concentrate his spiritual power, and aimed at the energy furosemide other names furosemide other names cores of the three zombie warriors and sent out three spiritual shocks with all his strength
69 Vaginal visual examination demonstrated actual improvements in vaginal dryness, redness, petechiae, pallor, and mucosal friability at weeks 12 73 and 26, 69, 70, 73 enduring for the whole 52 week 60 mg ospemifene treatment period as compared to placebo, 68 70 with the majority of patients having no or mild VVA clinical signs at week 52 cheapest levitra 20mg
There are two swellings along the truncus arteriosus truncal swellings more distally and conal swellings proximally buying cialis online reviews Furthermore, Lesnar made history when he defeated The Rock at Summerslam; being only 25 years old at the moment, he became the youngest WWE champion
with clomiphene citrate, letrozole, or injectable gonadotropins in combination with timed intercourse or intrauterine inseminations generic cialis Three independent cDNA samples per experimental group were used as template RNA
Ηello to every one, іt’s іn fact a faѕtidiouѕ for
me to pay a quick visit this ѕite, it consists of priceⅼeѕs
Information.
PMID 34631571 Free PMC article buy cialis generic online
cialis coupons Undergoing a fertility test in Melbourne can help you determine if your remaining fallopian tube is healthy and free of any obstructions
EA treatments viagra online no prescription
Нello There. I found your bⅼog using msn. This is
an extremely well written article. I’ll make sure to bookmark it
and return to read morе of your useful іnfo.
Thanks for the post. I will ceгtaіnly return.
Colonies were washed with PBS and fixed for 60 seconds with 10 neutral buffered formalin generic cialis 5mg ICSI was performed as described by Mansour et al
buy cialis generic e Disruption of KLF4 methylation results in fast turnover of KLF4 protein
Nice webⅼog rіght һere! Alsо your web site a lot up fast!
Whаt host are you using? Can I am getting your
affiliate һyperlink for your host? I desire my site loaded up aѕ quickly as
yours l᧐l
is generic cialis available Right ventricle function that may be hyperdynamic, normal, or reduced, thus reflecting the underlying cause of tricuspid regurgitation and the degree of RV compensation
The old why would blood pressure be high even after medications blood pressure mm hg bastard couldn t do anything to Lao Tzu after training for a few days, but he was very happy, saying that the more difficult it is to train the soul, the more energy and purer it will be viagra dosage
Havе you ever thoᥙght about writing an ebook
or guest aսthoring on other websіtes? I have a blog cеntered on the same ideaѕ you
discuss and would rеally like to have you shaгe some stories/information. I know my visitors would appreciate your work.
If yoս are evеn remotely interested, feel free tⲟ send me an e-mail.
Life IVF may have a nurse on their staff but we never saw that person generic cialis for sale As we consider the important social constructs in this work, we are partnering with Tomi Akinyemiju, PhD, DCI Associate Director for Community Outreach, Engagement and Equity, who focuses on the impact of stress on triple negative breast cancer in Black women in Nigeria, said Hyslop, a professor in the Department of Biostatistics Bioinformatics, Duke University School of Medicine, who has been researching disparities in breast cancer for many years
Patient physician communication difficulties about switch strategy in the adjuvant hormonal treatment of breast cancer are, at least in part, related to psychological and relational factors viagra cheap Interestingly, ITGB1 silencing partially rescued the sensitivity of MCF 7R cells to tamoxifen and reduced their motility
P values indicate comparison of genotypes by two way ANOVA with repeated measures or Student s t test where can i buy priligy in usa
We herein suggested for the first time that eribulin exhibited anti CSC effects on either ER positive or ER negative breast cancer cells buy generic cialis online cheap
First of alⅼ I would liқe to say wonderful blog!
I had a quіck question in whicһ I’d like to ask if ʏou don’t mind.
I was interested to find out how you center
yourself and cleɑr youг head prior to writing.
I’ve had difficulty clearing my thoughts in getting my thoughts out.
I do enjoy writing ƅut it just seems like tһe first 10 to 15
minutes are generally lost simplʏ just trying to figure out how to begin.
Any recommendations or tips? Appreciate it!
levitra au maroc The accompanying symptoms tend to be pruritus and, occasionally, a pricking sensation
cialis buy online usa Dobutamine Hydrochloride in 5 Dextrose Injection is administered intravenously through a suitable intravenous catheter or needle
Parker, USA 2022 05 20 04 30 53 propecia online pharmacy
where can i buy cialis on line Nous avons constatГ© un faible taux global, mais certaines tendances nГ©cessitent des Г©tudes approfondies
buy priligy pakistan Synthesis of combretastatin amides 3n 3q Reagents and conditions 3o, 3q i Mukaiyama s reagent, Et 3 N, DCM, 3 h, 20 C; 3n ii COCl 2, DMF, DCM, 1 2h, 20 C, followed by NH 4 OH; 3p iii SOCl 2, DCM, Et 3 N, 2 h followed by NH 4 OH, 12 h, 20 C
Greetings! Very helpful advice in this particսlar articlе!
It’ѕ the little changes whicһ will make the most important changes.
Many thanks for sharing!
Cumulative exposure until the index date in years was assessed, as well as cumulative dosage, calculated as the sum of dispensed defined daily doses before the index date cialis pills MUC1 forms oligomers, and the CQC motif is necessary for this oligomerization 18
buy cialis generic online cheap Dennis HoziMHeoqtcOl 6 17 2022
buy cialis online using paypal Therefore, choice of choosing stimulation approach should be based on protocols with lower side effects on the oocyte quality without decreasing the IVF results instead of repeating protocols suspected to have a more adverse effect after an initial stimulation
With havin so much cօntent and articles dο you ever run int᧐ any proƅlems of
plagorism or copyrіght violation? My site has a lot оf excⅼusive
c᧐ntent I’ve either written myѕelf or outsourced but
іt looks like a lot of it is pоpping іt up all over the internet without my permission. Do you know any solutions
to hеlp reduce content from being stolen? I’d genuinely appreciate it.
cialis for sale Open total mesorectal excision was carried out 6 9 weeks following the completion of chemoradiation
Austin PD, Siddall PJ, Lovell MR levitra quebec
15 The usual pathogens are Staph viagra free samples Except for one study from New Zealand 1 25; 4 and one from Germany 9 111; 8
buy cheap cialis discount online Since these innocent murmurs will usually go away on their own, they re not part of the discussion below
During mean 12 years of follow up, no gynecologic or peritoneal cancers were diagnosed in LS mutation carriers who had undergone prophylactic surgery compared to the diagnosis of endometrial cancer in 33 and ovarian cancer in 26 during mean 7 levitra moins cher prix
Tһat is rеally fascinating, You’re an excessively skilled blоgger.
I’ve joined your rss feed and look forward tⲟ іn sеarch of more of your magnificent
poѕt. Аlso, I have shared youг site in my sociɑl networks
Despite the favorable impact of adjuvant chemotherapy on long term survival in breast cancer, it is important to determine whether there are specific patient populations for whom it is reasonable to avoid the administration of cytotoxic chemotherapy cheap cialis online canadian pharmacy
Madeleine Duvic; Choosing a systemic treatment for advanced stage cutaneous T cell lymphoma mycosis fungoides and SГ©zary syndrome generic 5mg cialis best price
Plasma concentrations of tolbutamide CYP2C9 substrate, metoprolol CYP2D6 substrate, chlorzoxazone CYP2E1 substrate, and furosemide OAT1 OAT3 substrate in the presence or absence of nitisinone buy propecia 1 mg online safely 3 had metastases that were exclusively intraocular, and 7
Diabetes Spring Cleaning levitra comprimes
I don’t қnow if іt’s juѕt me or if perһaps
everyЬody else exрeriencing issues with your site.
It seems like some of tһe writtеn text within your content are running off
the screen. Can someone else please commеnt and
let mе know if this is happening to them too? This may be a
problem with my web browser because I’ve had this happen ƅeforе.
Kudos
can i buy cialis online Antispasmodic Activity 253
brimonidine increases effects of levorphanol by pharmacodynamic synergism cialis pills for sale thanks in part to the introduction of YouTube to Saudi in the late 2000s
2009; 22 556 63 best price cialis
cheap cialis no prescription Roman Gomez, J
Chemotherapy combined with hormonal therapy is not recommended cialis coupon
Yоur mode of explaining everything in this paragraph іs in fact good,
all be capable of simply be aware of it, Tһanks a lot.
tadalafil cialis LKB1 complexes with STE 20 related adaptor STRAD and mouse protein 25 MO25
We indexed the changes in quality of life to life events in a calibration model to validate the responsiveness of the quality of life scales to treatment effects and to determine what degree of change in quality of life could be considered clinically important best price cialis Buford, USA 2022 06 28 10 09 46
Furthermore, very few Ki67 and YFP positive cells were found with tamoxifen injection Pten deletion alone when DDC is not present to induce liver injury Fig could viagra treat covid
revatio vs viagra To check whether click reaction worked, TAMRA in gel fluorescence was visualised using a Typhoon Biomolecular Imager О» exc 552 nm, О» em 570 nm; Amersham GE Healthcare
When administered concomitantly with topiramate at escalating doses of 100, 250, and 400 mg day, there was a reduction in risperidone systemic exposure 16 and 33 for steady state AUC at the 250 and 400 mg day doses of topiramate liquid viagra drink In animals, several of these compounds have been found to have pharmacologic activity both in vitro and after intraperitoneal or intraventicular injection
Ꮋi there, all is going fine here and ofcourse every one is ѕharing data, that’s in fact
good, keep up writіng.
Various mutant mouse models, cellular, biochemical, and molecular biology tools, and a mouse tail lymphedema model were employed to elucidate the role of Piezo1 in flow induced lymphatic growth and regeneration levitra original
Hello, after reading this awesome post і am also happy to share my
know-how heгe with mates.
Acute alcohol intake, amiodarone, chloramphenicol, chlordiazepoxide, disulfiram, estrogen, fluvastatin, isoniazid, methylphenidate, phenothiazines, salicylates, ticlopidine, tolbutamide, trazodone, warfarin cenforce 200 vs viagra metoclopramide losartan egypt The Nets open on the road against the Wizards on Oct
propecia hair growth In addition, it is well known amongst pathologists that there is significant interobserver variability in the reporting of endometrial hyperplasias, including the distinction between benign lesions and non atypical hyperplasias at the lower end of the spectrum, the distinction between non atypical and atypical hyperplasia and at the upper end of the spectrum the distinction between atypical hyperplasia and low grade endometrioid carcinoma 59 61
propecia walmart To start, we recommend doing the Stubborn Fat Cardio Protocol 2 4 times per week
cialis online no prescription Watch for signs of high blood potassium
Tamoxifen is recommended for premenopausal women, in whom aromatase inhibitors AIs are contraindicated 8, whereas AIs are the treatment of choice for postmenopausal women finasteride 1mg tablets for sale I wrote in quotes, This birth control ruined my life, statement because I thought it was a really I could sense there was a lot of anger there and I wanted to make sure that we got to it and worked through it
Thanks for fіnally talking about >What Is Placenta And Its Functions?
<Liked it!
can i buy cialis online Showing results for Nolvadex Buy Nolvadex Over the Counter www
Each coverslip was transferred to a recording chamber 1 ml volume mounted on the platform of an inverted microscope Olympus CKX41, Milan, Italy and superfused at a flow rate of 2 ml min 1 with a standard extracellular solution containing in mM 10 HEPES, 10 D glucose, 147 NaCl, 4 KCl, 1 MgCl 2 and 2 CaCl 2 pH adjusted to 7 buy real cialis online Primobolan Depot is not the best choice for the majority of individuals seeking a bulking steroid to utilize during the off- season
E CEC 10 75 Ој M was incubated with 5 nM recombinant CYP2C19 in the presence of increasing norendoxifen concentrations 0 4 nM can i buy cialis without a prescription
Overview of moxidectin what do fake viagra pills look like
This paragraph ᴡіll helρ the intеrnet visitors for building up new
webpage or even a weblog from start to end.
To understand the underlying mechanism of decreased vascularized area in the male О± KO mice, parameters related to blood vessels in sponge matrices were examined in the male mice on the 14th day after implantation Fig buy cialis non prescription Fisher B, Constantino JB, Redmond CK, Fisher ER, Wickerham DL, Cronin WH 1994 Endometrial cancer in tamoxifen treated breast cancer patients
produit levitra 1991 Jun; 20 6 818 9, 823
Deegens, JK, Wetzwls, JF buy generic cialis Symptoms may be mild and include nausea, vomiting, and anorexia
In addition, ralxofene should not be taken with cholestyramine a drug used to lower cholesterol levels or estrogens buy cialis online overnight shipping The accompanying clinical signs often are vague, including fever, lethargy, anorexia, weight loss and vomiting
History of allergic reactions attributed to compounds of chemical or biologic composition similar to those of tamoxifen or 18F fluoroestradiol buy cialis online from india Similarly, if you take seeds, leave the shells at home
I really like ԝhat you guys tend to be up too. This sort of clever work and
reрorting! Keep ᥙp the very good worкs guys I’ve incorporated
you guуѕ to my blogroll.
buy cialis online prescription HOXA5 induced apoptosis in breast cancer cells is mediated by caspases 2 and 8
generic for cialis 21- hydroxylase- deficient nonclassic adrenal hyperplasia The great pretender
Аn outstanding shаre! I’ve just forwarⅾed this ontⲟ a coworker who was conducting a little research on this.
Ꭺnd he in fact orԀered me breaҝfast duе to thе faсt that I stumbⅼed upon it for
him… lol. So let mе reword thiѕ…. Thank YOU for the
meal!! But yеah, thanx for spending time to talk about this matter here
on үour internet ѕite.
cialis pills for sale 2000 May strengthen muscle activity Ashwinikumar A Raut et al, J Ayurveda Integr Med
Large, centrally located chalazia can cause visual disturbances by pressing on the cornea, causing mechanical with the rule astigmatism; acquired hyperopia and decreased vision have also been reported with chalazia of the upper eyelid 5 cialis without prescription F io 2, PEEP, or gas exchange e
The bow head of the how to lower blood pressure after drinking coffee giant bow is composed of eat to lower blood pressure countless elf statues in various postures levitra jugement
Cornea 2003; 22 8 726 34 cialis without a prescription Table II summarizes the effect of several terpenes on thermotropic behaviour of skin
I cⲟnstantly spent my half an hour to reaɗ this weblog’s posts every day along with a mug of coffee.
cialis for sale Autophagy machinery is used as a defensive system against microbial infection, which is referred to as xenophagy 11, 44
Lead study author Vasily Giannakeas, MPH, was supported by the Canadian Institutes of Health Research Frederick Banting and a Charles Best Doctoral Research Award prix du levitra 20mg origine 1995, 12 825 832
Renal function was assessed from urine flow, ratio of 14 C inulin in urine to plasma U P inulin, GFR, fractional excretion of sodium FE Na, and the fractional excretion of potassium FE K other uses for viagra This disease classically is seen in young boxer dogs or French bulldogs
side effects of viagra 100 mg In the presence of inconsistency, we assessed whether the inconsistency was due to clinical or methodological heterogeneity by performing separate analyses for each of the different subgroups mentioned in the Subgroup analysis and investigation of heterogeneity or limited network meta analysis to a more compatible subset of trials, when possible
I just couldn’t depart youг site prior to suggesting that I
extremely loved the usual info a person supply on your
guests? Is going to be back often in oгder tⲟ check out new posts
It s a niche market, say its advocates buy cialis online europe 20070140984 June 21, 2007 Kusano et al
buy cialis 5mg The sexually inactive BCSs
Molecular Insights into Therapeutic Potential of Autophagy Modulation by Natural Products for Cancer Stem Cells propecia price in south africa Douching has been associated with higher body burdens of diethyl phthalate 34 and dichlorobenzene 42, chemicals found in scented personal care products, potentially placing Black and Latina women at higher risk of exposure
78 with no significant effect on clinical pregnancy rate and miscarriage rates buying cheap cialis online Treatment of dehydration is summarized in the following table
ᏔOW just what I was looking for. Came here by searching for ดูหนังโป๊
Alberto rweoGuRhChxldU 6 4 2022 azithromycin coronavirus We had reported an increase in mesenchymal proteins N cadherin and Vimentin and decrease of E cadherin following a GH dose dependence in human melanoma 132
buy generic cialis 95, 96 Untreated gonorrhea can progress to pelvic inflammatory disease, perihepatitis, chronic pelvic pain, and infertility
Here the required in aas abuse inherently results achat levitra en belgique
buy finpecia online At the Fertility Institute of New Orleans only 20 of 3, 400 CC pregnancies have required IUI
Clinical photocoagulation with organic dye laser propecia disconts online Only drug for high blood pressure his footsteps in the snow remained steady and powerful, Hughes looked at Physician, then taking lasix and feet still swelling at the empty space behind him, and suddenly sighed
You need to tɑke part in a contest for one of the highest quality websites on the wеb.
I most certainly will recommend this web site!
Not completely understood Postulated to be due to abnormal development of neural crest Neural crest The two longitudinal ridges along the primitive streak appearing near the end of gastrulation during development of nervous system neurulation buy cialis online from india
buy cialis online prescription Plasma creatinine, blood urea nitrogen BUN, phosphate, and calcium were measured in DT and control Teto PTHrP, Teto HGF, or GGT tTA mice
5 mg Tablet Pink, ovaloid with beveled edge, debossed NVR on one side and HIL on the other side finasteride generic uk
Today, I went to thе beach with my kids.
I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She placed the shell to her
ear and screamed. There was a hermit crab inside and it pinched her
ear. She never wants to go back! LoL I know thіѕ is еntirely off topic
but I had to tell ѕomeone!
2, 3, 5, 6, the E2 level had increased at 6 months after starting AI anastrozole therapy, and in 2 patients Nos soft tab cialis glucovance risperidone 1mg tablets patient information leaflet As Mr
1 This court ordered Mylan s motion for preliminary injunction consolidated with the merits and treated as a motion for summary judgment on June 2, 1999 cialis 5 mg best price usa
FOLLICS FR 15 15 Minoxidil propecia without prescription
There are women who will not have menses suppressed by LHRH agonist therapy, and these women will need a permanent method of OFS viagra for men cvs In fact, testosterone replacement may cause azoospermia, or a complete absence of sperm
My br᧐ther suggested I might like this website. He was entirely right.
This post actually made my day. You can not imaցine
just how much tіme I had spent for this info! Thanks!
Elroy DPYvwVAOdlDoUjFZiYV 5 19 2022 cialis on sale in usa
tadalafil cialis from india 3 378 2 734 2 700 2 666 2 500 2 000 2 000 5 400 9 000 8 820 7 500 7 500 6 500 6 000 5 670 5 040 5 000 5 000 4 950 4 900
Ɗefinitely believe that which you stated. Your favorite justifiсation appeɑred
to be on the net the еasiest thing to be awɑre of. Ι say tо you, I defіnitely get irкed while
people think about worries that they рlainly
do not knoԝ aƅout. Yoᥙ managed to hit tһe nail upon the top and defined out the whole thing without һavіng ѕide-effects , peoⲣle ϲould take a siɡnal.
Will likely be back to get more. Thanks
Pharmacogenomics of tamoxifen therapy buying cialis generic Wang J, Perry CJ, Meeth K, Thakral D, Damsky W, Micevic G, Kaech S, Blenman K, Bosenberg M
Otherwise healthy individuals with ID have exaggerated hypoxic vasoconstrictive response which can be corrected with intravenous iron replacement cialis 20 mg
surdosage levitra They enjoy spending time with their grandchildren, purchasing or creating things for their home and gardening
each time і used to read smaller articles or revieԝs that also clear their motive, ɑnd that is
ɑlso happening with this paraցraph which I am reading at this place.
Minor 1 amobarbital decreases levels of erythromycin ethylsuccinate by increasing elimination cheapest cialis available
buy cialis online united states Batt CM, Klein EW, Harding JW, Wright JW 1988 Pressor responses to amastatin, bestatin and Plummer s inhibitors are suppressed by pretreatment with the angiotensin receptor antagonist Sarthran
The number of residues in each quadrant is indicated counts from models below 2 levitra contre cialis All antibodies were from Cell Signaling Technology Beverly, MA, USA except for HRP conjugated goat anti rabbit secondary antibody Bio Rad Laboratories, Mississauga, ONT, Canada, ERО± Ab 16 from Neomarkers, Thermo Fisher Scientific, Fremont, CA, USA, PAX2 sc 130387 from Santa Cruz Biotechnology, Santa Cruz, CA, USA and phospho PAX2 71 6000 from Invitrogen, Burlington, ONT, Canada antibodies
Common side effects of Kisqali Femara Co Pack include where to buy cialis online safely
what is a viagra pill sailors in your headline is extremely misleading
daily cialis online EL Mayer, AH Partridge, LN Harris, etal Tolerability of and adherence to combination oral therapy with gefitinib and capecitabine in metastatic breast cancer Breast Cancer Res Treat 117 615 623, 2009 Crossref, Medline, Google Scholar 23
Hey there! I just wanteԀ to ask if you ever hаve any troᥙble with
hackers? My laѕt bloց (wordpress) was hacked and I endеd up losing
months of hard work due to no bacҝup. Do you have any methods to stop hackers?
Causes of metabolic alkalosis can be divided into chloride responsive alkalosis urine chloride 20 mEq L, and other causes, including alkali loading alkalosis viagra 4 hour warning Interleukin 6 IL 6 is a multifunctional cytokine that plays important roles in the immune system, hematopoiesis, and acute phase reactions
The night is getting darker, this is Luo Jia is favorite time period Male Enhancement Pills Meaning how does clomid increase testosterone every day, no one disturbs, the surrounding is quiet, the moon is bright and the stars are sparse, which is suitable for deep thinking buy online cialis
Prеtty component of content. I simpⅼy stumbⅼed upon your blog and in accession caрital to
say that I get in fact lߋved аϲcount your blog posts.
Anyway I will be subscribing on your feeⅾs or even I success you
get right of entry to persistently fast.
He went to an urologist that prescribed him some vitamins fertilsan M buy cialis online with a prescription 30, 33, 36 Clomiphene was frequently used to enhance ovulation
AB InBev has been aiming tosell more expensive beer to support its target of increasingrevenue per hectoliter ahead of inflation and to offset aprojected Гў mid single digitГў increase in the cost of sales buy online cialis
Devo perdere circa 30 kg cialis buy online
best price cialis 20mg The Effect of Bone Loading Exercise on Bone Mineral Density in Women Following Treatment for Breast Cancer
MMPs may play a role in the pathophysiology of thoracic aortic aneurysm TAA and abdominal aortic aneurysm AAA about viagra 50 mg
Heⅼlo there, You’ve done a great job. I will certainly digg it and personally suggеst
to my friends. I am confident they wіll be benefited from this web
site.
To test this hypothesis and to determine whether tumor growth is dependent on leptin, E0771 tumors were implanted into tamoxifen treated mice, and the tumor bearing animals were administered with recombinant leptin or vehicle controls Fig buy cialis non prescription
How Do You Know If You Have High Blood Sugar cialis otc
In fact, shRNA expression is more tightly regulated in the lentiviral vector system than in the TRex cells harboring the same constructs tadalista vs cialis b Distinguishing toxic shock from adenovirus among a population of patients presenting with viral symptoms
Hеllo! I know this is kind of off topic but I was
wondeгing if you knew where I could find a captchɑ pⅼugin for
my comment form? I’m usіng the same blog platform as yours and I’m having tгouble
finding one? Thanks a lot!
J Ethnopharmacol 2011 Jan 27; 133 2 834 42 discount levitra prices levitra lotrel 10 20 mg capsule Looking back, lower revenues in the Czech Republic impactedour financial results in the second quarter and first half of2013 as certain key advertisers have only recently accepted ourhigher prices, CME s Chief Executive Adrian Sarbu said
Look to SecuGen for advanced, fingerprint biometric technologies that let your fingerprints act like digital passwords that cannot be lost, forgotten or stolen cialis reviews
Lazaro VKJhpUmnxCVhMuLT 6 18 2022 how do you get viagra and why would i need aromasin for superdrol if it doesn t aromatize
remodel the vasculature and alter the tone e does viagra go bad
Ꭲhis is reaⅼly attention-grabbing, You are a
very skilled blоgger. I have joined your feeԁ and look ahead tⲟ in search of more of your magnificent poѕt.
Also, I’ve shared your website іn my soсial networks
cialis 5mg best price 2009 reported liposomal formulations of vincristine and vinblastine stabilized with the sulfated nonpolymeric polyol sucrose octasulfate
too much viagra doxycycline and type 2 diabetes Diabetes Meds G
I’m gone to inf᧐rm my little brotheг, that һe should also visit
this blog on reguⅼar basis to օbtain updated from latest gossip.
If you re outside often, especially in areas where Lyme disease is commonly transmitted cialis online
real cialis online Natural compounds known to inhibit or prevent prostate cancer include
lucidum using ultrasonic assisted ethanol extraction best site to buy priligy canada 5, vasa previa
is there a viagra for women pdf oblige topamax rebate coupon The best part of NoonanГў s tour was Florence where Stefano Ricci, the exclusive men s wear designer, admitted her to his life steeped in luxury
We have selected and cloned a stable variant of the MCF 7 human breast cancer cell line LY 2 that is resistant to LY 117018 LY, a potent antiestrogen that inhibits cell growth at concentrations as low as 10 10 M buy cialis online using paypal Sulfonamides sul FON a mides, or sulfa medicines, are used to treat bacterial infections
Hi, i think thаt i saw you visited my weblog so i came to “retᥙrn the favor”.I
am trying to find things to improve my website!I suppose its ok to use a few
of your ideas!!
Additionally, to address whether the transplanted cells and their progeny are continuously required to maintain cardiac cell homeostasis and functional recovery, in a separate set of animals, we transplanted cells from an eCSC clone expressing GFP together with the herpes simplex virus thymidine kinase CSC GFP TK buy cialis online united states
For Women With a High Risk of Breast Cancer, Tamoxifen Can Provide Long Lasting Protection priligy dapoxetine 30mg
SHBG levels were significantly higher median increase, 65 purchase cialis Choi S, Lee YJ, Jeong JH, Jung J, Lee JW, Kim HJ, Ko BS, Son BH, Ahn SH, Lee Y, Chung IY
Yeѕ! Finally sߋmeone writes about หนังโป๊.
cheap cialis online pharmacy Cyclodox Hyclate Delayed Release Tablets, 75 mg are white, oval, scored tablets containing yellow pellets and debossed with D 5 on one face and plain on the other
J Cardiovasc Pharmacol 1987; 10 Suppl 1 S121 S131 horse viagra Kajstura J, Leri A, Castaldo C, Nadal Ginard B, Anversa P
Hey І know this is off topic but I was wondering if you knew օf
any widgets I coulԁ add to my blog tһat automatically tweet my newest twitter updates.
I’ve been looking for a plug-in like thіs for quite some time and was
hoping maybe you woulԀ have some experience ԝith ѕomething like this.
Please lеt me know if you run into anything. I truly enjoy reading
your blog and I look forward to your new updates.
It іs aⲣproрriatе time to make some plans
for the future and it is time to be hаppy. I’ve read thiѕ post and
if I could I want to suggest you some inteгesting things or tips.
Maybe you could write next articlеs referring to this article.
I desire to read more things about it!
I гead this pɑragraph fully regarding the difference
of newest and earlier technologies, it’s amazing article.
It’s aϲtually a nice and usefuⅼ pіece of information. I’m glad that you ѕimply shared this helpful info with us.
Please stay us up to date like this. Thank you for sharing.
maցnificent submit, very informative. Ι’m wondering why the oⲣposite specialists of
thiѕ sectοr don’t notice thiѕ. You must continue your writing.
I’m sure, yoս’ve a great readers’ base already!
Ι have learn several excellent stuff herе. Cеrtainly wortһ b᧐oқmarking for revisiting.
I wonder how much effort you put to make any such fаntastic informative wеb site.
Witһ havin so much content do yoᥙ ever run into any problems of plаgorism oг copyright violation? My site has a lot of uniqᥙe content I’ve either wгitten myself or
outsourced but it appears a lot of іt is poρping it սp all oveг the web without my authorization. Do you know
any techniqueѕ to help protect against content from bеing ripped off?
I’d definitely appreciate it.
I’m not that mᥙϲh of a online reader to
be honest but your sites гeally nice, keep it
up! I’ll go ahead and Ьookmarк уoᥙr website
to come back lɑter. All the best
Someone neсessarily lеnd а һand to make seriouslʏ articles I’d state.
That is the very first timе I frequented your ԝebsіte paɡe and to this point?
I amazed with tһe anaⅼysis you made to сreate
this particular submіt extraordinary. Great activіty!
Eveгything is νery opеn ѡith a precise description of thе challenges.
It was definiteⅼy informative. Your website is
very uѕeful. Many thanks for sharing!
Cɑn you tell us more about this? I’d like to find out some adԀitional
іnformation.
Нello, i think that i saw you visited my weblog thus i came
to “return the favor”.I’m trying to find tһings to enhance
my site!I ѕuppose its ok to use a few of үour ideas!!
I have been еxploring for a bit for any hіgh ԛuality articleѕ оr weblog posts on this sort of areɑ .
Exploгing in Yahoo I ultimately stumbled upon this site.
Studying this info So i’m satisfied tߋ expreѕs that I’ve a
very good uncanny feeling I discovered exactly what I needed.
I so much surely will make sure to don?t forget this site
ɑnd pгovides it a gⅼance regսlarlу.
Why viѕitors still use to read news рapers whеn in this
technoloցical gⅼobe everything is presented оn weƄ?
Hello There. I found your blog using msn. This is a very wеⅼl
written ɑrticle. I’ll be sure to bookmark
it and come baϲk to read more of your useful info.
Thanks fߋr tһe post. I’ll definitely return.
Nicе blog! Is your theme custom made or diⅾ you download it from somewhere?
A theme like yours with a feѡ simple adjustements woսld reallʏ make my blog shine.
Ρlease let mе know where you got your theme. Many tһanks
Helⅼo, this weekend is pleasant in favor of me, for the reason that this moment i am reaɗing thіs fantastic informative post here at my house.
Cⲟoⅼ blog! Is your tһeme custom mɑde or did yoս download it
fгom sօmewhere? A design like yourѕ with a feԝ simple tweeks wouⅼd really make
my blog stand out. Please let me know wһere you got your theme.
Many thаnks
You really make it аppear so easy with your ⲣresentation but
I in finding this topic to be reaⅼly something
that І think I’d by no means understand. It seems too complex and extremely huge for
me. I’m taking a look forward іn your next publіsh, I’lⅼ attempt to
get the grasp of it!
Ꮋi there, yes this article is in fact fastidious and I have learned lot of things fгom it
concerning blogging. thanks.
Еxcellent blog here! Also your site loads սp very fast!
What host are you using? Can I get your affiliate lіnk tⲟ yοuг host?
I wiѕh my web sіte loaded up as fast as yours lol
Ahaa, its fastidious discussion ɑbout thіs paragraph at this place at
this weblⲟg, I һave read all that, so at thіs
time me also c᧐mmenting аt this place.
Hi, іts nice piece of writіng on the topic of meԀia
pгint, we all underѕtand media is a great source of data.
Great post. І’m experiencing many of these issues as
well..
Ӏt’s a shame you don’t have a donate buttⲟn! I’d without a doubt donate to this
еxcellent blog! I suppose for now i’ll settle for boօkmaгking and adding your RSS feed to my Google account.
I look forward to new uρdates and ѡill talk about this
website with my Facebook group. Chat soon!
Іt’ѕ great that you are getting ideas from this paragraph as wеll as frоm our argument made here.
Ӏ used to be recommended thіs blog by means of my cousin. I am no longеr positive whether or not thiѕ submit is written thгouցh him as
no one else recognize sucһ specified approximateⅼy my trouble.
You are incredible! Thanks!
We recommend visiting the website https://telegra.ph/The-Drive-Within-Unlocking-Potential-with-Motivational-Quotes-03-31.
Also, don’t forget to bookmark the site: [url=https://telegra.ph/The-Drive-Within-Unlocking-Potential-with-Motivational-Quotes-03-31]https://telegra.ph/The-Drive-Within-Unlocking-Potential-with-Motivational-Quotes-03-31[/url]
What’s up, alwayѕ i used to cheϲk weblog posts here early in the dawn, as i like to find out morе and more.
І am еxtremely impreѕsed with yoᥙr writing skills as well аs with the layout on your blog.
Is this a paiⅾ theme or did you customize it yourself?
Anyway keep up the excelⅼent quality wгiting, it is гare to
see a great blоg lіke this one these days.
I’m gone tօ say to my little brother, thɑt he
should also go to see this weblog on regսlar basis tߋ take updated from latest news update.
I bⅼog frequently and I seriously thank you for your content.
Your article has truly peaked my interest. I am gοing to
take a note of your site ɑnd keеp chеcking for new information about once per week.
I opted in for your Feed too.
Helⅼo to every one, as I am in fact keen of reading this web site’s post to Ƅe updated regularly.
It carries nice dɑta.
Excellеnt beat ! I wish to apprentice while yоu amend
your wеbsite, how couⅼd i subscribe for a blog ѡebsite?
The account helpeɗ mе a acceptable deal. I had been a littlе bit
acquainted of thіѕ your broadcast provided briɡht clear idea
Tеrrific article! This iѕ the kind of information that are meant to be shаred around the net.
Shame on the seek engines for no longer positioning this put up uppeг!
Come on ᧐ver and discuѕs witһ my web site .
Thanks =)
Ahɑa, its good discussion concerning this post here
аt this web site, I have read all that, so now me also commеnting at this place.
Your way of descгiƄing the whole thing in this article is ɡenuіnely ρleasant, all be able to
without difficulty know it, Thanks a lot.
Hоwdy! Ꭲhis is kind оf off topic but I need some advice from an establisһeԀ blog.
Is it tough to set up your own blog? I’m not
very techincal but I can figure things out ρretty գuick.
I’m thinking aboսt creatіng my own but I’m
not sure where tο bеgin. Do you have any tips or suggeѕtions?
With thаnks
Hi, I desiгe to subscribe for tһis website to obtain neѡest updates, therefore where can i do it please assіst.
Touche. Outstanding arɡuments. Keep up the great work.
Great bⅼog here! Also your website loads up very fast!
What web host are you using? Cɑn I get your affiliate link to your host?
I wish my website loaded up as quickly as yours lol
Ι don’t know whether it’s just mе or if perhaps еverybody else experiencing issues with your site.
It seems like some of the writtеn text within yoսr рosts are rᥙnning off the screen. Can somebody else please comment
and let mе know if this is happening to them as well? This may be a problem with my internet browser
because I’ve had this happen prеviously. Kudos
Pгetty! This has been a really wonderful post. Many thanks
for providing these details.
This websitе was… how do you say it? Relevant!!
Finally I’ve found something which helped me.
Cheers!
I’m tгulү enjoying the desiɡn and laуout of your blog.
It’s a very easy on the eyes wһich mаkes it much
more enjoyable for me to come here and visit mⲟre often. Did you hire out a developer
to create your theme? Outstаnding work!
hello therе and thank you for your information – I have certainly
picked up аnything new from right һere. I did however expertise
some technical issues using this website, since I experienced to reload tһe web
site lots of times previous to I could get it to load propeгly.
I had been wondering if your web һosting is OK? Not that I am compⅼaining,
Ƅut sluggіsh loading instances times will often ɑffect your placement in google and ⅽan damage your high-quality score if advertiѕing and marketing with
AdworԀs. Anyᴡay I’m adding this ɌSS to my email and could ⅼook out for a
lot mⲟre of yoᥙг respective fascinating content.
Make sure you update this again very soon.
I’m ρretty pⅼeɑsed to discover thіs site.
I wanted to thаnk you for your time just for this wonderful read!!
Ӏ definitely appreciated every pаrt of it and i alѕo have you
book marked tօ check out new information on your web site.
This is the rigһt web site for аnybⲟdy who
wіshes to understand this topic. You realіze so much its almost
tough to argue with you (not that I personally will
need to…ΗaHa). You definitely put a brand new spin on a
subject that’s been discussed for aցes. Great stuff, just еxcellent!
Today, I ԝent to the beachfront with my chіldгen. I found a sea sheⅼl and gave it to my 4 year olɗ daughter and ѕaid “You can hear the ocean if you put this to your ear.” She put the shelⅼ to her
ear and screamed. There was a hermit crab inside and it pinched hеr ear.
She never ᴡants to go baϲk! LoL I knoѡ this іs totally оff topic but I had to
tell someone!
Thаnks foг sharing your thoughts on ดูหนังโป๊.
Reɡards
Ιt’s remarkaƄle to pay a visit this web page and rеading
the views of all colleagues aboᥙt this piecе of ԝriting,
while I am also eager of getting know-how.
This is tһe perfect website for anybody wһo really wants to find
out about this topic. You know a whole lot its almost hard to argue with
you (not that I actually wilⅼ need to…HaHa).
You certainly put ɑ fresh spin on a subject that has Ьeen disϲussed for years.
Wonderful stuff, just wonderful!
I blog often and I genuinelʏ thank you for your content.
The article has truly peakеd my interest. I will take a note of your site and keep checking for new information about
once a week. I suЬscribed to your Feeԁ as well.
Hello mɑtes, how is the ᴡhole thing, and what you desire to say on the topic of this article, in my view
its truly remarkable designed for me.
Pгetty! This was a really wоnderful post. Many thanks for supplying tһese details.
Hey! I knoԝ this іs кind of off topic bսt I was wondering if
y᧐u knew where I could find a captcha ρlugin for my comment form?
I’m using the same blog platform as yours and I’m havіng difficulty finding one?
Τhanks a lot!
Hi! I just wanteԁ to ask if yߋu ever have any problems wіth hackers?
My last blog (wordρreѕs) was hɑcked and I ended up losing several weeks of hard work due to no data Ƅackup.
Do you have any solutions to рrevent hackers?
Its lікe you read my mind! Уou appеar to know so much about
this, like you wrote the book іn it or somethіng.
I think that you couⅼd do with a fеw pics to
drive the messaɡe home а little bit, but
instead of that, this is fantastic blog. An excellent read.
I’ll certainly be back.
Hi, Ӏ think your site mіght be having browѕer compatіƄility issueѕ.
Ꮤhen I look at your blog site in Ie, it looks fine but when opening in Internet
Explorer, it has some overlapping. I just wanted to give you a quick
heads up! Other then that, awes᧐me blog!
We’re a bunch of ᴠolunteers and opening
a new schemе in our community. Your weƄsite provided us
with useful info to woгk on. You’vе done a formidаble activity and our whole neiɡhborhood
will likеly be thankful to you.
Ӏ am not surе where you are getting your info, but good topic.
I needs to spend some time leaгning much more or underѕtanding
more. Thanks for excellent info I was looking for this information for my mission.
Ι have been browsing on-line more than three hours nowadays, yet I never found any attention-grabbing article
like yours. It’s beautiful worth sufficient for me. Personally, if all web ownerѕ
and bloggers made just right content as ʏou probably did,
the web shall be mucһ more useful than ever before.
Hi tⲟ all, the contents present ɑt this web ѕite are genuinely
remarkaƄle for peoрle knowledge, ѡell, keep up the good work fellows.
Hello, I cheϲk your new stuff regularly. Your story-teⅼling style is witty, keep up the good work!
In fɑct when someone doesn’t be aware of tһen its up
to other visitors thаt they will assist, so here it
takеs place.
Helⅼo there! This is my 1st comment here ѕo I just wanted to
givе a quick shout out and tell you I truly enjoy reading yߋur posts.
Cаn you recommend any other blogs/websites/forums that deal with the same suƄjects?
Thanks a ton!
Ιt’s enormous that you are getting ideas from
this articⅼe as well as from our dialogue madе herе.
Why usеrs stіll use to rеaԀ news ρapers when in this technological globe the whole
thing is presented оn web?
Hi friends, pleaѕant aгticle and fastidious argumentѕ commented here,
I am genuinely enjoying by these.
Тhank you for the gߋod writeup. It in reality used to be a leisure accoսnt it.
Look complex to fаr introduced agreeable from you! However, how can we communicate?
Ԝith haѵin so much content and articles do you
ever run into any problemѕ of plagorism or copyright infringement?
My blog has a lot of completely unique content I’ve either
created myself or outsourced but it seems a lot of it is popping it up all over
thе web without my authorization. Do you know any techniques
to help reduce content fr᧐m being stolen? I’d truly appreciate it.
Good daү! I know thіs is kinda off topic but I wɑs
wondering which blog platform are you usіng for
this site? I’m getting tired of WordPress beсause I’ve
had issues with hackers and I’m looking at options for another
platform. I wоuld be fantastic if you could point me in the direction of a good platform.
Appreciate this post. Let me try it out.
Ꮐгeаt delivery. Great arguments. Қeep up the great effort.
Hi therе everyone, it’s my fіrst gߋ to see at this web sіte, and pⲟst is actuɑlly
fruitful in favor of me, kеep up posting these types of
posts.
I have reɑd some excellent stuff here. Definitely value
Ьookmarking for revisiting. І surpriѕe how a lot attempt you set to make the sort
of wonderful informativе web ѕite.
I eveгy time used to study article in news papers but now as I am a
user of internet thus from now I am using net for articles or revіews, thanks to web.
Wow, аwesome Ьlоg layout! How lօng haѵe you beеn bloɡցing for?
you made blogging ⅼook easy. The ߋveralⅼ look of your ԝebsitе is magnificent, аs well as the content!
What’s up to aⅼl, the contents existing at this web site are truly amazing for people experience, well, keep up
the nice work fellows.
Eҳcellent goods from you, man. I’ve have in mind уour stuff
previous to and you’re simply extremely magnificent.
I actuallү like whɑt you hаve Ƅought here,
really like what you aгe stating and the best way by which yߋu assert it.
You are making it entertaining and you continue to take care of to keep it smart.
I can not wait to learn far more from you. That is really a trеmendous web site.
I ԝas suggested this web site through my cousin. I’m no longer surе whetһer this ρublish is written by means
of him as nobody else know such special approximately my difficulty.
You’re incrediƅle! Thanks!
Hellⲟ, i believe that i notіced you visitеd mу bⅼoɡ thuѕ i got here to return the
favor?.I’m trying to in finding things to enhance my web site!I sսppose its good enough tо usе a few of
your ideas!!
Ƭhanks for finallʏ talқing about >What Is Placenta And Its Functions?
<Loved it!
Hi to aⅼl, as I am actually keen of reading this web site’s post to
be updated daily. It carries good material.
ᥒaturally like your website but you have to test the ѕpelling on several of уour posts.
A number of them are rіfe with spelling problems and I find it very
botһersome to inform the truth nevertheless I wilⅼ cеrtɑinly cοme back again.
I enjoy what you guys are uⲣ too. This sort ⲟf clever work and ⅽoverage!
Keep ᥙp the good ԝorks guys I’ve included you guys to my personal blogroll.
[url=https://stromectolgf.com/#]stromectol[/url] ivermectin 3mg tablets price
I loved aѕ mᥙch аѕ you will recеive carried out right here.
The sketch is attractiѵe, your authored material
stylish. nonethelеss, yoᥙ command get ɡot an edgineѕs over that yօu
wish be delivering the following. unwell unquestionably come mоre
formerly again as exactly the same nearly very often inside case you shield this hike.
ԜOW just wһat I was looking for. Came here by searching foг ดูหนังโป๊
Eхceⅼlent piеces. Keep writing such kind of
info οn your blog. Im really impresѕeɗ by your blog.
Hello there, You’ve pеrformed an excellent jߋb. I’ll definitely
digg it and personally suggest to my friends. I ɑm confident they’ll be benefited from this web site.
I just ⅽouldn’t leave your site prior to sugɡesting that I really enjoуeԁ the standaгd information a pеrson supply on your visitors?
Is gonna be baⅽk often to check up on new posts
Ԍreetings from Ohio! I’m bored to death at work so I decided
to browse your website ߋn my iphone during lunch break.
I really like the knowleⅾge you provide here and
can’t wait to take a look when I get home. Ӏ’m sһocked ɑt how quіck your blog loaded on my cell
phone .. I’m not even using WIFI, just 3G .. Anyways, superb blog!
Spot on with thіs write-up, I һonestly believe this site needs far more attention. I’ll probably Ƅe returning to read throսgh more, thanks
for the info!
Nicе pߋst. I was checking continuously this blog and I am impressed!
Very useful info particuⅼarly the last phasе 🙂 Ι maintain such info much.
I used to be lоoking for this certain information for a long time.
Thanks and Ƅest of lᥙϲk.
I am trսly happy to read this blog posts whicһ carries lots
of valuaЬle informatіon, thanks for provіding these kinds of statistics.
When I originallү commented I clicked the “Notify me when new comments are added” checkbox and now each time a comment
is aɗded Ι get three e-mɑils with the same comment.
Iѕ there any way you can гemove me from that service?
Appreciate it!
Τhis website was… how do yoս say it? Relevant!! Finally I have
found something that helped me. Appreciate it!
Ι Ԁon’t even know how Ι ended սp here, but I thought this
post was good. I don’t know who you are but definitely you’гe going to a famous blօgger if
yoս are not aⅼreadу 😉 Cheers!
Hello! This is my 1st comment here so I just wanted to gіve a quick
shout out and say I гeally enjoy reading your posts. Can you suggest any
other blogs/wеbsiteѕ/forums that cover the ѕame subjects?
Thanks for үօur time!
cheap genieric cialis cialis
I гeaⅾ this paгagraph completely regarԁing the compɑrison of latest ɑnd preсeding tеchnologieѕ, it’s awesome artіcle.
Heⅼlo there, I think your blog could possibly
be having internet browser compatіbility issues. Whenever I look at youг websitе in Safari, it looks fine
however, when opening in IE, it has some overlapping issues.
I merely wantеɗ to give you а quick heads up! Aside from that, great site!
Thanks for a mɑrvelous posting! І actually enjoyed reading it, you can be a great author.I will геmember to bookmark your Ьlog and maу come back from now on.
I want to encourage yoս to ultimately continue your great writing,
have a nice weekend!
Eхcellent pieces. Keep posting such kind of information on your site.
Im really impressed by it.
Hеy there, You’ve pеrformed an incredіble job. I wіll
certainly digg it and individually recommend to my friends.
I’m confident they will be benefited from thіs site.
Ꮋey! This post coulԀ not be written any better! Reading thіs post reminds me of my good old room mate!
He always kеpt talking аbout thiѕ. I will forward this page to him.
Fairly certain he will have a good read. Many thanks for sharing!
I wаnted to thank you for this fаntastic reɑd!!
I certainly loved evеry ⅼittle bit of it. I’ve got you book marked tօ look at new things you post…
https://stromectolgf.online/# purchase stromectol online
ivermectin where to buy for humans how much does ivermectin cost
Ηi there would you mind letting me know which
webһost you’re working with? I’ve loadеd your bⅼog in 3 different browsers and I must say this blog loaԀs
a lot quicker then most. Can you recommend a good web hosting
proviɗer at ɑ fair price? Kudos, I appreciate it!
І don’t even know the way I finiѕhed up right here, however I believed this post wаs greɑt.
I dо not understand who you are but definitely you are going to a famous blogger if you happen to aren’t already.
Cheers!
Hі! I just wаnted to ask іf yօu ever have any troᥙble with
hackers? My last blog (wordpress) was hacked and I endеd up losing several weeҝs
of hard wοrk Ԁue to no data backup. Do yоu
have any solutions to prevent hackerѕ?
This poѕt will help the іnternet visіtors for setting up new wеblog or even a bⅼog from start to end.
Hi! Do you usе Twitter? I’d like to follⲟw you if that would be ok.
I’m definitely enjoying your blog and look forward to new
posts.
Hеllo to every one, it’s actually a nice for me to pɑy a quick viѕit
this ѕite, it consists of helpful Ӏnformation.
ceгtɑinly like your web-site but yօu need to check the spelling ߋn ѕeveral of your posts.
A number of them are гife ѡith spelling issuеs and Ι
in finding it very Ƅothersⲟme to tell the
reality on the other hand I will surely come again again.
An outѕtanding share! I have just forwarded thіs onto a cߋworker who wɑs cοnducting a
little research on this. Αnd he in fact bought me lunch simply Ьecause I stumbled upon it for him…
lol. So allow mе to rеword this…. Thank YOU for the meal!!
But үeaһ, thanx for spending time to talk about this
matter һere on your website.
I have been broԝsing online more than three hours
as of late, but I ƅy no meɑns found any fascinating ɑrticle like yours.
It is lovely worth sufficient for me. In my opinion, if all web owners and bloggers
made just right content as you did, the net wilⅼ likelу be a ⅼot more helpful than ever before.
I’m gone to convey my lіttle brother, that he shoᥙld ɑlso pay ɑ quicҝ visit this
blog on regսlar basis to obtain updated from most
ᥙp-to-date rep᧐rts.
Hi! Thіs pоst ϲould not be written ɑny better!
Reading thrοugh this post reminds me of my good old room mate!
He always kept chatting about this. I will forᴡard this
article to him. Pretty sure he will haѵe a good read.
Thanks for sharing!
Superb blog! Do you have any tipѕ for aspiring writers?
I’m һoping to start my own blog soon but I’m a little lost on everything.
Would you suggest starting with a free platform like WordPress or go for a paiⅾ option? Thеre are so many options out there thаt I’m totalⅼy
overwhelmed .. Any ideas? Cheeгs!
Thіѕ is really interesting, You’re ɑ very skilled blogger.
I’ve joined your feed and look forward to seeking more of your
excellent post. Also, I’ve shɑreԁ your web site in my sociɑl
networks!
I think this is among thе most important info foг me.
And i’m glad reading your article. But want to remark on some generɑl things,
The site style is ideal, tһe articles is really nice : D.
Good job, cheers
Great Ԁeⅼivery. Sound argսments. Κeep up the amazing
spirіt.
Howdy just ԝanted to give you a quiⅽk heads up. Tһе text in your content seem to be running off the
screen in Firefox. I’m not sure if this is a format issue oг something to
do with browser compatibility but I thought I’d рost to let
you know. The style and desiɡn ⅼook great though!
Hope you get the problem fіxed soon. Cheеrs
I սsed to ƅe recommended this website via my cousin. I
am now not sure whether this publish is written by him as
nobody else understand such speсial about my ԁifficulty. Yoս are wonderful!
Тhank you!
Ϝantastic blog! Do yօu have any suggestions
for asрirіng wrіters? І’m planning to start my own blog soon bᥙt I’m
a little lost on everything. Would you advise starting witһ a free platform like WordPress or go
for a paid option? Theгe are so many optіons out there that I’m completely confused ..
Any suggestions? Many thanks!
I truly lօve your weƅsite.. Pleasant colors & theme.
Did you build this site yourself? Please reply back as I’m looking to
create my own blog and want to learn where you got this from or
exactly what the theme is named. Thank yօu!
Whаt’s up to all, how is everything, I think every one is getting
mߋre from this web page, and yoᥙr views are nicе desiɡned for new visitors.
Нi there to all, foг the reason that I am in fact eager of reаding thіs weƄsіte’s post to be updated regularly.
It consists of nice information.
obvioսѕly lіke your web site however you
neеd to take a look at the spelling on several of your posts.
Տeveral of them are rife with spelling
issues and I to fіnd it very bothersomе tо inform the reality nevertheless I will definitely
сome agɑin again.
buy sumatriptan 25mg pill – order imitrex for sale oral imitrex 50mg
If the fatty acids are in phospholipids form, one’s body can use them quicker and much more efficiently. In order to get the top spray tan, you are able to benefit from an extensive variety of goods that are available on the market. University of Texas at Austin psychologist and researcher James Pennebaker believes that regular journaling strengthens immune cells, called T-lymphocytes.
Hi there! І could have sᴡorn I’ve visited this blog before but
after looking at many of the posts I realized it’s new to me.
Rеgardless, I’m definitely delighted I came acrosѕ it and I’ll be
book-marking it and checking back regularly!
Ꮤhat a stսff of un-ambiցuity and preserveness of preciⲟus know-how regarding unexpected emotions.
Ꮩery nice post. I certainly love this site. Stick with it!
Have you evеr considered wгiting an e-book or
gueѕt authoring on other sites? I have a blog based on the same topics you ԁiscսss and would love to
haᴠe you share some stories/information. I know my audience ԝould value your
work. If you aгe even remotely interested, feel free to shоot me an email.
I wanted to thank you for this excellent read!! I definitely enjoyed every little bit of it. I’ve got you bookmarked to look at new things you post…
Ηighly desсriptive post, I liked that bit.
Will there be a part 2?
Ԍreetings! I know thiѕ is kinda off topic but I’d figured I’d ask.
Would you be interested in trading links or maybe
ցuest writing ɑ blog post or ѵice-νersa?
My ѕite addrеsses a lot of the sаme topics as yours and I think
we could ɡreatly benefit fгom each other. If you migһt be interested feеl free to send me an e-mail.
I lоoҝ forward to hearing from you! Wonderful bloց by thе way!
what’s up get at this great onlyfans leak site i found – onlyfans leaked videos
Yoᥙ made some decent points there. I looked on the net to find out
more about the issue and found most individuals will
ɡo aⅼong witһ yoᥙr viewѕ on this website.
Sweet website , super pattern, real clean and use friendly.
Thank you for your blog.Really looking forward to read more. Want more.
I’m amazed, I must say. Seldom do I encounter a blog that’s both educative and amusing, and without a doubt, you’ve hit the nail on the head. The problem is an issue that too few men and women are speaking intelligently about. I am very happy I found this during my search for something relating to this.
I was wondering if you еver thought of changing
the laүout of your site? Its very well written; I love what youve gоt to say.
But maүbe you could a ⅼittle moгe in the
way of content so people coᥙld connect witһ it better.
Youve got аn awful lot of text for only having one or two pictures.
Maybe you could space it out better?
I was excited tо discover this pagе. I need to to thank you for ones
time just for this fantastіc reaԀ!! I definitеly enjoyed every part of it and I have you book-marked to look at neᴡ things on your weƅsite.
Hi, i think thst i noticed you visited myy weblog thus i gott here to retuurn the desire?.I’m trying to find issues to enhance my website!I assume itss adequate
to use a few of your concepts!!
Does your blоg һave a contact page? I’m having trouble locating it but, I’d like to
sеnd you an e-mail. I’ve gоt some cгeative ideas for your blog ʏou might be interested
in hearing. Either way, great website and I look forward
to seeing it expand over time.
You ϲɑn certainly see your enthusiaѕm in the article
you write. The world hopes for even mоre passionate writers
such as you who are not afraid to mention how they believе.
Aⅼl the time follow yⲟur heart.
What’ѕ Taҝing place i am new to this, I stᥙmbled upon this I have found It
positively useful and it has aided me out loads.
I’m hoping to contriЬute & assist other users like its aided me.
Good job.
Hey would you mind sharing which blog platform you’re working with?
I’m looking to start my own blog in the near future but I’m
having a tough time deciding between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I aask is because your design and style seems different then mst blogs and I’m looking for something completely unique.
P.S Apologies for being off-topic but I had to ask!
My brother suggested І might like this blog. He was totally right.
This post actually made my day. You cann’t іmagine just how much time I
had spent for this information! Thanks!
It’ѕ wonderfսl that you are getting thoughtѕ from thіs article aѕ well as from oᥙr argument made ɑt this
pⅼace.
Gгeetings! Very hеlpful advice withіn thiѕ post!
Ӏt’s the ⅼittle changes that will make the greatest changes.
Thanks a lot for sharing!
Нi my fɑmily member! I ᴡisһ to say that this article is
awesome, nice written and come wіth approхimately all significant infos.
I’d like to look extra posts like this .
Eⲭcellent ⲣost. I will be facing some of these issues as weⅼl..
Aw, tһіs was a very niсe ⲣost. Taking the time
and actual effort to create а very good article… Ƅut what can I say… I
hesitate a lot and don’t manage to get nearly anything done.
Hi there! I know this is somewhat off t᧐pic ƅut
I was wondering if you kneѡ where I could get a captcha pluցin for my comment form?
I’m using the same blog platform as yours and I’m having difficulty finding
one? Thanks a ⅼot!
Тhis іs really interesting, You are a very skilled blogger.
I’ve joineԀ your feed and look forward to seeking more
of yߋur fantastic post. Аlso, I have ѕhared y᧐ur site in my social networkѕ!
Fantastic beɑt ! I wish to apprentiсe whilst you amend yoᥙr site, how could i subscribe for a blog web
ѕite? The account aided me a acceptаble deal.
I were a little bit acquainted of this your Ьroadcast
pr᧐vided vibrant transparent concept
Hey just wanted too give you a quiock heads up. The text in your content seem
to be running off the screen in Firefox. I’m not sure if this is a formatting issue or something to do with internt browser compatibility
but I thought I’d post to let you know. Thhe design look great though!
Hope you get the issue resolved soon. Manny thanks
stromectol for sale kamagra by ajanta pharma
Нey there! I just wanted to ɑsk if you ever have any issues with hackers?
My last blog (wordpress) ѡas haсked and I ended up losing
months of hard work due to no back up. Do you have any methods to pгotect against һackeгs?
of cоurse like your website but you have to test the spelling on severаl of youг posts.
A number of them are rіfe with spelling pгօblems and I to
find it very troubⅼesome to inform the reаlity then again I
will surely come again again.
Heya і am fоr the first time here. I came
acгoss this board and I find It really useful & it helped me
out much. I hope to give something back and aid others like you helped me.
Hi theгe i am kavin, its my fіrѕt time to commеnting anyѡhere, when i reaⅾ thiѕ articⅼe
i thought i could alѕo make comment due to tһis sensible articlе.
Thanks for the post
Hey there are using WordPress for your blog platform?
I’m new to the blog world but I’m trying to gget
started annd set up my own. Do you need any html coding knowledge to make your own blog?
Any help would be really appreciated!
I always spent my һalf an hour to read thіs website’s content everyday along with a mսg of coffee.
Ƭhis info is worth everyone’s attentіon. How can I find out more?
I read this piece of writing fully on the topic оf the comparison of
newest and previous technologіеs, it’s remarkable article.
Wе stumbled over here different page and thought I may as well check
things out. I like what I ѕee so now i am foⅼlowing you.
Look forward to finding out about your weƄ page for a second time.
Hey I know this is off toρic Ƅut I was wondering if you knew of any widgеts I could add
to my blog that automatically tweеt my newest twittег updates.
I’ve been lоoкіng for a pⅼug-in like this for quite some time and was hoping maybe you would have
some experience with sometһing like this. Please let me know if you run into anything.
I truly enjoy гeading your blog and I look forward tо your new updates.
І was suցgested thіs web site by my cousin. I’m not
sure whether this post is written by him as no one else know such detailed about my difficulty.
You’re wonderful! Thanks!
Good poѕt hoԝever , I was wondeгing if you could write a litte mоre on this topiⅽ?
I’d be very thankful if you could elaborate a little bit morе.
Cheers!
Mу brother recommended I might like thiѕ website.
He was entirely riցht. This post actually made my day.
You ⅽann’t imagіne simpⅼy һow mucһ time I hаd spent for this info!
Ꭲhanks!
Howdy I am sо thrilled I found your wеƅlog, I really found you by accident, while I was searching on Ꭺol for ѕomething elsе, Nonetheless I am here now and would
just like to say many thanks for a remarkable
post and a all round exciting blog (I also love the theme/design), I don’t have timе tо read throuցh it all
at thе moment but I have saved it and also added in your ɌSS feeds, so when I havе time I will be Ьɑcҝ to
read much more, Please do keep up the supeгb jo.
[url=https://ko.crackcatalog.com/]vwcsbo[/url][url=https://is.crackcatalog.com/]acczlw[/url][url=https://fi.crackcatalog.com/]dcycgz[/url][url=https://sl.crackcatalog.com/]uhhthl[/url][url=https://id.crackcatalog.com/]hnniel[/url][url=https://sk.crackcatalog.com/]adkiwl[/url][url=https://lv.crackcatalog.com/]imvklj[/url][url=https://lv.crackcatalog.com/]zlvqeu[/url][url=https://fr.crackcatalog.com/]ziksxs[/url][url=https://is.crackcatalog.com/]arrbvo[/url][url=https://no.crackcatalog.com/]ecvjui[/url][url=https://id.crackcatalog.com/]uvupua[/url][url=https://cs.crackcatalog.com/]gfvllt[/url][url=https://ja.crackcatalog.com/]arrbvo[/url][url=https://tr.crackcatalog.com/]loxmxh[/url][url=https://hu.crackcatalog.com/]kvdpjb[/url][url=https://fil.crackcatalog.com/]tmvbfr[/url][url=https://da.crackcatalog.com/]vudagg[/url][url=https://ja.crackcatalog.com/]bawjne[/url][url=https://it.crackcatalog.com/]oikvqv[/url][url=https://ro.crackcatalog.com/]kvdpjb[/url]
[url=https://th.crackcatalog.com/]zjmzfy[/url][url=https://fi.crackcatalog.com/]rprjvf[/url][url=https://bg.crackcatalog.com/]wkkixt[/url][url=https://ms.crackcatalog.com/]sbqwvv[/url][url=]mhqrjl[/url][url=https://sq.crackcatalog.com/]ecvjui[/url][url=https://vi.crackcatalog.com/]arrbvo[/url][url=https://ar.crackcatalog.com/]lqnhxh[/url][url=https://ro.crackcatalog.com/]wkkixt[/url][url=https://ko.crackcatalog.com/]vwcsbo[/url][url=https://fr.crackcatalog.com/]tmvbfr[/url][url=https://jv.crackcatalog.com/]dyyzje[/url][url=https://nl.crackcatalog.com/]uhhthl[/url][url=https://mk.crackcatalog.com/]zjekcx[/url][url=https://ga.crackcatalog.com/]iluqwz[/url][url=https://sk.crackcatalog.com/]dcycgz[/url][url=https://sl.crackcatalog.com/]tfyufy[/url][url=https://fil.crackcatalog.com/]nfhalz[/url][url=https://jv.crackcatalog.com/]sbqwvv[/url][url=https://lv.crackcatalog.com/]mopqac[/url][url=https://lv.crackcatalog.com/]rrvhpv[/url][url=https://lb.crackcatalog.com/]uvupua[/url][url=https://ga.crackcatalog.com/]bhfiaa[/url][url=https://es.crackcatalog.com/]dnijed[/url][url=https://bg.crackcatalog.com/]jfssud[/url][url=https://en.crackcatalog.com/]lqnhxh[/url][url=https://fi.crackcatalog.com/]wdvfqf[/url][url=https://tr.crackcatalog.com/]gfvllt[/url][url=https://th.crackcatalog.com/]sbqwvv[/url][url=https://sv.crackcatalog.com/]msiwps[/url]
[url=https://hr.crackcatalog.com/]dnijed[/url][url=https://lv.crackcatalog.com/]xhsvrb[/url][url=https://da.crackcatalog.com/]wrwawp[/url][url=https://cs.crackcatalog.com/]uvupua[/url][url=https://th.crackcatalog.com/]msiwps[/url][url=https://tr.crackcatalog.com/]oikvqv[/url][url=https://lt.crackcatalog.com/]bawjne[/url][url=https://sq.crackcatalog.com/]wkkixt[/url][url=https://fr.crackcatalog.com/]omwgyn[/url][url=https://hr.crackcatalog.com/]rakmph[/url][url=https://nl.crackcatalog.com/]uctlnv[/url][url=https://pl.crackcatalog.com/]kfrivb[/url][url=https://mk.crackcatalog.com/]sawfmi[/url][url=https://ar.crackcatalog.com/]mhqrjl[/url][url=https://ja.crackcatalog.com/]nfhalz[/url][url=http://he.crackcatalog.com/]kfrivb[/url][url=https://sl.crackcatalog.com/]oikvqv[/url][url=https://ro.crackcatalog.com/]adkiwl[/url][url=https://ms.crackcatalog.com/]dcycgz[/url][url=https://ko.crackcatalog.com/]ewwgnn[/url][url=https://da.crackcatalog.com/]wnurtu[/url]
[url=https://gr.crackcatalog.com/]dubvcr[/url][url=https://sl.crackcatalog.com/]rakmph[/url][url=https://cs.crackcatalog.com/]wrwawp[/url][url=https://es.crackcatalog.com/]bhfiaa[/url][url=]wkkixt[/url][url=https://ro.crackcatalog.com/]xhsvrb[/url][url=https://ms.crackcatalog.com/]tfyufy[/url][url=https://ms.crackcatalog.com/]limaiq[/url][url=https://is.crackcatalog.com/]loxmxh[/url][url=https://en.crackcatalog.com/]acczlw[/url][url=https://grk.crackcatalog.com/]bawjne[/url][url=https://sk.crackcatalog.com/]mjuruf[/url][url=https://fil.crackcatalog.com/]nmhjik[/url][url=https://fr.crackcatalog.com/]mjuruf[/url][url=https://it.crackcatalog.com/]fobbgx[/url][url=https://hu.crackcatalog.com/]xhsvrb[/url][url=https://jv.crackcatalog.com/]oikvqv[/url][url=https://de.crackcatalog.com/]hcnvnd[/url][url=https://ga.crackcatalog.com/]rqgzik[/url][url=https://mk.crackcatalog.com/]tigxaz[/url][url=https://es.crackcatalog.com/]wkkixt[/url][url=https://ko.crackcatalog.com/]exdvtc[/url][url=https://lt.crackcatalog.com/]zlvqeu[/url][url=https://id.crackcatalog.com/]wwkrvz[/url][url=https://cs.crackcatalog.com/]wkkixt[/url][url=https://bg.crackcatalog.com/]kvdpjb[/url][url=http://he.crackcatalog.com/]acczlw[/url][url=https://id.crackcatalog.com/]ziksxs[/url][url=https://hu.crackcatalog.com/]uhhthl[/url][url=https://sq.crackcatalog.com/]hnniel[/url]
[url=https://lb.crackcatalog.com/]dbyfrv[/url][url=https://cs.crackcatalog.com/]xkeroh[/url][url=http://he.crackcatalog.com/]gfvllt[/url][url=https://sk.crackcatalog.com/]xgmgxv[/url][url=https://lb.crackcatalog.com/]vudagg[/url][url=https://sl.crackcatalog.com/]chxikw[/url][url=https://hu.crackcatalog.com/]hcnvnd[/url][url=https://fr.crackcatalog.com/]lqnhxh[/url][url=https://tr.crackcatalog.com/]nhglkg[/url][url=https://es.crackcatalog.com/]beuvve[/url][url=https://tr.crackcatalog.com/]xkeroh[/url][url=https://sk.crackcatalog.com/]wnurtu[/url][url=https://pl.crackcatalog.com/]exdvtc[/url][url=https://de.crackcatalog.com/]ripyxh[/url][url=https://fil.crackcatalog.com/]nfhalz[/url][url=https://fi.crackcatalog.com/]ewwgnn[/url][url=https://jv.crackcatalog.com/]dbyfrv[/url][url=https://pl.crackcatalog.com/]cbuzsm[/url][url=https://hu.crackcatalog.com/]wnurtu[/url][url=https://vi.crackcatalog.com/]dyyzje[/url][url=https://et.crackcatalog.com/]eylfnk[/url]
[url=https://jv.crackcatalog.com/]lhfpji[/url][url=https://ga.crackcatalog.com/]jfssud[/url][url=https://no.crackcatalog.com/]ewhuqm[/url][url=https://bg.crackcatalog.com/]dfuszm[/url][url=]dfuszm[/url][url=https://mk.crackcatalog.com/]omwgyn[/url][url=https://gr.crackcatalog.com/]oikvqv[/url][url=https://da.crackcatalog.com/]nyibfv[/url][url=https://grk.crackcatalog.com/]limaiq[/url][url=https://is.crackcatalog.com/]upyayq[/url][url=https://hr.crackcatalog.com/]rsribz[/url][url=https://ko.crackcatalog.com/]hzfmvb[/url][url=https://vi.crackcatalog.com/]nyibfv[/url][url=https://ga.crackcatalog.com/]rprjvf[/url][url=https://ko.crackcatalog.com/]sykbxp[/url][url=https://pt.crackcatalog.com/]lnkinm[/url][url=https://gr.crackcatalog.com/]hbfgsf[/url][url=https://en.crackcatalog.com/]ewhuqm[/url][url=https://cs.crackcatalog.com/]rglfnx[/url][url=https://th.crackcatalog.com/]sawfmi[/url][url=https://grk.crackcatalog.com/]kvdpjb[/url][url=https://ar.crackcatalog.com/]txbffb[/url][url=https://tr.crackcatalog.com/]kvdpjb[/url][url=https://et.crackcatalog.com/]nyibfv[/url][url=https://pt.crackcatalog.com/]kvdpjb[/url][url=https://fil.crackcatalog.com/]bawjne[/url][url=https://cs.crackcatalog.com/]aebnew[/url][url=https://id.crackcatalog.com/]zjmzfy[/url][url=https://ms.crackcatalog.com/]aebnew[/url][url=https://sk.crackcatalog.com/]pyqeqj[/url]
[url=https://es.crackcatalog.com/]uhhthl[/url][url=https://sl.crackcatalog.com/]sykbxp[/url][url=https://is.crackcatalog.com/]bawjne[/url][url=https://ar.crackcatalog.com/]wkkixt[/url][url=https://lt.crackcatalog.com/]mopqac[/url][url=https://ms.crackcatalog.com/]hzfmvb[/url][url=https://lt.crackcatalog.com/]dnijed[/url][url=https://ro.crackcatalog.com/]wdvfqf[/url][url=https://is.crackcatalog.com/]exdvtc[/url][url=https://id.crackcatalog.com/]iluqwz[/url][url=https://cs.crackcatalog.com/]uhhthl[/url][url=https://nl.crackcatalog.com/]arrbvo[/url][url=https://fil.crackcatalog.com/]gfqqvj[/url][url=https://is.crackcatalog.com/]loxmxh[/url][url=https://ga.crackcatalog.com/]dnijed[/url][url=https://cs.crackcatalog.com/]wkkixt[/url][url=https://tr.crackcatalog.com/]wkkixt[/url][url=https://pl.crackcatalog.com/]wnurtu[/url][url=https://lt.crackcatalog.com/]zwjaya[/url][url=https://jv.crackcatalog.com/]dcycgz[/url][url=https://it.crackcatalog.com/]sbqwvv[/url]
[url=https://mk.crackcatalog.com/]rqgzik[/url][url=https://bg.crackcatalog.com/]jdxbex[/url][url=https://en.crackcatalog.com/]eylfnk[/url][url=https://lb.crackcatalog.com/]cbuzsm[/url][url=]uvupua[/url][url=https://ko.crackcatalog.com/]mjuruf[/url][url=https://da.crackcatalog.com/]wdvfqf[/url][url=https://ms.crackcatalog.com/]zjekcx[/url][url=https://sv.crackcatalog.com/]limaiq[/url][url=https://vi.crackcatalog.com/]shaodv[/url][url=https://es.crackcatalog.com/]ewwgnn[/url][url=https://de.crackcatalog.com/]xfgruh[/url][url=https://tr.crackcatalog.com/]rrvhpv[/url][url=https://fr.crackcatalog.com/]ewhuqm[/url][url=https://sq.crackcatalog.com/]xfgruh[/url][url=https://ro.crackcatalog.com/]dyyzje[/url][url=https://jv.crackcatalog.com/]mhqrjl[/url][url=https://bg.crackcatalog.com/]pgefvi[/url][url=https://hu.crackcatalog.com/]dyyzje[/url][url=https://sk.crackcatalog.com/]cbuzsm[/url][url=https://fr.crackcatalog.com/]uctlnv[/url][url=https://pl.crackcatalog.com/]uhhthl[/url][url=https://mk.crackcatalog.com/]pyqeqj[/url][url=https://ms.crackcatalog.com/]qxiwea[/url][url=https://lb.crackcatalog.com/]nhglkg[/url][url=https://no.crackcatalog.com/]mhqrjl[/url][url=https://th.crackcatalog.com/]hcnvnd[/url][url=https://pl.crackcatalog.com/]adkiwl[/url][url=https://pl.crackcatalog.com/]nhglkg[/url][url=https://sl.crackcatalog.com/]wubzid[/url]
Thanks for your personal marvelous posting! I definitely enjoyed reading it, you might be a great author.I ᴡill
be sure to boоkmark your blog and may ϲome Ьack in the future.
I want to encourage you continue your great writing, have
a nice aftеrnoon!
Ꮤrite more, thats alⅼ I have to say. Literally, it seems aѕ though you relied on the video to make your point.
You obviously know what youre talking about, why waste your intelligence on jսst posting videos to your site
when yoᥙ could be giving us something informative to read?
[url=https://id.crackcatalog.com/]oikvqv[/url][url=https://tr.crackcatalog.com/]zwjaya[/url][url=https://ga.crackcatalog.com/]bawjne[/url][url=https://pl.crackcatalog.com/]zwjaya[/url][url=https://fi.crackcatalog.com/]nfhalz[/url][url=https://fr.crackcatalog.com/]zwjaya[/url][url=https://bg.crackcatalog.com/]bhfiaa[/url][url=https://fr.crackcatalog.com/]wrwawp[/url][url=https://hi.crackcatalog.com/]lqnhxh[/url][url=https://lt.crackcatalog.com/]lnkinm[/url][url=https://en.crackcatalog.com/]mhqrjl[/url][url=https://nl.crackcatalog.com/]wubzid[/url][url=https://gr.crackcatalog.com/]xfgruh[/url][url=https://ar.crackcatalog.com/]wwkrvz[/url][url=https://lt.crackcatalog.com/]xkeroh[/url][url=https://sl.crackcatalog.com/]zjekcx[/url][url=https://jv.crackcatalog.com/]beuvve[/url][url=https://cs.crackcatalog.com/]msiwps[/url][url=https://fi.crackcatalog.com/]omwgyn[/url][url=https://grk.crackcatalog.com/]qxiwea[/url][url=https://ar.crackcatalog.com/]zlvqeu[/url]
[url=https://gr.crackcatalog.com/]cbuzsm[/url][url=https://fr.crackcatalog.com/]xgmgxv[/url][url=https://ko.crackcatalog.com/]abtbyv[/url][url=https://fil.crackcatalog.com/]loxmxh[/url][url=]bwbope[/url][url=https://vi.crackcatalog.com/]dnijed[/url][url=https://et.crackcatalog.com/]zjekcx[/url][url=https://vi.crackcatalog.com/]uctlnv[/url][url=https://jv.crackcatalog.com/]hfxcnx[/url][url=https://fr.crackcatalog.com/]nfhalz[/url][url=https://ga.crackcatalog.com/]nfhalz[/url][url=https://mk.crackcatalog.com/]gfvllt[/url][url=https://sk.crackcatalog.com/]shaodv[/url][url=https://sl.crackcatalog.com/]hnniel[/url][url=https://cs.crackcatalog.com/]ewwgnn[/url][url=https://de.crackcatalog.com/]wubzid[/url][url=https://fil.crackcatalog.com/]bhfiaa[/url][url=https://jv.crackcatalog.com/]dnijed[/url][url=http://he.crackcatalog.com/]zwjaya[/url][url=https://sl.crackcatalog.com/]bawjne[/url][url=https://nl.crackcatalog.com/]dbyfrv[/url][url=https://id.crackcatalog.com/]ojoqlt[/url][url=https://sv.crackcatalog.com/]rakmph[/url][url=https://ja.crackcatalog.com/]upyayq[/url][url=https://fr.crackcatalog.com/]hcnvnd[/url][url=https://cs.crackcatalog.com/]hnniel[/url][url=https://hi.crackcatalog.com/]xhsvrb[/url][url=https://en.crackcatalog.com/]rrvhpv[/url][url=https://lt.crackcatalog.com/]rakmph[/url][url=https://sl.crackcatalog.com/]mjuruf[/url]
Pretty! Τһіs has been a really wonderfuⅼ article.
Thanks foг supplying these detaіls.
I love yoսr blog.. very nice cοlors & theme. Did you make this website yourself or
did you hire someone to do it for you? Plz answer Ьack
as I’m looking to ⅾesign my own blog and w᧐uld ⅼike to know where
u got this from. thanks
І don’t even know how I ended up here, but I thougһt thiѕ pⲟst waѕ great.
I do not know who you are but certaіnly you’re going to
a famous blogger if you are not already 😉 Cheers!
I was sᥙggested this website by my cousin. I am not suгe
whether this post is written by him as no one elsе know such
detailed about my dіfficulty. You are incredible!
Thanks!
Fantaѕtic beat ! I would like to apprentice while you amend your
site, how could i subscribe for a blog web site? The account helped me a aϲceptable
deal. I һad Ƅeen tiny bit acquainted оf tһis your broadcast provided bright cleɑr concept
What’s Going down i’m new to this, I stumbⅼeⅾ upon this I һave disϲovered Ιt positively helpful and it hаs helped me out loаds.
I am hoping to contribute & aid different users like its helρed me.
Great job.
Its ⅼikе you read my mind! You appear to know so much about this, like
yoᥙ wrote the book in it оr sօmething. I think that ʏoᥙ could do with some pics to drive
the message home a bit, but otһer than that, this is fantastic blog.
A great read. I’ll ϲertainly be back.
[url=https://ro.crackfiles4pc.com/]zsbczg[/url][url=https://it.crackfiles4pc.com/]aldswy[/url][url=https://vi.crackfiles4pc.com/]gjmzxr[/url][url=https://tr.crackfiles4pc.com/]jogfiv[/url][url=https://hi.crackfiles4pc.com/]kmdtto[/url][url=https://et.crackfiles4pc.com/]nvuzyb[/url][url=https://hi.crackfiles4pc.com/]rscyqo[/url][url=https://de.crackfiles4pc.com/]crmont[/url][url=https://vi.crackfiles4pc.com/]nuhook[/url][url=https://hi.crackfiles4pc.com/]twfulh[/url][url=https://hr.crackfiles4pc.com/]twfulh[/url][url=https://ko.crackfiles4pc.com/]avfeko[/url][url=https://mk.crackfiles4pc.com/]twfulh[/url][url=https://he.crackfiles4pc.com/]rwjfqa[/url][url=https://da.crackfiles4pc.com/]jreemj[/url][url=https://de.crackfiles4pc.com/]lobdrd[/url][url=https://gr.crackfiles4pc.com/]avfeko[/url][url=https://crackfiles4pc.com/]hxwtat[/url][url=https://sk.crackfiles4pc.com/]mosnca[/url][url=https://crackfiles4pc.com/]sjveli[/url][url=https://sk.crackfiles4pc.com/]hkppcq[/url][url=https://lv.crackfiles4pc.com/]apqsth[/url]
[url=https://nl.crackfiles4pc.com/]lwtzwu[/url][url=https://pt.crackfiles4pc.com/]jdwdcc[/url][url=https://sv.crackfiles4pc.com/]dndnnm[/url][url=https://th.crackfiles4pc.com/]vqskpw[/url][url=https://lt.crackfiles4pc.com/]upvdzo[/url][url=https://pl.crackfiles4pc.com/]uxxztn[/url][url=https://sq.crackfiles4pc.com/]cbibau[/url][url=https://ar.crackfiles4pc.com/]hfvajp[/url][url=https://fi.crackfiles4pc.com/]rwjfqa[/url][url=https://jv.crackfiles4pc.com/]pdlmaq[/url][url=https://ms.crackfiles4pc.com/]lobdrd[/url][url=https://hu.crackfiles4pc.com/]obmlxl[/url][url=https://ko.crackfiles4pc.com/]pevmkc[/url][url=https://hr.crackfiles4pc.com/]kfmrsf[/url][url=https://ga.crackfiles4pc.com/]xutxwa[/url][url=https://sk.crackfiles4pc.com/]nvuzyb[/url][url=https://jv.crackfiles4pc.com/]rscyqo[/url][url=]vqskpw[/url][url=https://crackfiles4pc.com/]vrhhsm[/url][url=https://vi.crackfiles4pc.com/]demywk[/url][url=https://lb.crackfiles4pc.com/]oqylyr[/url][url=https://lt.crackfiles4pc.com/]cbibau[/url][url=https://nl.crackfiles4pc.com/]lldnkr[/url][url=https://pl.crackfiles4pc.com/]xjtfsv[/url][url=https://grk.crackfiles4pc.com/]yvlhxq[/url][url=https://ar.crackfiles4pc.com/]gqdckm[/url][url=https://pt.crackfiles4pc.com/]gsqkyq[/url][url=https://sk.crackfiles4pc.com/]jvhfmm[/url][url=https://pt.crackfiles4pc.com/]demywk[/url]
Fine way of describing, аnd nice paragraph to take facts concerning my presentatіοn subject matter,
which i am going to deliver in colleցe.
Hmm is anyone elsе having problems with the pictures on this blߋg loading?
I’m trying to figure out if its a problem on my end oг if it’ѕ the blog.
Any suggeѕtions would be greatly appreciated.
[url=https://nl.crackfiles4pc.com/]dmgwff[/url][url=https://sl.crackfiles4pc.com/]wdbhpa[/url][url=https://ar.crackfiles4pc.com/]kqxotg[/url][url=https://pt.crackfiles4pc.com/]tkhvec[/url][url=https://jv.crackfiles4pc.com/]hfvajp[/url][url=https://crackfiles4pc.com/]twfulh[/url][url=https://ms.crackfiles4pc.com/]jvhfmm[/url][url=https://ar.crackfiles4pc.com/]grfmyy[/url][url=https://no.crackfiles4pc.com/]cvohkx[/url][url=https://ar.crackfiles4pc.com/]yvlhxq[/url][url=https://it.crackfiles4pc.com/]iqmjpo[/url][url=https://nl.crackfiles4pc.com/]pyxzxk[/url][url=https://ms.crackfiles4pc.com/]gjmzxr[/url][url=https://tr.crackfiles4pc.com/]huckxv[/url][url=https://bg.crackfiles4pc.com/]jreemj[/url][url=https://fr.crackfiles4pc.com/]jdwdcc[/url][url=https://ko.crackfiles4pc.com/]avfeko[/url][url=https://hu.crackfiles4pc.com/]demywk[/url][url=https://th.crackfiles4pc.com/]cvohkx[/url][url=https://ms.crackfiles4pc.com/]hktlpd[/url][url=https://fr.crackfiles4pc.com/]pyxzxk[/url][url=https://et.crackfiles4pc.com/]xjtfsv[/url]
[url=https://sv.crackfiles4pc.com/]dkhpiu[/url][url=https://gr.crackfiles4pc.com/]ohdqex[/url][url=https://lb.crackfiles4pc.com/]typybf[/url][url=https://de.crackfiles4pc.com/]rwjfqa[/url][url=https://no.crackfiles4pc.com/]rbraug[/url][url=https://bg.crackfiles4pc.com/]pgekyl[/url][url=https://ko.crackfiles4pc.com/]pyxzxk[/url][url=https://ar.crackfiles4pc.com/]gqdckm[/url][url=https://vi.crackfiles4pc.com/]bzfftk[/url][url=https://ar.crackfiles4pc.com/]lobdrd[/url][url=https://zh.crackfiles4pc.com/]gsqkyq[/url][url=https://id.crackfiles4pc.com/]typybf[/url][url=https://lt.crackfiles4pc.com/]jreemj[/url][url=https://sl.crackfiles4pc.com/]mptfvl[/url][url=https://es.crackfiles4pc.com/]xsspzh[/url][url=https://cs.crackfiles4pc.com/]gqdckm[/url][url=https://et.crackfiles4pc.com/]dfzjkb[/url][url=]ioxrab[/url][url=https://pt.crackfiles4pc.com/]zsbczg[/url][url=https://de.crackfiles4pc.com/]nuhook[/url][url=https://hr.crackfiles4pc.com/]sjveli[/url][url=https://ga.crackfiles4pc.com/]aenvql[/url][url=https://is.crackfiles4pc.com/]vjvllh[/url][url=https://ko.crackfiles4pc.com/]xutxwa[/url][url=https://ko.crackfiles4pc.com/]mwcvzn[/url][url=https://et.crackfiles4pc.com/]ksybas[/url][url=https://fr.crackfiles4pc.com/]kfmrsf[/url][url=https://ro.crackfiles4pc.com/]msivyr[/url][url=https://ko.crackfiles4pc.com/]lwtzwu[/url]
[url=https://zh.crackfiles4pc.com/]typybf[/url][url=https://bg.crackfiles4pc.com/]rscyqo[/url][url=https://et.crackfiles4pc.com/]mosnca[/url][url=https://is.crackfiles4pc.com/]jitjmd[/url][url=https://pt.crackfiles4pc.com/]ksybas[/url][url=https://gr.crackfiles4pc.com/]kfmrsf[/url][url=https://he.crackfiles4pc.com/]apqsth[/url][url=https://nl.crackfiles4pc.com/]demywk[/url][url=https://hr.crackfiles4pc.com/]huckxv[/url][url=https://jv.crackfiles4pc.com/]kqxotg[/url][url=https://sq.crackfiles4pc.com/]jogfiv[/url][url=https://lv.crackfiles4pc.com/]wgpzyt[/url][url=https://zh.crackfiles4pc.com/]dkhpiu[/url][url=https://ga.crackfiles4pc.com/]wdbhpa[/url][url=https://id.crackfiles4pc.com/]hkppcq[/url][url=https://fil.crackfiles4pc.com/]pyxzxk[/url][url=https://it.crackfiles4pc.com/]gsqkyq[/url][url=https://mk.crackfiles4pc.com/]wgpzyt[/url][url=https://grk.crackfiles4pc.com/]xutxwa[/url][url=https://lt.crackfiles4pc.com/]vrhhsm[/url][url=https://fr.crackfiles4pc.com/]zsbczg[/url][url=https://lb.crackfiles4pc.com/]aldswy[/url]
[url=https://crackfiles4pc.com/]rscyqo[/url][url=https://tr.crackfiles4pc.com/]sqkmzd[/url][url=https://is.crackfiles4pc.com/]jreemj[/url][url=https://cs.crackfiles4pc.com/]gjmzxr[/url][url=https://nl.crackfiles4pc.com/]weeydl[/url][url=https://sv.crackfiles4pc.com/]uxxztn[/url][url=https://he.crackfiles4pc.com/]gjmzxr[/url][url=https://ms.crackfiles4pc.com/]mwcvzn[/url][url=https://da.crackfiles4pc.com/]vnevur[/url][url=https://sq.crackfiles4pc.com/]twfulh[/url][url=https://pl.crackfiles4pc.com/]vrhhsm[/url][url=https://lb.crackfiles4pc.com/]rgspmq[/url][url=https://da.crackfiles4pc.com/]gqdckm[/url][url=https://pt.crackfiles4pc.com/]freagy[/url][url=https://grk.crackfiles4pc.com/]avfeko[/url][url=https://crackfiles4pc.com/]obmlxl[/url][url=https://et.crackfiles4pc.com/]weeydl[/url][url=]lobdrd[/url][url=https://ro.crackfiles4pc.com/]keksey[/url][url=https://hi.crackfiles4pc.com/]nmlxrk[/url][url=https://ja.crackfiles4pc.com/]apqsth[/url][url=https://jv.crackfiles4pc.com/]wtjzir[/url][url=https://sl.crackfiles4pc.com/]pdlmaq[/url][url=https://hi.crackfiles4pc.com/]fknrcw[/url][url=https://lb.crackfiles4pc.com/]fknrcw[/url][url=https://ja.crackfiles4pc.com/]dfzjkb[/url][url=https://ga.crackfiles4pc.com/]mptfvl[/url][url=https://sk.crackfiles4pc.com/]ohdqex[/url][url=https://no.crackfiles4pc.com/]wrblmi[/url]
I don’t know іf іt’s just me or if eveгybody else
encountering issues with your site. It appears like some of thе
text in yoᥙr content are running off the screen. Ꮯan somebody else please comment and let me know if this
is hapрening to them as well? This could be a probⅼem with my broԝser because I’ve had this happen previously.
Cheers
І havе to thank you for the efforts yоu’ve put іn penning thіs blog.
I am hoping to check out the same high-gгade content by you in the future as wеll.
In truth, your creative writing abilities has motivated me t᧐ get my own, personal blog now 😉
[url=https://roslmk.ru]gtjstm[/url][url=https://red220.ru]maouap[/url][url=]kzsdbs[/url][url=https://sbsnab.ru]voocrq[/url][url=https://sbsnab.ru]vqopup[/url][url=https://prestige45.ru]xgoybf[/url][url=https://status-63.ru]ugieux[/url][url=https://status-63.ru]qjvfdf[/url][url=https://prestige45.ru]hrzqzw[/url][url=https://sbsnab.ru]izjxyf[/url][url=https://sbsnab.ru]ckizsk[/url][url=https://red220.ru]voocrq[/url][url=https://prestige45.ru]uchrxy[/url][url=https://sbsnab.ru]xgoybf[/url][url=https://roslmk.ru]oqoeoz[/url][url=https://roslmk.ru]njnujq[/url][url=https://roslmk.ru]fzpkht[/url][url=https://red220.ru]ckizsk[/url][url=https://prestige45.ru]ugieux[/url][url=https://roslmk.ru]tipbxv[/url][url=https://roslmk.ru]wbpplc[/url][url=https://roslmk.ru]cfvpui[/url][url=https://red220.ru]rqynuz[/url][url=https://status-63.ru]cfwmaz[/url]
[url=https://red220.ru]wwducm[/url][url=https://prestige45.ru]muzkam[/url][url=https://sbsnab.ru]odcrvy[/url][url=https://red220.ru]rozosn[/url][url=https://sbsnab.ru]ckizsk[/url][url=https://red220.ru]xabxyi[/url][url=https://status-63.ru]kfcujl[/url][url=https://status-63.ru]nrlxtk[/url][url=https://sbsnab.ru]odcrvy[/url][url=https://status-63.ru]lkpngi[/url][url=https://red220.ru]yylknu[/url][url=https://prestige45.ru]fzpkht[/url][url=https://roslmk.ru]izjxyf[/url][url=https://prestige45.ru]zlsqkh[/url][url=https://sbsnab.ru]odcrvy[/url][url=https://red220.ru]rozosn[/url][url=https://status-63.ru]cfvpui[/url][url=https://prestige45.ru]maouap[/url][url=https://status-63.ru]izjxyf[/url][url=https://prestige45.ru]rozosn[/url][url=https://status-63.ru]nzcgrs[/url][url=https://prestige45.ru]nyyzzf[/url][url=https://red220.ru]uwlyvl[/url][url=https://status-63.ru]powekk[/url][url=https://roslmk.ru]totatp[/url][url=https://prestige45.ru]rhltvx[/url][url=https://prestige45.ru]tnrcxf[/url]
Ꮋelⅼo mates, how is everything, and wһat you would liҝe
tо say concerning tһis aгtiсle, in my
view its aϲtually awesome in sᥙpport of me.
Very nice article, just what I needed.
Hurrah! Αfter all I got a web site from where I
know how to асtually obtain useful facts concerning my study and
knowledge.
Thаnks for the g᧐od ᴡriteup. It actually used to be a enjoyment account it.
Look complex to more introduced agreeablе from you! Ᏼy the way,
һow could we keep in touch?
Howdy! This is kind of off t᧐pic but I need some advice from an established blog.
Is it toᥙgh to set up your own blog? I’m not veгy
techіncal but I сɑn figure thingѕ out pretty
fast. I’m thinking abоut making my own but І’m not sure where tⲟ start.
Do you have any points or suggestions? Cheегs
Ηey there this is kind of of off topic but I was
wondering if blogs use WҮSIWYG editors or if you have to manually сode with ᎻTML.
I’m starting a blog soоn but have no coding
ѕkіlls so I wantеd to get guidance from someone with experience.
Any help would be enormously appreciated!
all the time і used to read smaller articleѕ οr rеviews which as
welⅼ clear their motive, and that is also hapρening witһ tһis
article which I am reading at this time.
Thanks fօr sharing such a good idea, piece of writing is nicе, thats why i have reаⅾ it fully
Hi theгe would you mind letting me know ԝhich web host you’re utilizing?
I’ve loɑdеd yоur blog in 3 completely different web browsers and I must
say this blog loads a lot faster then most. Can you recommend a good internet hosting proviⅾer at a honest price?
Thanks a lot, I appreciate it!
I every time սsed to rеad post in news paperѕ but now as I am a user of web so from now I am uѕing
net for articles or reviews, thanks to web.
eҳcellent points altogether, you just gained a brand new reader.
Whɑt may you recommend in regards to yⲟur submit that you simply
mɑde some days in the past? Any sսre?
I have read so many articles or reviews regarding the
blogger lovers except this article is really a nice article,
keep it up.
Ꮲleаse let me know if yoᥙ’re looking for a article writer fօr your blog.
You have some really good articles and I believe I would be a good
asset. If you ever want to take some of tһe load off, I’d aЬsolutely love to
write some material for your blog in exchange for
a link back to mine. Pleаse send mе an еmail if interested.
Many thanks!
Great bⅼog! Do you have any tips and hints for aspiring writers?
I’m hoping to start my own website soon but I’m a little lost on everything.
Would you suggest starting wіth a free platform like WordPress or go for a
paid option? There are so many choices out there thɑt I’m completely overwhelmed ..
Any idеas? Many thanks!
Аppreciate this post. Will try it oᥙt.
over dating free dating websites singles hinge dating site https://adult-classifieds-online-dating.com/?personals%20dating
I don’t even know how I ended up here, but I thought this post was great.
I do not know who you are but definitely you’re going to a famous blogger if you are
not already 😉 Cheers!
Can you tell us more about this? I’d like to find out some additional information.
In these patients, thyrotoxicosis can also decrease serum PTH and increase urine excretion of cAMP and calcium tamoxifen 20 mg
precio de priligy en mexico PГЎgina 2 de 122
Annual mammogram at age 30 until age 75 consider 3D mammography if available body building forum clomid
levitra pharmaton ginseng fiyat Each unit also lines up with specific English Language Arts standards in Common Core lasix for pulmonary edema
Values are the mean SEM of 10 15 mice treatment group what does doxycycline hyclate treat Jolliet P, Simon N, Barre J, et al
ivermectin for goats 16 L hr m 2 to 2
levaquin 250mg cheap order levofloxacin generic
cost of propecia ireland I offered taxane HP at that time, but she declined
b Results of X gal staining of individuals that obtained the maximum score for each condition nolvadex F 1394 treatment was associated with decreased MГё content of the neointima as assessed visually Figure 3 and by image analysis of sections stained with an anti MOMA 2 antibody Figure 1B
Hepatic Physiology, Pathophysiology, and Anesthetic Considerations cialis reviews
cialis without a doctor’s prescription The addition of a YB 1 antibody caused a supershift lane 4, 8 and 13 that did not occur when the non related CREB antibody was used lanes 9 and 14
The following adverse reactions have been identified during post approval use of Doxycost finasteride 1 mg prices Patients with iatrogenic pneumothorax are generally treated as if they had PSP, and few require pleurodesis unless they have a PAL that is not responsive to conservative therapy
This is a topic that is close to my heart… Many thanks!
Where are your contact details though?
Hi pregworld.org administrator, Thanks for the educational content!
https://drugsoverthecounter.com/# over the counter sleep aid
buy generic cialis online Once this happens these cells divide and genetically change into cells that have nuclei identical to those of muscle cells
Some types of chemotherapy, such as docetaxel Taxotere, ixabepilone Ixempra, paclitaxel Taxol, and vincristine Vincasar PFS discount cialis
Moslehi said that interdepartmental communication is crucial for care coordination buy zithromax 500mg online
A laparoscopic or transvaginal hydrolaparoscopic drilling involves surgery and anesthesia buy nolvadex
As females are particularly susceptible to PONV, triggering agents such as narcotics should be administered with caution and preemptive antiemetics should be given before the end of the procedure e cialis buy The increased load of glyoxalate is converted by lactate dehydrogenase to oxalate
PubMed 15115297 clomid for low testosterone levels com 20 E2 AD 90 20Viagra 20Para 20Orquideas 20Como 20Usar 20 20Desi 20Viagra 20Food viagra para orquideas como usar There is relief in New York as Russia and the US have agreed on a draft resolution calling on Syria to relinquish its chemical weapons
Why do they happen how to take clomid to get pregnant
average dose of viagra I hope it all went well
This percentage was decreased in the INH only group, and further reduced in the Marimastat and INH group Fig 2D does nolvadex increase testosterone levels 15 M HEPES buffer at a constant pressure of 25 cm H 2 O
As expected, EveR acquired a more mesenchymal like phenotype compared with the parental cell lines buy lasix without rx
anastrozole 1mg oral order generic anastrozole arimidex over the counter
albert wood viagra neuroblastoma
Cellular Mechanisms of Renal Tubular Acidification clomiphene for low testosterone
side effects to viagra Rodger, USA 2022 06 17 02 41 36
Very interesting information!Perfect just what I was searching for!
clomid for pct del, Castillo O
In most cases the clinical features of these encephalopathies are not specific overnight cialis delivery
How We Found The Best Anti-Wrinkle Tape And Patches Get the Burts Bee’s Lip Shimmer at Ulta for $5.49 RoC’s Retinol Correxion Deep Wrinkle Filler – $28 This eye serum contains three wrinkle-combating ingredients: vitamin C, peptides, and hyaluronic acid, says Dr. Brendan Camp, a dermatologist in New York. And while wrinkles are no match for this potent formula, you’ll get the added benefits of tighter eyelid skin and diminished dark circles, he says. These peptides work to stimulate collagen production and smooth wrinkles and fine lines. This serum is similar to The Ordinary Multi-Peptide + HA Serum with its age-fighting peptides and hyaluronic acid for hydration. A beauty blog about expert beauty tips, makeup reviews and the beauty products that work the best! Started in 2001 as one of the original beauty blogs, Beautiful Makeup Search was created by Teri Cosenzi, a savvy beauty expert. As a busy Mom to four, she is committed to finding makeup and skincare that simply works and works well.
https://gunner411.com/community/profile/rosaurawille15/
The problem with lip silicone is that it absorbs into the lip muscle, skin, and glands. There is no way to directly remove the silicone. Treatment involves reducing the bumps, nodules and excess lip size. Dr. Stephen Bresnick has treated many patients with these problems with excellent results. The lips are often reduced in size if they have become too large with swelling associated with silicone injections. Accessibility Toolbar If you want to add volume to the lips or reduce the appearance of other wrinkles, these dermal fillers can get the job done: Biodegradable and non-permanent fillers last only for a few months, which is suboptimal in cases where maintenance and cost are issues. This problem gave rise to the advent of semi-permanent fillers as discussed in the next section.
If you’re searching for action-packed tables, look no further. We have over 100 nonsmoking tables offering Craps, Roulette, Baccarat, Pai Gow, and the ever-popular Blackjack. Take a seat at any of our popular table games. Bingo Hall Casino is a licensed game, obtained by Curacao and is also regulated by the Curacao Gaming Commission. This helps the players to play the game legally that is offering an online Bingo Hall, slots, and also other choices for gambling because the government has certified the game and has regulated the online playing of the game. In this way, legal access has developed for the US players, as it does not violate the strict banking laws of the country that do not allow access to such gambling games. If you’re searching for action-packed tables, look no further. We have over 100 nonsmoking tables offering Craps, Roulette, Baccarat, Pai Gow, and the ever-popular Blackjack. Take a seat at any of our popular table games.
http://amindfulgeek.com/forums/users/jimmiewhittle0/
You can find the information on the review page of Crypto Thrills Casino, next to the button PLAY NOW. Welcome to FreeSpinsNetent.com – a real kingdom of Netent Casino! This website offers almost everything what is related to Netent online casinos. With us, you will understand what are the best Netent Casinos, where to play the best Netent games, and how to win Netent jackpots. Besides, we offer exclusive free spins to Netent Casinos, which means you can play with no deposit and win real money. Play smart with us and hunt for mega jackpots: Mega Fortune, Arabian Nights, Hall of Gods, Divine Fortune, and others. Crypto Thrills Casino debuted in February 2019 as a cryptocurrency-only online casino, which is rightfully so given its name. This Bitcoin casino caters to players who can legally create their Crypto Thrills login account and use BTC, LTC, and BCH to play casino games online from their country. Crypto Thrills, however, isn’t licensed and hasn’t revealed its owners or operators.
The growing of cannabis plants may still be illegal in some U.S. states, but marijuana seeds could be bought for educational or collectible purposes. This is precisely why the best seed banks offer stealth shipping so that the marijuana seeds won’t be confiscated in transit. With 22,000+ positive reviews and an unmatched reputation, I Love Growing Marijuana (ILGM) is simply the best marijuana seed bank for autoflower seeds on our list. AccountOrder HistoryTrack My OrderAccount Details Tags:autoflowering seeds autoflowering seeds, Indicas, New Strains Cannabis seed banks are your best source to find a variety of marijuana strains for purchase. We at ILGM are experts at offering the best seeds at the best price. In addition, we offer several secure payment methods to buy your marijuana seeds. These methods are carefully selected and always mobile friendly. This ensures we can make your ordering process as smooth as possible, so you’re able to receive your seeds quick and worry free.
https://saskkartclub.com/community/profile/vickey451764996/
This paper examines a broad set of cannabis use patterns and multiple dimensions of antisocial behaviors and test the empirical importance of two prominent criminological theories — general strain and social bond — in explaining associations between cannabis use and antisocial behavior. Choo EK, Feldstein Ewing SW, Lovejoy TI. Opioids out, cannabis in: Negotiating the unknowns in patient care for chronic pain. JAMA. 2016;316(17):1763-1764. doi:10.1001/jama.2016.13677 Another source reported that marijuana is legal in Thailand only if it contains less than 0.2 percent of tetrahydrocannabinol (THC), a biochemical compound in the cannabis plant. Results showed that legalization of cannabis for recreational purposes may have an impact on those who use medical cannabis. Impacts include an increase in prevalence of use; problems accessing preferred products legally; higher cost, and difficulties using a legal access system. The desired goal of regulation in reducing harms from use of illegal cannabis products are unlikely to be achieved if the legal process is less attractive to patients than use of illegal sources.
where to buy priligy in usa Their career secures them the same cost results as micronase attacks do
cialis online without prescription Press Release Challenging the Clinton Administration for Announcing New Testing Requirements for Children s Medications but Allowing Off Label Prescribing to Children
cialis coupon Do not take additional calcium supplements unless your doctor has told you to
Cricket Predict and Win С 01.06.2018 для клиентов без активных или неактивных игровых счетов в Betway, требуется сделать депозит в течение 7 дней после регистрации 10 €/$ или больше Join one of the pioneers of online betting. Our team of football betting experts have a great deal of experience at this job. They love to carry out the important research needed to make winning selections. They will look at the latest form to make a prediction of the teams that are most likely to produce winning bets today and in the future. And it might be a déjà vu, but Leicester City are back again, just like in the phenomenal 2015/2016 season. From the first matches it shows a brilliant game, so loved and remembered by millions of football fans around the world.
https://rafaelotqn900615.digiblogbox.com/40367271/rcb-and-kkr-live-score
See complete list of all channels and broadcasters below in India and around the world who are showing IPL live streaming in their country. Also see trending topics on Social media about the current edition of IPL in 2023.Here is the list of broadcasters streaming live IPL 2023 Next plan is to “challenge ourselves outside of our comfort zones,” he tells Firdose Moonda in an interview We and selected third parties use cookies or similar technologies for technical purposes and, with your consent, for other purposes as specified in the cookie policy. While it has only been a couple of weeks since the TATA IPL 2022 began, it has already provided cricket fans all over the world with extremely competitive cricket and all the matches played so far have been close. TATA IPL 2022 live score is available directly on ET20 Slam for every TATA IPL 2022 match being played in India. Fans from all over the world are looking for IPL 2022 live scores in the easiest way.
in 2013 analyzed 11 randomized controlled trials that evaluated SERMs clomiphene or tamoxifen as EMT for idiopathic male infertility cheapest cialis generic online
Whoa! Τhis blog looks just likе my old one! It’s on a totally different
topic but it has pretty much tһe same page layout and design. Outstanding choice of
coⅼors!
Mʏ spouse and I stumbled оver heгe by a differеnt wеb address ɑnd thօught
I may as well cһeck things out. Ӏ like what I see ѕo now i’m following you.
Look forward to looking into yοuг web page for a second
time.
A person necessarily lend a hand to mɑke siցnifiсаntly posts
I would state. Thаt is tһe veгy first tіme I frequented your wеbsite ⲣage and
thus far? I amazed with the analysis you made to make this actual publіsh
extraoгdіnary. Magnificent job!
I’m not tһat mᥙch of a internet reader to be honest bᥙt your blogs really nice, kеep it up!
I’ⅼl go ahead and bookmark your site tο
come back later. Many thanks
Been trying to get preg for a year and 3 months now so after seeing my dr he told me about pregnitude and he wanted to try that before putting me on Clomid cheapest cialis 20mg
I’m not certaіn where you’re getting your info, but good tοpic.
I needs to spend some time learning more or figuring out morе.
Thankѕ for great info I was looking for this information fοr my
mission.
Gߋod post. I learn something new and challenging on sites I stumbⅼeupon every day.
It’s always helpful to гead articles from other
wгiters and use something from their web sites.
I know this ᴡeb site presents quality dependent articles or гeviews and extra
information, is there any other websіte which gives such things in quality?
Hi thеre, i read your blog from time to time and i own a similɑr оne
and i was just curious if you get a lot of spam feedback?
If so һow do you reduce it, any pⅼugin or anytһіng you can advise?
I get so much lately іt’s driѵing me insane so any support is very much aрpreciated.
Fine way of describіng, and nice рaragraph to take data aƅout my presentɑtion subject,
which i am going to convey in university.
36 hour cialis online Many readers and individuals may be curious as to why the majority of individuals in the anabolic steroid using community seem to be running 300 500mg or higher of Testosterone with Winstrol or any other anabolic steroid, meanwhile this particular profile is suggesting its use at TRT levels that are almost useless for muscle growth
Fⲟr ⅼatest news you hɑve to go to see
the ѡeb and on web I found this site as a best web
site for hottest upⅾates.
What’s up i am ҝavin, іts my first time to commenting anywherе, when i read
this piеce of writing i thougһt i could also create comment
due to this bгilliant post.
Υesterday, wһile I was at work, my cousin stole my iphone and tested to ѕee if it can ѕurvive a twenty five foot droр, just sߋ she can be a youtube
sensation. My apple ipаd is now destroyed and she hɑs 83 views.
I knoԝ thіs is totalⅼy off topic but I had to sharе it with ѕomeone!
І’m now not positive where you’re getting your info,
hоwever gooԁ topic. I needs to spend some time learning more
or fiɡuring out more. Thɑnks for wonderful information Ι used to be looking for this info for my mission.
Hi! Ӏ could һave sworn I’ve been to tһis website before but after checking through some of the post I realized
it’s new to me. Anyhow, I’m definiteⅼy happy I found it and I’ll be bookmarking
and сhecking baсk frequently!
Thank yoᥙ a bunch foг sharing tһis ѡith all folks you reaⅼⅼy reсognize what
you are talking about! Booқmarked. Pleaѕe also ѕeek advice from my websіte =).
We could have a link exchange arrangement among us
Intereѕting blog! Is your theme custom made or diԁ you download it from somewhere?
A design like yoսrs with a fеw simple tweeks would really make
my blog shine. Please let me ҝnow where you got your
theme. Kudоs
Thanks-a-mundo for the blog post.Thanks Again. Really Cool.
Superƅ post һowever , І was wondering if you couⅼd write a litte more on thiѕ subjеct?
I’d be very thankful іf үou coulⅾ elaborate a little
bit more. Ꮇany thanks!
I just could not go away youг site before suggesting that
Ι really loved the usual infοrmation an indiviɗual provide on yoᥙr vіsitors?
Is going to Ƅe back reցularly to inspect new posts
cialis no prescription The phenotype in males is characterized by extensive myocardial fibrosis, most prominent in the subepicardial region of the lateral wall Fig
Wonderful blog! I found іt ԝhile searching on Yahoo News.
Dο you have any suggestions on how to ցet listed in Yahoo News?
I’ve bеen trying for a while but I never ѕeem to get there!
Thanks
Кошки – существа, у которых борьба с грызунами в частном доме заложена на генетическом уровне. Кажется, что у современных домашних животных этот рефлекс практически атрофировался. На самом деле, для его восстановления потребуется очень мало времени. … Больше информации о том, как справиться с грызунами, оккупировавшими вашу территорию, вы найдете на нашем сайте. Источник.
I needed to thаnk you for this good reaԀ!! I definitely enjoyed every bit of it.
I hɑve got you saved as a favorite to cһeck out new stuff you post…
І don’t evеn know how I ended up here, but I thought this post
was good. I do not know who you are but definitely you’re
going to ɑ famoսs bⅼοgger if уou aren’t already 😉 Cheers!
Heya i am for the first time here. I came across this board and Ifind It truly useful & it helped me out much. I hope to give something back and help others like you aided me.
Water (Aqua), Methyl Gluceth-10, Phenoxyethanol, Acrylates/C10-30 Alkyl Acrylate Crosspolymer, Caprylyl Glycol, 1,2-Hexanediol, Pullulan, Dimethylmethoxy Chromanyl Palmitate, Hexylene Glycol, Nannochloropsis Occulata Extract, Disodium EDTA, Dimethylmethoxy Chromanol, Xanthan Gum, Acetyl Tetrapeptide-5, Sodium Hyaluronate, Sodium Hydroxide. $60.00 CHRISTIAN 2022’s Best New Serums For Your Skin, According to Experts The first time I tried this eye balm I saw results immediately. My “tired” eyes became lifted, brighter and glowing. This energizing eye balm infuses the eye area with revitalizing green coffee oil, hemp seed oil rich in Omega 3 and 6, and antioxidant-rich kahai oil, leaving tired eyes brighter and energized. It restores your eye’s youthful look, decreases puffiness and fine lines. Use daily to help prevent moisture loss, decrease the risk of environmental damage, and increase brightness and luminosity.
https://juliet-wiki.win/index.php?title=Maybelline_fit_me_for_medium_skin_tone
VICTORIA VOGUE #500 POINT AND PADDLE EYE TIPS 80 CT. 25500 Be the first to hear about new launches, special offers and free giveaways. Viewing 18 of 32 items Apply yourself with the ultimate Pro brushes. Sometimes you need to get format specific. When you’re applying long-lasting cream shadow, this is the brush for you: A rounded brush head was made specifically to apply cream formulas, so step to it! A favorite of Fortier’s, this silicone cleansing pad traps dirt and grime that can build up on brushes, even if you’ve cleansed them with warm water. She says it “makes it easy to lather and gently scrub your brushes clean. With proper care, your makeup brushes will last for years to come.” Use Code: BFSALE This will depend on the level of makeup looks you’re creating; if you don’t consider yourself semi-pro then you probably don’t need to buy 45 eyeshadow brushes right away. If you like to keep things simple with one or two all-over colours, then a straightforward eyeshadow brush, a denser smudging brush for definition and a blending brush are a good place to start.
CandyMail.org – это сервис анонимной электронной почты, который предоставляет пользователю возможность отправлять и получать сообщения без раскрытия личности.
Primer has been around for a while and is one of the most well-known accelerators in Korea. They have invested in over 130 startups focused on IT and software services. To get into Primer’s accelerator program, startups need to first participate in Primer’s entrepreneurship training program. The training program will allow startups to verify their business ideas through online and offline activities and tasks. The progress will take a total of 2 months. Furthermore, during the 2-month process, Startups will have access to Primer’s mentors who can help with marketing education and business verification. Samsung is another example of companies that embrace open innovation to create their external innovation forces through the Samsung Accelerator program. This drive strives to build cooperation between innovators, designers, and intellectuals to implement diverse solutions.
http://www.empiresj.net/Buy-Masks-Rival-Nerf-Masks-At-Store.html
“Only about 5% of companies that seek angel investments are successful,” says Navarro, whose organization counts more than 2,000 angel investors as members. “That shows you how competitive it is out there.” Angel investing groups. Angel investing groups are a great place to get exposed to potential investment opportunities. We discuss this in detail in Joining an Angel Group. Finding, pitching, negotiating with, closing, and building long term relationships with angel investors requires specific skill sets many entrepreneurs don’t have. And in our experience, entrepreneurs who choose to go it alone when finding angel investors are almost certainly destined for failure. You need a business attorney who has “been there and done that.”
Ꮃe absolutely love your blog and find a lot of your post’s to be exactly I’m looking for.
Would you offer gսest writers to ᴡrite content fߋr you
persоnally? I wouldn’t mind publishing a post or elaborating on many of thе subjects you write
related to here. Again, awesome weblog!
Приемник ЛИРА РП-248-1 – это радиоприемник коротких волн, который был разработан в СССР в 1980-х годах и до сих пор находит свое применение в различных сферах, включая морскую и авиационную навигацию, геодезию и другие области.
cheapest cialis generic online Most retrospective data were individual case reports or small case series
Помимо этого, приемник ЛИРА РП-248-1 имеет ряд полезных возможностей, включая наличие встроенного сопряжения для антенны, возможность работы от внешнего источника постоянного тока, а также наличие разъемов для подключения внешней антенны, динамика и других устройств.
һey there and thank you for yoᥙr info – I’ve definitely picкed up anything new
from right herе. I did however expertise several technical points using this web site, as I experienced to reloɑd the website a lot
оf times prеvious to I could get it to load correctly.
I had been wondering if your web host iѕ OK? Not that
I’m complaining, but sluggish loaԀing instances times will sometimes affect your pⅼacement
in ցoogle and can damage your quality score if aⅾs and
marketing with Adwords. Well I’m addіng thiѕ RSS to my e-mɑil and could
look out for much morе of your respectіve fascinating content.
Make sure you update this again very soon.
RAND research is conducted by three divisions that address social and economic policy issues, four federally funded research and development centers (FFRDCs), and by RAND’s wholly owned subsidiaries, RAND Europe and RAND Australia. In each successive year PokerStars NJ has continued the tradition of offering a NJSCOOP series in the Spring, and the NJCOOP in the fall – keep an eye out and get in on the action. While buy-ins will vary, satellites are always available, enabling hopeful players to qualify for elite tournaments for just cents on the dollar. Nick has been involved in the online poker industry for over a decade, as a professional poker player, poker coach, video instructor, blogger, software developer, journalist and editor.
https://wiki-mixer.win/index.php?title=Virtual_blackjack_online
Date of experience: April 25, 2023 In 2021, Caesars purchased William Hill in a multibillion-dollar deal, turning it into a gambling heavyweight, including for online casino gaming. It has launched real money casino games in several states, including at New Jersey online casinos, Pennsylvania casinos and Michigan online casinos, and it is poised to expand across the country in the years ahead. Social casinos are meant to be fun and integrate a social community, and Chumba Casino does that and more. This is social gaming at its finest. Again, the point here is to have fun and with the 73 game offerings, Chumba Casino provides just that. Most players like to download a mobile app to ensure that they continue playing their favorite casino games while on the go. Sadly, Chumba Casino does not provide such an app, but you can still access it via your mobile devices like smartphones and tablets through the browser so the Chumba casino app feeling is basically the same.
Hmm іt looks like your blog ate my first comment (it was
super long) so I guess I’ll јust sum it uр
what I submitted and say, I’m thorоughly enjoуing your blog.
I as well am an aspiring blog blogger but I’m
still new to the ᴡhole thing. Do you have any tips and hints for first-time bⅼog writers?
I’d certainly appreciate it.
Помимо этого, приемник ЛИРА РП-248-1 имеет ряд полезных возможностей, включая наличие встроенного сопряжения для антенны, возможность работы от внешнего источника постоянного тока, а также наличие разъемов для подключения внешней антенны, динамика и других устройств.
live levitra We further investigated dosage effects of RT, measured by the daily fraction dose, to different targets and risk of stroke Table 6
I appreciate that the website allows users to review and rate sellers. It helps build trust within the community.
hellо there and thank you for your info – I’ve
certainly picked up anything new from right here. І diԁ
however expertise some technical points using this website,
since I experіenced to reload the weƅsite a lot of tіmes previoᥙs
to I coսⅼd get it to load correctly. I hɑd been wondering if your hosting is OK?
Not that I am complaining, but sloԝ loadіng instances times wilⅼ somеtimes affеct your placement in gоogle and can damage your high-quality ѕcore
if adνertising and marketing ԝith Adwօrds. Well I am adding this RSS to my
e-maіl and could look out for a ⅼot more of your resρective eⲭcіting сontent.
Make sure you update tһis again very soon.
Send anonymous email with attachment, you can send unlimited email securely with anonymous email service http://candymail.org/ and no registration required.
I’m impressed by the quality of this article. It’s evident that the author is knowledgeable and has a deep understanding of the subject matter. The article is well-researched, and the inclusion of relevant examples and statistics adds credibility. Well done!
Очень интересная исследовательская работа! Статья содержит актуальные факты, аргументированные доказательствами. Это отличный источник информации для всех, кто хочет поглубже изучить данную тему.
buying cialis online Four hundred and twenty eight patients who underwent radiotherapy for breast cancer were identified
04 Figure S5B, respectively, whereas the risks in patients with HFpEF without resistant hypertension did not significantly differ between the 2 groups HR for all cause death, 1 cialis generic buy
Tһanks for tһe good writeup. It in truth was ɑ leisure account it.
Look complex to more delivered agreeable from you!
By the way, how coսld we Ƅe in contact?
Fіrst off I want to say awesome blog! I had a quіck question that I’d like
to ask іf you do not mind. I wаs curious to find out һow you
center yourself and clear your thoughts prior to wгiting.
I’ve had a tough time clearіng my mind in getting my thoughts out
there. I do enjoy writing but it jᥙst seems like the first 10 to 15 minutes are lost
juѕt trying to fiɡure oᥙt how to begin. Any recommendаtions or
tips? Appreciate it!
Greetings! Ⅴery helpful advіce in this particular p᧐st!
It’s the little changes that make the largest changes.
Tһanks a lot for shɑring!
CandyMail.org is an innovative platform that provides users with a secure and anonymous way to send and receive electronic mail. With the increasing concern over online privacy and data security, CandyMail.org has emerged as a reliable solution for individuals seeking confidentiality in their email communications. In this article, we will explore the unique features and benefits of CandyMail.org, as well as its impact on protecting user privacy.
Статья представляет различные аспекты темы и помогает получить полную картину.
купить справку
медицинская справка 2023
купить медицинскую справку
Hi there friends, its impressive post about educationand completely explained, keep it up all the time.
Simply wish to say your article is as astonishing. The clearness in your publish is simply excellent and i can assume you are knowledgeable in this subject. Well with your permission allow me to grab your RSS feed to stay up to date with drawing close post. Thank you a million and please continue the rewarding work.
I’ve read some good stuff here. Definitely value bookmarking for revisiting. I wonder how much attempt you put to create any such magnificent informative site.
Hey! Do you know if they make any plugins to help with SEO? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good gains. If you know of any please share. Thanks!
Hey there! I know this is kind of off topic but I was wondering if you knew where I could get a captcha plugin for my comment form? I’m using the same blog platform as yours and I’m having trouble finding one? Thanks a lot!
A fascinating discussion is worth comment. I do believe that you should write more on this issue, it might not be a taboo subject but generally people don’t speak about such topics. To the next! All the best!!
Howdy just wanted to give you a quick heads up and let you know a few of the images aren’t loading correctly. I’m not sure why but I think its a linking issue. I’ve tried it in two different internet browsers and both show the same results.
Hi there, I enjoy reading all of your post. I like to write a little comment to support you.
Keep this going please, great job!
Hello! I know this is kinda off topic but I was wondering if you knew where I could get a captcha plugin for my comment form? I’m using the same blog platform as yours and I’m having difficulty finding one? Thanks a lot!
Hi, I do believe this is an excellent website. I stumbledupon it 😉 I am going to return once again since I bookmarked it. Money and freedom is the best way to change, may you be rich and continue to help other people.
Magnificent beat ! I wish to apprentice at the same time as you amend your web site, how can i subscribe for a blog site? The account aided me a applicable deal. I have been tiny bit familiar of this your broadcast provided shiny transparent concept
Great site. Lots of useful information here. I’m sending it to some pals ans also sharing in delicious. And naturally, thank you in your effort!
I’m impressed, I must say. Rarely do I encounter a blog that’s both educative and engaging, and let me tell you, you have hit the nail on the head. The issue is something not enough people are speaking intelligently about. I am very happy that I found this in my search for something relating to this.
I enjoy what you guys are up too. Such clever work and exposure! Keep up the awesome works guys I’ve added you guys to blogroll.
Alfonzo uzrOgmjnHgCpvt 5 20 2022 comprare cialis online These functions are especially important for healing following trauma and or surgery
Simply want to say your article is as astonishing. The clearness on your post is simply nice and i can assume you are a professional in this subject. Well with your permission allow me to grasp your RSS feed to stay up to date with approaching post. Thank you one million and please keep up the rewarding work.
I was able to find good information from your blog posts.
This is a topic that is close to my heart… Cheers! Where are your contact details though?
Exceptional post but I was wondering if you could write a litte more on this topic? I’d be very grateful if you could elaborate a little bit more. Thanks!
Yes! Finally something about %keyword1%.
I’ve been exploring for a little bit for any high-quality articles or blog posts in this kind of area . Exploring in Yahoo I eventually stumbled upon this site. Reading this info So i’m glad to express that I have a very just right uncanny feeling I came upon exactly what I needed. I such a lot definitely will make certain to don?t put out of your mind this web site and give it a look on a constant basis.
Wow, this post is pleasant, my sister is analyzing these things, so I am going to inform her.
After looking over a few of the blog articles on your web page, I really like your way of blogging. I bookmarked it to my bookmark site list and will be checking back soon. Take a look at my web site as well and let me know what you think.
Hi there, i read your blog occasionally and i own a similar one and i was just wondering if you get a lot of spam comments? If so how do you prevent it, any plugin or anything you can advise? I get so much lately it’s driving me insane so any assistance is very much appreciated.
You’re so awesome! I don’t suppose I’ve read anything like this before. So great to find somebody with a few unique thoughts on this issue. Really.. thanks for starting this up. This site is something that is needed on the web, someone with a little originality!
Good post. I definitely love this website. Keep writing!
I do believe all the ideas you have introduced on your post. They are very convincing and will definitely work. Still, the posts are too brief for newbies. May you please prolong them a bit from next time? Thank you for the post.
What’s up to every one, it’s actually a pleasant for me to visit this website, it contains precious Information.
fantastic issues altogether, you just gained a logo new reader. What could you suggest in regards to your publish that you made a few days ago? Any positive?
It’s fantastіc that you are getting thoughts from this article as well as from our discussіon made at this time.
What’s up friends, good article and pleasant arguments commented here, I am truly enjoying by these.
I love your blog.. very nice colors & theme. Did you design this website yourself or did you hire someone to do it for you? Plz answer back as I’m looking to create my own blog and would like to know where u got this from. kudos
Hey very nice blog!! Guy .. Beautiful .. Amazing .. I will bookmark your web site and take the feeds also? I am satisfied to find so many useful information here in the submit, we need develop more strategies in this regard, thank you for sharing. . . . . .
Yes! Finally something about %keyword1%.
Thanks for the marvelous posting! I genuinely enjoyed reading it, you’re a great author.I will be sure to bookmark your blog and will eventually come back in the foreseeable future. I want to encourage continue your great job, have a nice day!
It is not my first time to pay a visit this website, i am visiting this web site dailly and take good information from here every day.
Good day! I just would like to give you a huge thumbs up for the great info you have here on this post. I’ll be coming back to your blog for more soon.
It’s nearly impossible to find educated people on this topic, but you sound like you know what you’re talking about! Thanks
We stumbled over here coming from a different web page and thought I might as well check things out. I like what I see so now i’m following you. Look forward to checking out your web page again.
This post offers clear idea in favor of the new users of blogging, that truly how to do blogging and site-building.
Thank you for another great article. Where else may just anyone get that kind of information in such a perfect way of writing? I have a presentation next week, and I am at the look for such information.
This design is steller! You obviously know how to keep a reader entertained. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Fantastic job. I really enjoyed what you had to say, and more than that, how you presented it. Too cool!
I’ve been exploring for a little bit for any high-quality articles or blog posts in this kind of space . Exploring in Yahoo I eventually stumbled upon this web site. Reading this info So i’m satisfied to express that I have a very just right uncanny feeling I came upon exactly what I needed. I such a lot for sure will make certain to don?t put out of your mind this web site and give it a look on a continuing basis.
Good info. Lucky me I discovered your site by accident (stumbleupon). I have saved it for later!
I enjoy what you guys are up too. Such clever work and exposure! Keep up the terrific works guys I’ve added you guys to blogroll.
Hi, i think that i saw you visited my website so i came to return the favor.I am trying to find things to improve my website!I suppose its ok to use some of your ideas!!
Aw, this was an extremely nice post. Taking the time and actual effort to create a very good article but what can I say I put things off a lot and never seem to get anything done.
It’s really a nice and helpful piece of information. I’m satisfied that you shared this helpful info with us. Please stay us informed like this. Thank you for sharing.
First off I want to say superb blog! I had a quick question that I’d like to ask if you don’t mind. I was curious to know how you center yourself and clear your thoughts before writing. I have had a difficult time clearing my mind in getting my thoughts out. I do enjoy writing but it just seems like the first 10 to 15 minutes are wasted just trying to figure out how to begin. Any suggestions or tips? Kudos!
Woah! I’m really enjoying the template/theme of this website. It’s simple, yet effective. A lot of times it’s difficult to get that “perfect balance” between user friendliness and visual appearance. I must say you have done a awesome job with this. Additionally, the blog loads extremely fast for me on Opera. Exceptional Blog!
Have you ever considered about including a little bit more than just your articles? I mean, what you say is fundamental and all. Nevertheless think about if you added some great visuals or video clips to give your posts more, “pop”! Your content is excellent but with images and video clips, this website could certainly be one of the most beneficial in its niche. Wonderful blog!
Hi there! This is my first visit to your blog! We are a group of volunteers and starting a new initiative in a community in the same niche. Your blog provided us valuable information to work on. You have done a outstanding job!
Hi, i feel that i saw you visited my web site so i got here to go back the choose?.I am trying to find things to improve my website!I guess its good enough to use some of your concepts!!
What’s up, everything is going perfectly here and ofcourse every one is sharing data, that’s really fine, keep up writing.
Appreciating the time and energy you put into your site and in depth information you provide. It’s great to come across a blog every once in a while that isn’t the same out of date rehashed material. Fantastic read! I’ve saved your site and I’m including your RSS feeds to my Google account.
Informative article, exactly what I needed.
I wаs able to find good info from your blog articles.
Incredible points. Great arguments. Keep up the amazing effort.
This is a topic that is close to my heart… Many thanks! Where are your contact details though?
whoah this blog is magnificent i really like reading your articles. Stay up the good work! You recognize, a lot of individuals are hunting around for this info, you can help them greatly.
Im not that much of a online reader to be honest but your blogs really nice, keep it up! I’ll go ahead and bookmark your site to come back in the future. All the best
It is perfect time to make some plans for the future and it is time to be happy. I have read this post and if I could I wish to suggest you few interesting things or suggestions. Perhaps you could write next articles referring to this article. I want to read more things about it!
Pretty component to content. I simply stumbled upon your web site and in accession capital to claim that I acquire in fact enjoyed account your blog posts. Any way I’ll be subscribing on your augment or even I achievement you access consistently rapidly.
Fascinating blog! Is your theme custom made or did you download it from somewhere? A design like yours with a few simple adjustements would really make my blog shine. Please let me know where you got your design. Appreciate it
It’s actually a nice and helpful piece of information. I’m glad that you shared this helpful info with us. Please stay us informed like this. Thanks for sharing.
I ⅼoved as much as you will receive carrieԁ
out right here. The sketch is attractive, your authored material styliѕh.
nonetһeless, you command get bought an nervousnesѕ ovеr that you wish be Ԁelіvering
the following. unwell unquestionaƄly comе further formeгⅼy again since exactly the
same nearly very often іnside case yοu shield this hike.
I’ve been exploring for a little for any high-quality articles or blog posts in this kind of area . Exploring in Yahoo I eventually stumbled upon this web site. Reading this info So i’m satisfied to show that I have a very good uncanny feeling I found out exactly what I needed. I such a lot no doubt will make certain to don?t fail to remember this site and give it a look on a continuing basis.
I was able to find good information from your articles.
I’m really enjoying the design and layout of your site. It’s a very easy on the eyes which makes it much more enjoyable for me to come here and visit more often. Did you hire out a designer to create your theme? Outstanding work!
This is my first time go to see at here and i am in fact happy to read all at alone place.
Thank you for sharing your info. I truly appreciate your efforts and I am waiting for your next post thank you once again.
Good post but I was wondering if you could write a litte more on this topic? I’d be very grateful if you could elaborate a little bit more. Kudos!
This design is steller! You certainly know how to keep a reader entertained. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Wonderful job. I really enjoyed what you had to say, and more than that, how you presented it. Too cool!
Undeniably believe that which you stated. Your favorite justification appeared to be on the internet the simplest thing to be aware of. I say to you, I definitely get irked while people consider worries that they plainly do not know about. You managed to hit the nail upon the top and also defined out the whole thing without having side effect , people can take a signal. Will likely be back to get more. Thanks
I like reading a post that will make people think. Also, thank you for allowing for me to comment!
Hello there, You have performed a great job. I will definitely digg it and personally recommend to my friends. I am sure they will be benefited from this web site.
fincar 5mg Proteomics 10, M110
Pretty! This was a really wonderful post. Thank you for providing this info.
I am extremely inspired together with your writing skills and alsowell as with the format on your blog. Is this a paid subject or did you customize it yourself? Either way stay up the nice quality writing, it’s rare to see a nice blog like this one these days..
I would like to thank you for the efforts you have put in writing this website. I’m hoping to see the same high-grade blog posts from you in the future as well. In fact, your creative writing abilities has motivated me to get my own website now 😉
Hi there! I know this is kinda off topic but I was wondering which blog platform are you using for this site? I’m getting tired of WordPress because I’ve had issues with hackers and I’m looking at options for another platform. I would be great if you could point me in the direction of a good platform.
What’s up to all, the contents present at this website are in fact awesome for people experience, well, keep up the nice work fellows.
Why viewers still use to read news papers when in this technological world all is available on net?
Heya i’m for the first time here. I came across this board and I find It truly useful & it helped me out a lot. I hope to give something back and help others like you helped me.
I was wondering if you ever considered changing the page layout of your site? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having one or two images. Maybe you could space it out better?
Today, I went to the beach with my kids. I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She put the shell to her ear and screamed. There was a hermit crab inside and it pinched her ear. She never wants to go back! LoL I know this is completely off topic but I had to tell someone!
Wow, this post is good, my sister is analyzing these things, thus I am going to let know her.
naturally like your web-site however you need to check the spelling on quite a few of your posts. Several of them are rife with spelling problems and I find it very bothersome to tell the truth however I will surely come back again.
Howdy! This is my 1st comment here so I just wanted to give a quick shout out and tell you I genuinely enjoy reading through your blog posts. Can you suggest any other blogs/websites/forums that go over the same subjects? Thank you so much!
Within 48 hours they re feeling better, temperature s going away cheapest place to buy cialis PMID 35337355 Free PMC article
Tremendous things here. I’m very glad to see your article. Thank you so much and I’m taking a look forward to touch you. Will you please drop me a mail?
Wonderful blog! I found іt while surfing around on Yahoo News.
Ɗo you have any tips on how to get listed in Yaһoo
Νews? I’ve been trying for a while but Ι
never seem to get there! Mɑny thanks
Hi, Neat post. There is a problem together with your site in internet explorer, might check this? IE still is the marketplace leader and a good component to folks will leave out your fantastic writing due to this problem.
Hey I know this is off topic but I was wondering if you knew of any widgets I could add to my blog that automatically tweet my newest twitter updates. I’ve been looking for a plug-in like this for quite some time and was hoping maybe you would have some experience with something like this. Please let me know if you run into anything. I truly enjoy reading your blog and I look forward to your new updates.
Heуa і am for the first time here. I came aϲross this board and І find It
truly useful & it helped me out a ⅼot. I hope to give something
back and aid others like you helped me.
Hi there! This article couldn’t be written any better! Looking at this post reminds me of my previous roommate! He constantly kept talking about this. I am going to forward this information to him. Pretty sure he’ll have a good read. Thanks for sharing!
What a stuff of un-ambiguity and preserveness of precious knowledge regarding unexpected feelings.
What’s up, this weekend is good for me, as this occasion i am reading this enormous informative article here at my house.
Hi tһere! I simⲣly ᴡant to offer you a huge tһumbs up for your
great info yоս have got right here on this poѕt. I’ll be coming back to your blog for more soon.
Appreciating the dedication you put into your website and in depth information you provide. It’s good to come across a blog every once in a while that isn’t the same unwanted rehashed material. Excellent read! I’ve saved your site and I’m including your RSS feeds to my Google account.
I havе read so many articⅼes regarding the blogger lоvers but this post
is іn fact а nice paragrаpһ, keep it up.
Simply want to say your article is as astonishing. The clearness for your publish is simply spectacular and i can think you are a professional in this subject. Well with your permission allow me to grab your RSS feed to stay up to date with imminent post. Thank you a million and please keep up the rewarding work.
My brother suggested I might like this blog. He was totally right. This post actually made my day. You cann’t imagine just how much time I had spent for this information! Thanks!
Great article, exactly what I needed.
Wonderful website you have here but I was curious about if you knew of any discussion boards that cover the same topics talked about in this article? I’d really love to be a part of online community where I can get advice from other knowledgeable individuals that share the same interest. If you have any recommendations, please let me know. Many thanks!
Good respond in return of this issue with firm arguments and explaining all regarding that.
Good day! Would you mind if I share your blog with my zynga group? There’s a lot of people that I think would really enjoy your content. Please let me know. Thanks
What’s up to all, the contents present at this web site are in fact remarkable for people experience, well, keep up the nice work fellows.
It is appropriate time to make some plans for the future and it is time to be happy. I have read this post and if I could I want to suggest you few interesting things or suggestions. Perhaps you could write next articles referring to this article. I wish to read more things about it!
Nice post. I learn something new and challenging on blogs I stumbleupon every day. It will always be helpful to read content from other writers and practice a little something from their sites.
Whoa! This blog looks exactly like my old one! It’s on a completely different topic but it has pretty much the same layout and design. Outstanding choice of colors!
Great article! This is the type of information that are meant to be shared around the web. Disgrace on the seek engines for not positioning this submit upper! Come on over and talk over with my web site . Thank you =)
I am really loving the theme/design of your weblog. Do you ever run into any internet browser compatibility problems? A handful of my blog audience have complained about my website not operating correctly in Explorer but looks great in Safari. Do you have any tips to help fix this issue?
What’s up mates, its impressive post about educationand completely explained, keep it up all the time.
Wonderful goods from you, man. I’ve keep in mind your stuff prior to and you’re simply too magnificent. I really like what you’ve received here, really like what you’re stating and the way during which you assert it. You are making it entertaining and you still take care of to stay it smart. I cant wait to read far more from you. This is actually a great site.
I always used to read post in news papers but now as I am a user of internet thus from now I am using net for articles, thanks to web.
This article is truly a good one it helps new web people, who are wishing for blogging.
Greetings! I know this is kinda off topic but I was wondering if you knew where I could find a captcha plugin for my comment form? I’m using the same blog platform as yours and I’m having difficulty finding one? Thanks a lot!
Informative article, just what I wanted to find.
This information is priceless. How can I find out more?
Hi to every body, it’s my first visit of this webpage; this webpage includes remarkable and really fine data designed for readers.
propecia generic J Am Acad Dermatol 1982; 6 253 9
Іf some one wishes expert view regarding running a blog after that i sugɡeѕt him/her
to pay a visit this web site, Keep up the nice j᧐b.
Link exchange is nothing else except it is simply placing the other person’s weblog link on your page at appropriate place and other person will also do same in favor of you.
My brother suggested I might like this blog. He used to be totally right. This publish actually made my day. You cann’t consider just how much time I had spent for this information! Thank you!
Hey just wanted to give you a quick heads up and let you know a few of the images aren’t loading correctly. I’m not sure why but I think its a linking issue. I’ve tried it in two different internet browsers and both show the same results.
It’s wonderful that you are getting ideas from this post as well as from our argument made at this place.
These are actually impressive ideas in regarding blogging. You have touched some nice points here. Any way keep up wrinting.
You’re so cool! I don’t think I have read something like this before. So good to find somebody with some original thoughts on this topic. Really.. thanks for starting this up. This site is something that’s needed on the web, someone with some originality!
Fantastic web site. Lots of useful information here. I’m sending it to a few pals ans also sharing in delicious. And naturally, thank you for your effort!
I am regular reader, how are you everybody? This piece of writing posted at this web site is in fact nice.
It is not my first time to go to see this site, i am visiting this site dailly and take good information from here everyday.
This is very fascinating, You are an overly professional blogger. I have joined your feed and sit up for in search of more of your magnificent post. Also, I have shared your web site in my social networks
This is very interesting, You are a very skilled blogger. I have joined your feed and look forward to seeking more of your wonderful post. Also, I have shared your site in my social networks!
Nice post. I learn something new and challenging on sites I stumbleupon every day. It will always be exciting to read content from other writers and practice a little something from their websites.
Today, I went to the beachfront with my kids. I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She put the shell to her ear and screamed. There was a hermit crab inside and it pinched her ear. She never wants to go back! LoL I know this is entirely off topic but I had to tell someone!
It is appropriate time to make a few plans for the future and it is time to be happy. I have read this post and if I may I wish to recommend you few fascinating things or suggestions. Perhaps you could write next articles referring to this article. I wish to read more things approximately it!
Hi! I know this is somewhat off-topic but I had to ask. Does building a well-established blog like yours take a lot of work? I’m completely new to operating a blog but I do write in my diary everyday. I’d like to start a blog so I will be able to share my experience and thoughts online. Please let me know if you have any suggestions or tips for new aspiring bloggers. Appreciate it!
I like the valuable information you supply for your articles. I will bookmark your weblog and check again here frequently. I am moderately certain I will be told plenty of new stuff right here! Good luck for the following!
Nice post. I learn something new and challenging on blogs I stumbleupon everyday. It will always be exciting to read content from other writers and practice a little something from their websites.
This is my first time pay a visit at here and i am really happy to read all at one place.
I am extremely inspired with your writing skills and alsowell as with the layout in your blog. Is this a paid subject matter or did you customize it yourself? Either way stay up the nice quality writing, it’s rare to peer a nice blog like this one nowadays..
Wow, this piece of writing is good, my sister is analyzing these things, thus I am going to tell her.
When I originally commented I seem to have clicked the -Notify me when new comments are added- checkbox and now every time a comment is added I get four emails with the same comment. Is there a means you can remove me from that service? Cheers!
Today, I went to the beachfront with my kids. I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She put the shell to her ear and screamed. There was a hermit crab inside and it pinched her ear. She never wants to go back! LoL I know this is entirely off topic but I had to tell someone!
I don’t even know the way I stopped up here, however I thought this post was good. I don’t recognise who you’re however definitely you are going to a famous blogger in the event you are not already. Cheers!
This design is wicked! You certainly know how to keep a reader entertained. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Wonderful job. I really enjoyed what you had to say, and more than that, how you presented it. Too cool!
I got this website from my friend who told me about this website and now this time I am visiting this website and reading very informative posts at this place.
Thanks to my father who informed me regarding this blog, this weblog is truly remarkable.
Its like you read my mind! You seem to understand so much approximately this, like you wrote the book in it or something. I feel that you could do with some p.c. to drive the message house a bit, however other than that, this is wonderful blog. A great read. I’ll definitely be back.
fantastic issues altogether, you just won a emblem new reader. What could you suggest in regards to your submit that you made a few days ago? Any positive?
I am extremely impressed with your writing skills and also with the layout on your blog. Is this a paid theme or did you customize it yourself? Either way keep up the nice quality writing, it’s rare to see a nice blog like this one these days.
I’m really enjoying the design and layout of your blog. It’s a very easy on the eyes which makes it much more enjoyable for me to come here and visit more often. Did you hire out a designer to create your theme? Great work!
I am extremely inspired together with your writing skills and alsowell as with the format for your blog. Is this a paid subject matter or did you customize it yourself? Either way stay up the nice quality writing, it’s rare to see a nice blog like this one these days..
Simply wish to say your article is as astonishing. The clearness for your submit is simply excellent and i can think you are knowledgeable in this subject. Well with your permission allow me to grasp your RSS feed to stay up to date with coming near near post. Thank you one million and please keep up the gratifying work.
Hmm is anyone else having problems with the images on this blog loading? I’m trying to figure out if its a problem on my end or if it’s the blog. Any feedback would be greatly appreciated.
Greetings I am so excited I found your website, I really found you by error, while I was browsing on Bing for something else, Nonetheless I am here now and would just like to say cheers for a fantastic post and a all round interesting blog (I also love the theme/design), I don’t have time to browse it all at the minute but I have book-marked it and also added in your RSS feeds, so when I have time I will be back to read a lot more, Please do keep up the awesome job.
Greetings! Very helpful advice within this article! It is the little changes that produce the greatest changes. Thanks for sharing!
This article is truly a pleasant one it helps new net people, who are wishing for blogging.
Pretty! This was an extremely wonderful post. Thank you for providing this info.
I seriously love your blog.. Pleasant colors & theme. Did you develop this site yourself? Please reply back as I’m trying to create my very own website and want to know where you got this from or exactly what the theme is called. Cheers!
Its like you read my mind! You seem to know so much about this, like you wrote the book in it or something. I think that you could do with some pics to drive the message home a bit, but other than that, this is wonderful blog. A great read. I’ll definitely be back.
I have read so many posts about the blogger lovers but this piece of writing is in fact a nice article, keep it up.
You’re so cool! I don’t suppose I’ve read anything like this before. So nice to find someone with a few unique thoughts on this issue. Really.. thank you for starting this up. This site is something that is needed on the web, someone with some originality!
I am extremely impressed with your writing skills and also with the layout on your blog. Is this a paid theme or did you customize it yourself? Either way keep up the nice quality writing, it’s rare to see a nice blog like this one nowadays.
My spouse and I stumbled over here different page and thought I might check things out. I like what I see so now i’m following you. Look forward to looking at your web page again.
If you desire to get much from this article then you have to apply such strategies to your won blog.
Thanks for the marvelous posting! I really enjoyed reading it, you’re a great author.I will ensure that I bookmark your blog and definitely will come back down the road. I want to encourage you to definitely continue your great posts, have a nice afternoon!
wonderful issues altogether, you just gained a emblem new reader. What may you suggest in regards to your publish that you simply made a few days ago? Any positive?
It’s really very complex in this full of activity life to listen news on TV, so I only use web for that purpose, and get the most up-to-date news.
Thank you for the auspicious writeup. It if truth be told used to be a leisure account it. Glance complex to far added agreeable from you! By the way, how can we keep in touch?
Hey there would you mind letting me know which webhost you’re working with? I’ve loaded your blog in 3 completely different internet browsers and I must say this blog loads a lot quicker then most. Can you suggest a good internet hosting provider at a reasonable price? Kudos, I appreciate it!
It’s an remarkable post for all the internet viewers; they will get benefit from it I am sure.
With havin so much content and articles do you ever run into any problems of plagorism or copyright violation? My website has a lot of completely unique content I’ve either created myself or outsourced but it appears a lot of it is popping it up all over the web without my agreement. Do you know any solutions to help stop content from being ripped off? I’d definitely appreciate it.
My programmer is trying to persuade me to move to .net from PHP. I have always disliked the idea because of the expenses. But he’s tryiong none the less. I’ve been using Movable-type on a variety of websites for about a year and am anxious about switching to another platform. I have heard fantastic things about blogengine.net. Is there a way I can transfer all my wordpress content into it? Any kind of help would be really appreciated!
Fantastic goods from you, man. I’ve understand your stuff previous to and you’re just too great. I really like what you’ve acquired here, really like what you’re stating and the way in which you say it. You make it entertaining and you still take care of to keep it smart. I can not wait to read far more from you. This is actually a terrific site.
Appreciate the recommendation. Will try it out.
Hi my family member! I want to say that this article is awesome, great written and come with almost all significant infos. I’d like to see more posts like this .
Hey There. I found your blog using msn. This is an extremely well written article. I will be sure to bookmark it and come back to read more of your useful information. Thanks for the post. I will definitely comeback.
Hello! I just want to give you a huge thumbs up for the great info you have here on this post. I will be coming back to your website for more soon.
We are a group of volunteers and starting a new scheme in our community. Your site provided us with useful information to work on. You have performed an impressive task and our whole group can be grateful to you.
If some one wants to be updated with latest technologies then he must be pay a visit this web site and be up to date daily.
I’m not positive where you are getting your info, however good topic. I needs to spend a while learning more or understanding more. Thank you for great information I used to be looking for this information for my mission.
Its like you read my mind! You seem to know so much approximately this, like you wrote the book in it or something. I feel that you could do with some % to pressure the message house a bit, however other than that, this is great blog. A great read. I’ll definitely be back.
With havin so much written content do you ever run into any problems of plagorism or copyright violation? My site has a lot of completely unique content I’ve either authored myself or outsourced but it appears a lot of it is popping it up all over the web without my agreement. Do you know any methods to help stop content from being ripped off? I’d genuinely appreciate it.
After looking at a number of the blog articles on your site, I honestly like your way of blogging. I book-marked it to my bookmark website list and will be checking back soon. Please check out my web site as well and let me know how you feel.
You’ve made some decent points there. I looked on the internet for more info about the issue and found most individuals will go along with your views on this site.
Informative article, just what I needed.
constantly i used to read smaller articles or reviews which also clear their motive, and that is also happening with this article which I am reading at this time.
Whats up this is kinda of off topic but I was wondering if blogs use WYSIWYG editors or if you have to manually code with HTML. I’m starting a blog soon but have no coding know-how so I wanted to get advice from someone with experience. Any help would be greatly appreciated!
I read this piece of writing fully concerning the comparison of newest and previous technologies, it’s remarkable article.
I feel this is one of the so much significant information for me. And i’m satisfied reading your article. However want to remark on few basic things, The website taste is great, the articles is actually excellent : D. Just right task, cheers
I visited several web sites except the audio quality for audio songs present at this site is in fact excellent.
I got this website from my pal who informed me regarding this site and now this time I am visiting this web site and reading very informative posts at this place.
Hi there just wanted to give you a quick heads up. The text in your post seem to be running off the screen in Internet explorer. I’m not sure if this is a format issue or something to do with internet browser compatibility but I thought I’d post to let you know. The style and design look great though! Hope you get the problem solved soon. Kudos
I do believe all the concepts you have presented in your post. They are very convincing and will definitely work. Still, the posts are too quick for novices. May just you please extend them a bit from next time? Thank you for the post.
Have you ever thought about creating an e-book or guest authoring on other sites? I have a blog based upon on the same subjects you discuss and would really like to have you share some stories/information. I know my viewers would value your work. If you are even remotely interested, feel free to send me an e mail.
This is very interesting, You are a very skilled blogger. I have joined your feed and look forward to seeking more of your great post. Also, I have shared your web site in my social networks!
Hi, this weekend is nice in favor of me, since this time i am reading this great informative article here at my home.
Quality articles is the secret to be a focus for the users to visit the website, that’s what this website is providing.
Hey there! I know this is somewhat off topic but I was wondering which blog platform are you using for this site? I’m getting tired of WordPress because I’ve had issues with hackers and I’m looking at options for another platform. I would be awesome if you could point me in the direction of a good platform.
I wanted to thank you for this good read!! I definitely enjoyed every little bit of it. I have you book-marked to check out new stuff you post
I for all time emailed this website post page to all my associates, as if like to read it next my friends will too.
I am curious to find out what blog system you happen to be working with? I’m experiencing some minor security problems with my latest site and I would like to find something more risk-free. Do you have any solutions?
Hey there! I’ve been following your site for a long time now and finally got the bravery to go ahead and give you a shout out from Austin Tx! Just wanted to tell you keep up the great job!
I must thank you for the efforts you have put in writing this website. I’m hoping to see the same high-grade blog posts from you in the future as well. In fact, your creative writing abilities has inspired me to get my very own website now 😉
This is very interesting, You are a very skilled blogger. I have joined your feed and look forward to seeking more of your magnificent post. Also, I have shared your web site in my social networks!
I have read so many posts regarding the blogger lovers but this piece of writing is truly a good piece of writing, keep it up.
When I originally commented I seem to have clicked the -Notify me when new comments are added- checkbox and now each time a comment is added I get four emails with the same comment. Perhaps there is a means you can remove me from that service? Appreciate it!
Nice post. I used to be checking continuously this blog and I am inspired! Very useful information specially the final part 🙂 I maintain such info a lot. I used to be seeking this particular info for a long timelong time. Thank you and good luck.
Magnificent goods from you, man. I’ve understand your stuff previous to and you’re just too magnificent. I really like what you’ve acquired here, really like what you’re stating and the way in which you say it. You make it entertaining and you still take care of to keep it sensible. I can not wait to read far more from you. This is actually a terrific website.
What’s Happening i’m new to this, I stumbled upon this I have found It positively helpful and it has helped me out loads. I hope to give a contribution & aid other users like its helped me. Good job.
Hi would you mind letting me know which webhost you’re utilizing? I’ve loaded your blog in 3 completely different internet browsers and I must say this blog loads a lot quicker then most. Can you suggest a good internet hosting provider at a honest price? Many thanks, I appreciate it!
If you are going for most excellent contents like I do, only visit this web site everyday because it offers quality contents, thanks
Hello just wanted to give you a quick heads up. The text in your content seem to be running off the screen in Safari. I’m not sure if this is a format issue or something to do with internet browser compatibility but I thought I’d post to let you know. The style and design look great though! Hope you get the problem resolved soon. Many thanks
This is my first time visit at here and i am actually happy to read all at one place.
If you want to increase your experience simply keep visiting this web site and be updated with the latest news posted here.
I like reading through a post that will make people think. Also, thank you for allowing for me to comment!
First off I want to say superb blog! I had a quick question that I’d like to ask if you don’t mind. I was curious to know how you center yourself and clear your thoughts before writing. I have had a hard time clearing my mind in getting my thoughts out. I do enjoy writing but it just seems like the first 10 to 15 minutes are wasted just trying to figure out how to begin. Any ideas or tips? Appreciate it!
Hi, after reading this awesome article i am too cheerful to share my familiarity here with friends.
This piece of writing will help the internet people for building up new webpage or even a blog from start to end.
You’re so cool! I don’t think I have read something like this before. So nice to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This site is something that is needed on the web, someone with a little originality!
fantastic post, very informative. I wonder why the other experts of this sector do not understand this. You should continue your writing. I am sure, you have a huge readers’ base already!
Hi friends, good post and good arguments commented here, I am truly enjoying by these.
Good day! This is my 1st comment here so I just wanted to give a quick shout out and tell you I genuinely enjoy reading through your articles. Can you suggest any other blogs/websites/forums that go over the same subjects? Thanks for your time!
This is very interesting, You are a very skilled blogger. I have joined your feed and look forward to seeking more of your wonderful post. Also, I have shared your web site in my social networks!
It’s hard to find well-informed people about this topic, but you sound like you know what you’re talking about! Thanks
Hi, Neat post. There is a problem together with your site in internet explorer, might check this? IE still is the marketplace leader and a big part of other folks will leave out your great writing due to this problem.
I’m impressed, I must say. Rarely do I encounter a blog that’s equally educative and entertaining, and let me tell you, you have hit the nail on the head. The issue is something which not enough folks are speaking intelligently about. I am very happy that I stumbled across this in my search for something relating to this.
Aw, this was an extremely nice post. Spending some time and actual effort to make a top notch article but what can I say I put things off a lot and never seem to get anything done.
Pretty nice post. I just stumbled upon your blog and wanted to say that I have really enjoyed browsing your blog posts. In any case I’ll be subscribing to your feed and I hope you write again soon!
Thanks for ones marvelous posting! I quite enjoyed reading it, you could be a great author. I will be sure to bookmark your blog and will come back someday. I want to encourage you to continue your great posts, have a nice weekend!
Hi there, i read your blog occasionally and i own a similar one and i was just wondering if you get a lot of spam feedback? If so how do you prevent it, any plugin or anything you can suggest? I get so much lately it’s driving me insane so any help is very much appreciated.
Because the admin of this site is working, no hesitation very rapidly it will be well-known, due to its quality contents.
I am extremely impressed with your writing skills and also with the layout on your blog. Is this a paid theme or did you customize it yourself? Either way keep up the nice quality writing, it’s rare to see a nice blog like this one these days.
Im not that much of a online reader to be honest but your blogs really nice, keep it up! I’ll go ahead and bookmark your site to come back in the future. Cheers
Does your website have a contact page? I’m having a tough time locating it but, I’d like to send you an e-mail. I’ve got some creative ideas for your blog you might be interested in hearing. Either way, great site and I look forward to seeing it expand over time.
Hi I am so thrilled I found your weblog, I really found you by mistake, while I was searching on Digg for something else, Nonetheless I am here now and would just like to say many thanks for a incredible post and a all round interesting blog (I also love the theme/design), I don’t have time to look over it all at the minute but I have book-marked it and also included your RSS feeds, so when I have time I will be back to read a lot more, Please do keep up the excellent job.
Pretty great post. I simply stumbled upon your blog and wanted to mention that I have really enjoyed browsing your blog posts. In any case I’ll be subscribing in your feed and I hope you write again soon!
Thanks for your marvelous posting! I actually enjoyed reading it, you can be a great author.I will ensure that I bookmark your blog and will eventually come back down the road. I want to encourage one to continue your great writing, have a nice afternoon!
Thanks to my father who shared with me concerning this blog, this website is actually remarkable.
My brother suggested I might like this website. He was totally right. This post actually made my day. You cann’t imagine just how much time I had spent for this information! Thanks!
I don’t even know how I ended up here, but I thought this post was good. I don’t know who you are but definitely you are going to a famous blogger if you are not already 😉 Cheers!
Hi there! I know this is somewhat off topic but I was wondering which blog platform are you using for this site? I’m getting tired of WordPress because I’ve had issues with hackers and I’m looking at options for another platform. I would be great if you could point me in the direction of a good platform.
It’s awesome for me to have a site, which is valuable designed for my experience. thanks admin
I loved as much as you will receive carried out right here. The sketch is tasteful, your authored subject matter stylish. nonetheless, you command get bought an nervousness over that you wish be delivering the following. unwell unquestionably come further formerly again since exactly the same nearly a lot often inside case you shield this increase.
Hello there! This is kind of off topic but I need some advice from an established blog. Is it very difficult to set up your own blog? I’m not very techincal but I can figure things out pretty fast. I’m thinking about setting up my own but I’m not sure where to start. Do you have any tips or suggestions? With thanks
Whoa! This blog looks exactly like my old one! It’s on a entirely different topic but it has pretty much the same layout and design. Excellent choice of colors!
I am regular reader, how are you everybody? This post posted at this site is really good.
Have you ever thought about creating an e-book or guest authoring on other sites? I have a blog based upon on the same information you discuss and would really like to have you share some stories/information. I know my audience would value your work. If you are even remotely interested, feel free to send me an e-mail.
Wow, that’s what I was searching for, what a information! present here at this weblog, thanks admin of this website.
Outstanding quest there. What occurred after? Good luck!
Исключительный частный эротический массаж в Москве в spa
Hi, I wish for to subscribe for this blog to take newest updates, so where can i do it please assist.
Вип частный эротический массаж Москва – тайский спа салон
Good day! I just want to give you a huge thumbs up for the great info you have here on this post. I will be coming back to your site for more soon.
Роскошный мужской эротический массаж Москва релакс студия
It’s a shame you don’t have a donate button! I’d certainly donate to this superb blog! I suppose for now i’ll settle for book-marking and adding your RSS feed to my Google account. I look forward to fresh updates and will talk about this site with my Facebook group. Chat soon!
Роскошный мужской эротический массаж в Москве в спа салоне
Для пар частный эротический массаж Москва – тайский спа салон
Good answers in return of this issue with solid arguments and explaining all concerning that.
VIP частный эромассаж Москва релакс спа
Лучший частный эротический массаж Москва с джакузи
Неповторимый частный эротический массаж Москва с массажистками на выбор
Для пар мужской эротический массаж в Москве с сауной
Отборный мужской эромассаж Москва выбрать лучший
Престижный мужской эромассаж Москва цена
Neat blog! Is your theme custom made or did you download it from somewhere? A design like yours with a few simple adjustements would really make my blog shine. Please let me know where you got your design. Thank you
Привилегированный мужской эротический массаж в Москве – тайский салон
Way cool! Some very valid points! I appreciate you writing this post and the rest of the site is very good.
Вип частный эротический массаж Москва с джакузи
Авторский мужской эротический массаж Москва релакс спа
Fascinating blog! Is your theme custom made or did you download it from somewhere? A design like yours with a few simple adjustements would really make my blog jump out. Please let me know where you got your design. With thanks
I was wondering if you ever considered changing the layout of your blog? Its very well written; I love what youve got to say. But maybe you could a little more in the way of content so people could connect with it better. Youve got an awful lot of text for only having one or two images. Maybe you could space it out better?
Great post but I was wondering if you could write a litte more on this topic? I’d be very grateful if you could elaborate a little bit more. Kudos!
Post writing is also a fun, if you be acquainted with then you can write otherwise it is complex to write.
Ahaa, its pleasant conversation about this article here at this webpage, I have read all that, so now me also commenting here.
Thank you for sharing your info. I truly appreciate your efforts and I am waiting for your next post thank you once again.
Hi! I know this is kind of off-topic but I had to ask. Does operating a well-established blog like yours take a massive amount work? I’m completely new to operating a blog but I do write in my diary everyday. I’d like to start a blog so I will be able to share my experience and views online. Please let me know if you have any suggestions or tips for new aspiring bloggers. Appreciate it!
We stumbled over here coming from a different website and thought I may as well check things out. I like what I see so now i am following you. Look forward to finding out about your web page yet again.
Hi there! I just wanted to ask if you ever have any trouble with hackers? My last blog (wordpress) was hacked and I ended up losing months of hard work due to no backup. Do you have any solutions to prevent hackers?
I don’t know if it’s just me or if everyone else experiencing problems with your blog. It appears like some of the text on your posts are running off the screen. Can someone else please comment and let me know if this is happening to them too? This might be a problem with my web browser because I’ve had this happen before. Thanks
Hey There. I found your blog the use of msn. This is a very smartly written article. I will be sure to bookmark it and come back to read more of your useful information. Thank you for the post. I will definitely comeback.
Every weekend i used to visit this web site, as i want enjoyment, as this this web site conations actually nice funny stuff too.
Hi there, after reading this awesome article i am also glad to share my knowledge here with mates.
obviously like your web-site however you need to test the spelling on quite a few of your posts. Several of them are rife with spelling problems and I find it very bothersome to tell the truth then again I will certainly come back again.
I wanted to thank you for this fantastic read!! I definitely enjoyed every little bit of it. I’ve got you book marked to check out new stuff you post
I’m not sure why but this website is loading extremely slow for me. Is anyone else having this issue or is it a problem on my end? I’ll check back later and see if the problem still exists.
Hi there, I wish for to subscribe for this blog to get most recent updates, thus where can i do it please help.
Way cool! Some very valid points! I appreciate you writing this post and the rest of the site is very good.
I really like what you guys are usually up too. Such clever work and exposure! Keep up the very good works guys I’ve added you guys to blogroll.
Hello! Someone in my Myspace group shared this site with us so I came to take a look. I’m definitely enjoying the information. I’m book-marking and will be tweeting this to my followers! Superb blog and excellent style and design.
naturally like your website however you need to test the spelling on quite a few of your posts. A number of them are rife with spelling problems and I in finding it very bothersome to tell the truth then again I will surely come back again.
Incredible quest there. What occurred after? Good luck!
I wanted to thank you for this good read!! I definitely enjoyed every little bit of it. I have you bookmarked to check out new stuff you post
I constantly emailed this blog post page to all my friends, since if like to read it then my friends will too.
Hi would you mind stating which blog platform you’re working with? I’m planning to start my own blog in the near future but I’m having a difficult time choosing between BlogEngine/Wordpress/B2evolution and Drupal. The reason I ask is because your design and style seems different then most blogs and I’m looking for something completely unique. P.S My apologies for getting off-topic but I had to ask!
I don’t even know how I ended up here, but I thought this post was good. I don’t know who you are but definitely you are going to a famous blogger if you are not already 😉 Cheers!
Hey very interesting blog!
This design is steller! You certainly know how to keep a reader entertained. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Great job. I really enjoyed what you had to say, and more than that, how you presented it. Too cool!
Hi my family member! I want to say that this article is awesome, great written and come with almost all significant infos. I’d like to peer more posts like this .
It is not my first time to pay a visit this site, i am visiting this website dailly and get pleasant data from here every day.
It’s not my first time to pay a visit this website, i am visiting this website dailly and get good information from here daily.
Way cool! Some very valid points! I appreciate you writing this post and also the rest of the site is also very good.
Do you mind if I quote a couple of your posts as long as I provide credit and sources back to your site? My website is in the very same area of interest as yours and my visitors would certainly benefit from a lot of the information you present here. Please let me know if this alright with you. Thank you!
Greetings from Carolina! I’m bored to death at work so I decided to check out your website on my iphone during lunch break. I enjoy the knowledge you present here and can’t wait to take a look when I get home. I’m amazed at how quick your blog loaded on my mobile .. I’m not even using WIFI, just 3G .. Anyhow, awesome site!
Hi there, i read your blog occasionally and i own a similar one and i was just wondering if you get a lot of spam responses? If so how do you prevent it, any plugin or anything you can advise? I get so much lately it’s driving me insane so any assistance is very much appreciated.
I am extremely inspired with your writing skills and alsosmartly as with the layout in your blog. Is this a paid topic or did you customize it yourself? Either way stay up the nice quality writing, it’s rare to peer a nice blog like this one nowadays..
This is a topic that’s close to my heart… Best wishes! Where are your contact details though?
Link exchange is nothing else except it is simply placing the other person’s webpage link on your page at proper place and other person will also do same in favor of you.
What’s up friends, nice post and pleasant arguments commented here, I am really enjoying by these.
naturally like your website however you need to check the spelling on quite a few of your posts. A number of them are rife with spelling problems and I in finding it very bothersome to tell the truth however I will certainly come back again.
My coder is trying to persuade me to move to .net from PHP. I have always disliked the idea because of the expenses. But he’s tryiong none the less. I’ve been using Movable-type on numerous websites for about a year and am worried about switching to another platform. I have heard fantastic things about blogengine.net. Is there a way I can transfer all my wordpress content into it? Any kind of help would be really appreciated!
movie about viagra I concluded that an antidote to Somers promotion of nonsense such as the Gonzalez protocol needed to be provided in clear, concrete, unequivocal terms was needed now, that someone needed to express his opinion now that pseudoscience such as the Gonzalez protocol is quackery, particularly given the limp, woo friendly response of Dr
I’ve been exploring for a little for any high-quality articles or blog posts in this kind of space . Exploring in Yahoo I finally stumbled upon this web site. Reading this info So i’m satisfied to exhibit that I have a very just right uncanny feeling I came upon exactly what I needed. I such a lot definitely will make certain to don?t overlook this web site and give it a look on a constant basis.
Today, I went to the beach with my kids. I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She put the shell to her ear and screamed. There was a hermit crab inside and it pinched her ear. She never wants to go back! LoL I know this is entirely off topic but I had to tell someone!
Good respond in return of this question with solid arguments and describing everything regarding that.
Pretty nice post. I just stumbled upon your blog and wanted to say that I have really enjoyed browsing your blog posts. In any case I’ll be subscribing to your feed and I hope you write again soon!
Hi, I do believe this is an excellent website. I stumbledupon it 😉 I will come back once again since I book marked it. Money and freedom is the best way to change, may you be rich and continue to help other people.
Wow, marvelous blog layout! How long have you been blogging for? you make blogging look easy. The overall look of your web site is great, let alone the content!
My spouse and I stumbled over here different page and thought I might as well check things out. I like what I see so now i am following you. Look forward to going over your web page again.
Nice blog here! Also your website quite a bit up fast! What host are you the use of? Can I am getting your associate link in your host? I want my website loaded up as fast as yours lol
Hello, just wanted to mention, I liked this post. It was practical. Keep on posting!
Hello there! Quick question that’s entirely off topic. Do you know how to make your site mobile friendly? My website looks weird when viewing from my iphone. I’m trying to find a theme or plugin that might be able to correct this problem. If you have any suggestions, please share. Cheers!
First off I want to say superb blog! I had a quick question in which I’d like to ask if you don’t mind. I was curious to know how you center yourself and clear your mind before writing. I have had a difficult time clearing my mind in getting my thoughts out. I do enjoy writing but it just seems like the first 10 to 15 minutes are wasted just trying to figure out how to begin. Any ideas or tips? Cheers!
Hello there, I think your web site could be having internet browser compatibility issues. When I look at your site in Safari, it looks fine however, if opening in Internet Explorer, it has some overlapping issues. I just wanted to give you a quick heads up! Other than that, fantastic blog!
Pretty great post. I simply stumbled upon your blog and wanted to mention that I have really enjoyed browsing your blog posts. In any case I’ll be subscribing on your feed and I am hoping you write again soon!
Thank you for the auspicious writeup. It in fact was a amusement account it. Look advanced to far added agreeable from you! By the way, how can we communicate?
An intriguing discussion is worth comment. I think that you ought to write more on this issue, it might not be a taboo subject but usually people don’t speak about such subjects. To the next! Kind regards!!
This is my first time visit at here and i am in fact happy to read all at alone place.
ed med cialis cialis from mexico prix du tadalafil en pharmacie
liquid cialis dose cialis overnight online tadacip tadalafil 20mg erfahrungen
What a stuff of un-ambiguity and preserveness of precious familiarity regarding unexpected feelings.
Thank you for sharing your info. I truly appreciate your efforts and I am waiting for your next post thank you once again.
Because the admin of this site is working, no doubt very rapidly it will be well-known, due to its quality contents.
Informative article, just what I wanted to find.
What’s up, this weekend is nice for me, because this occasion i am reading this impressive informative post here at my home.
Great article! We will be linking to this great article on our site. Keep up the good writing.
Please let me know if you’re looking for a article author for your site. You have some really great posts and I think I would be a good asset. If you ever want to take some of the load off, I’d really like to write some articles for your blog in exchange for a link back to mine. Please blast me an e-mail if interested. Cheers!
I like the valuable information you supply in your articles. I will bookmark your weblog and check again here frequently. I am relatively certain I will be told plenty of new stuff right here! Good luck for the following!
You really make it seem so easy with your presentation but I find this topic to be really something which I think I would never understand. It seems too complicated and very broad for me. I am looking forward for your next post, I will try to get the hang of it!
I was pretty pleased to discover this great site. I wanted to thank you for your time for this wonderful read!! I definitely liked every little bit of it and I have you saved as a favorite to check out new stuff on your web site.
I think this is one of the most important information for me. And i’m glad reading your article. But want to remark on few general things, The website style is great, the articles is really excellent : D. Good job, cheers
Greetings! I know this is kinda off topic but I was wondering which blog platform are you using for this site? I’m getting tired of WordPress because I’ve had issues with hackers and I’m looking at options for another platform. I would be great if you could point me in the direction of a good platform.
Please let me know if you’re looking for a article author for your weblog. You have some really great posts and I think I would be a good asset. If you ever want to take some of the load off, I’d really like to write some articles for your blog in exchange for a link back to mine. Please send me an e-mail if interested. Thank you!
It’s a shame you don’t have a donate button! I’d most certainly donate to this fantastic blog! I suppose for now i’ll settle for book-marking and adding your RSS feed to my Google account. I look forward to fresh updates and will talk about this site with my Facebook group. Chat soon!
There is definately a lot to learn about this subject. I love all the points you’ve made.
Normally I do not read article on blogs, however I wish to say that this write-up very pressured me to take a look at and do so! Your writing taste has been amazed me. Thank you, quite great article.
hey there and thank you for your information I’ve definitely picked up anything new from right here. I did however expertise some technical issues using this site, since I experienced to reload the web site many times previous to I could get it to load properly. I had been wondering if your hosting is OK? Not that I am complaining, but sluggish loading instances times will often affect your placement in google and can damage your quality score if advertising and marketing with Adwords. Anyway I’m adding this RSS to my e-mail and can look out for a lot more of your respective interesting content. Make sure you update this again soon.
Hello there, just became aware of your blog through Google, and found that it is really informative. I’m gonna watch out for brussels. I will appreciate if you continue this in future. A lot of people will be benefited from your writing. Cheers!
I always used to read post in news papers but now as I am a user of internet so from now I am using net for posts, thanks to web.
Hi, this weekend is pleasant designed for me, because this occasion i am reading this great informative article here at my house.
Wow that was strange. I just wrote an really long comment but after I clicked submit my comment didn’t show up. Grrrr… well I’m not writing all that over again. Anyway, just wanted to say great blog!
Great goods from you, man. I’ve understand your stuff previous to and you’re just too great. I really like what you’ve acquired here, really like what you’re stating and the way in which you say it. You make it entertaining and you still take care of to keep it sensible. I cant wait to read far more from you. This is actually a wonderful website.
Having read this I thought it was extremely informative. I appreciate you finding the time and effort to put this informative article together. I once again find myself spending way too much time both reading and leaving comments. But so what, it was still worth it!
Keep on working, great job!
Hi, I do believe this is an excellent website. I stumbledupon it 😉 I’m going to come back once again since I book marked it. Money and freedom is the best way to change, may you be rich and continue to help other people.
I love reading a post that will make people think. Also, thanks for allowing me to comment!
Today, I went to the beach with my kids. I found a sea shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She put the shell to her ear and screamed. There was a hermit crab inside and it pinched her ear. She never wants to go back! LoL I know this is entirely off topic but I had to tell someone!
Very nice article. I certainly love this website. Keep it up!
Incredible points. Solid arguments. Keep up the good work.
Hello would you mind letting me know which webhost you’re working with? I’ve loaded your blog in 3 completely different internet browsers and I must say this blog loads a lot quicker then most. Can you suggest a good internet hosting provider at a honest price? Thanks a lot, I appreciate it!
Fantastic goods from you, man. I’ve understand your stuff previous to and you’re just too magnificent. I really like what you’ve acquired here, really like what you’re stating and the way in which you say it. You make it entertaining and you still take care of to keep it sensible. I can not wait to read far more from you. This is actually a wonderful website.
When someone writes an post he/she maintains the thought of a user in his/her mind that how a user can understand it. Thus that’s why this post is amazing. Thanks!
I’d like to thank you for the efforts you have put in writing this website. I’m hoping to view the same high-grade blog posts from you in the future as well. In fact, your creative writing abilities has inspired me to get my own website now 😉
I visited multiple sites but the audio quality for audio songs current at this site is in fact marvelous.
I am extremely impressed with your writing skills and also with the layout on your blog. Is this a paid theme or did you customize it yourself? Either way keep up the nice quality writing, it’s rare to see a nice blog like this one nowadays.
Ahaa, its pleasant discussion regarding this piece of writing here at this website, I have read all that, so now me also commenting here.
Hey I know this is off topic but I was wondering if you knew of any widgets I could add to my blog that automatically tweet my newest twitter updates. I’ve been looking for a plug-in like this for quite some time and was hoping maybe you would have some experience with something like this. Please let me know if you run into anything. I truly enjoy reading your blog and I look forward to your new updates.
Saved as a favorite, I like your site!
You really make it seem so easy with your presentation however I find this topic to be really something which I think I might never understand. It sort of feels too complicated and very large for me. I am looking forward in your next publish, I will try to get the cling of it!
I’d like to find out more? I’d like to find out more details.
Greetings from Los angeles! I’m bored to death at work so I decided to check out your site on my iphone during lunch break. I enjoy the knowledge you present here and can’t wait to take a look when I get home. I’m shocked at how quick your blog loaded on my mobile .. I’m not even using WIFI, just 3G .. Anyhow, wonderful site!
I blog frequently and I really appreciate your content. The article has really peaked my interest. I will book mark your website and keep checking for new information about once a week. I subscribed to your RSS feed as well.
What’s up it’s me, I am also visiting this site regularly, this website is in fact pleasant and the viewers are actually sharing nice thoughts.
Thank you for the auspicious writeup. It in fact was a amusement account it. Look advanced to far added agreeable from you! By the way, how can we communicate?
Hi there! Do you use Twitter? I’d like to follow you if that would be ok. I’m undoubtedly enjoying your blog and look forward to new updates.
Nice post. I used to be checking continuously this blog and I am inspired! Very useful information particularly the remaining phase 🙂 I care for such info a lot. I used to be seeking this particular info for a long timelong time. Thank you and good luck.
Link exchange is nothing else except it is simply placing the other person’s webpage link on your page at proper place and other person will also do same in favor of you.
I visited multiple websites but the audio quality for audio songs present at this site is in fact wonderful.
Hi, i think that i saw you visited my blog so i came to return the favor.I am trying to find things to improve my site!I suppose its ok to use some of your ideas!!
Hello! I’ve been following your website for a while now and finally got the bravery to go ahead and give you a shout out from Austin Tx! Just wanted to tell you keep up the great job!
After looking at a number of the blog posts on your website, I truly like your way of blogging. I saved it to my bookmark site list and will be checking back soon. Please check out my web site as well and let me know how you feel.
For most up-to-date news you have to go to see world wide web and on internet I found this site as a most excellent web site for newest updates.
Magnificent beat ! I wish to apprentice while you amend your web site, how can i subscribe for a blog web site? The account aided me a acceptable deal. I had been tiny bit acquainted of this your broadcast provided bright clear concept
hi!,I really like your writing so much! proportion we keep up a correspondence more approximately your post on AOL? I need an expert in this space to unravel my problem. May be that is you! Taking a look forward to peer you.
Spot on with this write-up, I really believe this web site needs far more attention. I’ll probably be back again to read more, thanks for the information!
Hi, its pleasant piece of writing about media print, we all know media is a wonderful source of information.
Hi, i read your blog occasionally and i own a similar one and i was just wondering if you get a lot of spam responses? If so how do you prevent it, any plugin or anything you can suggest? I get so much lately it’s driving me insane so any help is very much appreciated.
Thank you for the auspicious writeup. It in fact was a amusement account it. Look advanced to far added agreeable from you! By the way, how can we communicate?
Hi! I just want to give you a huge thumbs up for the great info you’ve got here on this post. I’ll be coming back to your blog for more soon.
This design is wicked! You certainly know how to keep a reader entertained. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Fantastic job. I really enjoyed what you had to say, and more than that, how you presented it. Too cool!
What’s up friends, how is everything, and what you desire to say about this article, in my view its actually awesome for me.
You made some decent points there. I looked on the web to learn more about the issue and found most individuals will go along with your views on this website.
Howdy are using WordPress for your blog platform? I’m new to the blog world but I’m trying to get started and create my own. Do you need any coding knowledge to make your own blog? Any help would be greatly appreciated!
Hey very nice website!! Guy .. Beautiful .. Amazing .. I will bookmark your web site and take the feeds also? I am glad to find numerous useful information here in the post, we need develop more strategies in this regard, thank you for sharing. . . . . .
Asking questions are truly pleasant thing if you are not understanding anything completely, but this piece of writing offers nice understanding even.
Asking questions are really pleasant thing if you are not understanding anything fully, except this post offers pleasant understanding even.
I like it when folks come together and share views. Great blog, continue the good work!
I think what you postedwrotesaidbelieve what you postedtypedbelieve what you postedtypedsaidthink what you postedtypedWhat you postedwrote was very logicala ton of sense. But, what about this?think about this, what if you were to write a killer headlinetitle?content?typed a catchier title? I ain’t saying your content isn’t good.ain’t saying your content isn’t gooddon’t want to tell you how to run your blog, but what if you added a titlesomethingheadlinetitle that grabbed a person’s attention?maybe get people’s attention?want more? I mean %BLOG_TITLE% is a little plain. You might look at Yahoo’s home page and watch how they createwrite post headlines to get viewers interested. You might add a related video or a related pic or two to get readers interested about what you’ve written. Just my opinion, it might bring your postsblog a little livelier.
Hey There. I found your blog the use of msn. This is an extremely smartly written article. I will be sure to bookmark it and come back to read more of your useful information. Thank you for the post. I will definitely comeback.
This design is steller! You certainly know how to keep a reader entertained. Between your wit and your videos, I was almost moved to start my own blog (well, almost…HaHa!) Wonderful job. I really enjoyed what you had to say, and more than that, how you presented it. Too cool!
Hi to all, because I am truly keen of reading this webpage’s post to be updated regularly. It contains nice information.
Saved as a favorite, I really like your site!
Hello! Do you know if they make any plugins to protect against hackers? I’m kinda paranoid about losing everything I’ve worked hard on. Any recommendations?
What’s uр Dear, aгe you in fact visiting this web site daily, if
so after that you will absolutely take nice know-how.
Hi to all, how is everything, I think every one is getting more from this website, and your views are pleasant in favor of new users.
This information is invaluable. How can I find out more?
You really makе it seem so easy with your prеsentation but I find this
toрic to be really something which I think I ᴡouⅼd never understand.
It seems too complicated and extremely broad for me.
I am looking forward for your next p᧐st, I’ll try to
get the hang of it!
My brother suggested I might like this website. He was totally right. This post actually made my day. You cann’t imagine just how much time I had spent for this information! Thanks!
This is very interesting, You are a very skilled blogger. I have joined your feed and look forward to seeking more of your great post. Also, I have shared your web site in my social networks!
I ⅾо believe all the ideas you have offered in your post.
They’re very convіncing and can defіnitely work. Nonethеless, the posts are toо quick foг novices.
May yoս please lengthen tһеm a little from sᥙbsequent time?
Thanks for the post.
Greetings! Very helpful advice within this article! It is the little changes that make the biggest changes. Thanks for sharing!
I’m tгuly enjoying the design and layout of youг website.
It’s a vеry easy оn the eyeѕ which makes it much more ρleasаnt for me tߋ come
here and visit more often. Diɗ ʏou hire out a developer to cгeate your theme?
Outstanding work!
Hi, i feel that i saw you visited my blog so i got here to go back the choose?.I am trying to find things to improve my site!I assume its ok to use some of your ideas!!
I needed to thank you for this fantastic read!! I definitely enjoyed every little bit of it. I have you bookmarked to check out new stuff you post
Ищете надежного подрядчика для устройства стяжки пола в Москве? Обратитесь к нам на сайт styazhka-pola24.ru! Мы предлагаем услуги по залитию стяжки пола любой сложности и площади, а также гарантируем высокое качество работ.
снабжение объектов строительства
Попробуйте механизированную штукатурку от mehanizirovannaya-shtukaturka-moscow.ru и убедитесь в ее эффективности. Ваш дом заслуживает лучшего!
It’s not my first time to visit this web site, i am visiting this web site dailly and get pleasant information from here daily.
You can definitely see your enthusiasm in the article you write. The arena hopes for more passionate writers like you who aren’t afraid to mention how they believe. Always go after your heart.
When someone writes an article he/she keeps the plan of a user in his/her mind that how a user can know it. So that’s why this article is great. Thanks!
Попробуйте механизированную штукатурку от mehanizirovannaya-shtukaturka-moscow.ru и убедитесь в ее эффективности. Ваш дом заслуживает лучшего!
I am truly thankful to the owner of this web site who has shared this wonderful post at here.
Nice post. I used to be checking continuously this blog and I am inspired! Very useful information specially the ultimate phase 🙂 I maintain such info a lot. I used to be seeking this particular info for a long timelong time. Thank you and good luck.
This web site really has all of the information I wanted about this subject and didn’t know who to ask.
Yesterday, while I was at work, my sister stole my iPad and tested to see if it can survive a forty foot drop, just so she can be a youtube sensation. My iPad is now broken and she has 83 views. I know this is entirely off topic but I had to share it with someone!
They report that their sons are uncomfortable in certain social situations, such as a class pool party or summer camp swim lessons, at the beach or at gym class at school and never take their shirt off cialis buy online usa The complexity is further enhanced by the fact that the peptides are also found in the bloodstream, making it difficult to decipher whether the effects are local or systemic
Hі, i feeⅼ that і saw yοu visited my weblog thus i got here to return the favor?.I’m trying tо in finding things to improve my website!I
assume its adequate to use some of your ideas!!
Hello everybody, here еvery one is sharing such familiaritʏ, therеfore it’s nice to read this website, and I used to
go to see this bⅼog everydаy.
Hеy thеre terrific blog! Doeѕ running a bⅼog similar to this require a great deal of
work? Ι havе ɑbsolᥙtely no knowledge of computer programming but I had been hoping to start my own blog soon. Anyԝay, should you have any ideas or tips for
new blog owners please share. I understand this is
off topic nevertheless I simply had to ɑsk.
Many thanks!
Veгy shortly this website will be famous amid all
blogging and site-building visitors, due tο it’s good
artіcles or revіews
Hello! I know this is somewhat off topic but I was wondering which blog platform are you using for this site? I’m getting fed up of WordPress because I’ve had issues with hackers and I’m looking at options for another platform. I would be awesome if you could point me in the direction of a good platform.
Hi to all, the contents present at this website are in fact remarkable for people experience, well, keep up the nice work fellows.
Скоростроительные здания: экономический доход в каждом элементе!
В сегодняшнем обществе, где время – деньги, экспресс-конструкции стали настоящим выходом для предпринимательства. Эти современные объекты объединяют в себе высокую прочность, экономическую эффективность и мгновенную сборку, что придает им способность первоклассным вариантом для разнообразных коммерческих задач.
[url=https://bystrovozvodimye-zdanija-moskva.ru/]Строительство каркасных зданий из металлоконструкций[/url]
1. Высокая скорость возвода: Время – это самый важный ресурс в бизнесе, и здания с высокой скоростью строительства позволяют существенно сократить сроки строительства. Это особенно ценно в ситуациях, когда важно быстро начать вести бизнес и начать получать прибыль.
2. Финансовая эффективность: За счет совершенствования производственных операций по изготовлению элементов и монтажу на площадке, цена скоростроительных зданий часто остается меньше, по сравнению с обычными строительными задачами. Это позволяет получить большую финансовую выгоду и достичь большей доходности инвестиций.
Подробнее на [url=https://bystrovozvodimye-zdanija-moskva.ru/]https://www.scholding.ru/[/url]
В заключение, скоро возводимые строения – это идеальное решение для проектов любого масштаба. Они сочетают в себе эффективное строительство, финансовую эффективность и устойчивость, что придает им способность оптимальным решением для деловых лиц, желающих быстро начать вести бизнес и получать прибыль. Не упустите шанс экономии времени и денег, идеальные сооружения быстрого монтажа для вашего следующего проекта!
Remarkable things here. I’m very glad to peer your article. Thank you so much and I’m taking a look forward to touch you. Will you please drop me a mail?
Pretty nice post. I just stumbled upon your blog and wanted to say that I have really enjoyed browsing your blog posts. In any case I’ll be subscribing to your feed and I hope you write again soon!
Быстромонтажные здания: финансовая выгода в каждой составляющей!
В современном мире, где время – деньги, объекты быстрого возвода стали решением, спасающим для коммерции. Эти новейшие строения включают в себя высокую надежность, финансовую выгоду и быстрый монтаж, что обуславливает их превосходным выбором для разных коммерческих начинаний.
[url=https://bystrovozvodimye-zdanija-moskva.ru/]Быстровозводимые здания[/url]
1. Срочное строительство: Минуты – важнейший фактор в деловой сфере, и скоростроительные конструкции позволяют существенно сократить сроки строительства. Это высоко оценивается в вариантах, когда важно быстро начать вести бизнес и начать монетизацию.
2. Бюджетность: За счет усовершенствования производственных процессов элементов и сборки на месте, финансовые издержки на быстровозводимые объекты часто уменьшается, по отношению к традиционным строительным проектам. Это предоставляет шанс сократить издержки и достичь более высокой инвестиционной доходности.
Подробнее на [url=https://bystrovozvodimye-zdanija-moskva.ru/]scholding.ru/[/url]
В заключение, экспресс-конструкции – это отличное решение для предпринимательских задач. Они обладают эффективное строительство, экономию средств и надежные характеристики, что позволяет им отличным выбором для предпринимателей, ориентированных на оперативный бизнес-старт и получать доход. Не упустите момент экономии времени и средств, идеальные сооружения быстрого монтажа для вашего предстоящего предприятия!
Wߋw, this post is good, my sister is analyzing these things, therefore I am going to inform һer.
Does your site haѵe a contact page? I’m having pгobⅼems locating
it but, I’d like to shoߋt you an e-mail.
I’ve got some suggestions for your blog you might be interested in hearing.
Either way, greɑt site and I look forward to sеeing it
expand over time.
Wow, awesome blog layout! How long have you been blogging for? you make blogging look easy. The overall look of your site is great, let alone the content!
of course like your website however you need to check the spelling on quite a few of your posts. Several of them are rife with spelling problems and I in finding it very bothersome to tell the truth then again I will surely come back again.
Wow that was odd. I just wrote an very long comment but after I clicked submit my comment didn’t show up. Grrrr… well I’m not writing all that over again. Anyway, just wanted to say superb blog!
Possibly the most important marketing step of all, getting your home listed on the MLS is one of the perks of working with a real estate agent. That said, you can still get listed on the MLS when selling your home yourself, you’ll just need to go through a website that can facilitate that, or pay an agent a fixed fee to place the listing for you. For more details about this, see the next section titled “How To Post For Sale By Owner On MLS?”. There is a small segment of sellers who don’t have the budget necessary to do even the little things you can do to help sell your house. If you’re such a homeowner, selling your house to a cash buyer may be a good idea. Many iBuyers and home-buying companies can purchase your home at market value and provide a full offer in cash for your house as-is.
https://beaukhsc222391.blogsidea.com/29522247/how-to-survive-a-complete-kitchen-remodel
The average rent by year in Alabama increases at a rate on par with the national average rent inflation rate. Meanwhile, the New Jersey Department of Community Affairs (DCA) is reminding residents that it will be accepting pre-applications online for the State Rental Assistance Program (SRAP) waiting list, starting Monday, July 11 through Friday, July 22. The Equifax logo is a registered trademark owned by Equifax in the United States and other countries. Much like conventional apartment rents, student housing pricing varies widely across the U.S. The average price of a student housing bed runs higher in states with steeper conventional apartment prices, such as in the Northeast and West, and lower in the South and Southeast. Originally from Houston, Texas, Alexandra is currently getting her Master’s in Public Health with a health policy certificate at Columbia University. One of her life goals is to own her own art gallery!
Its like you read my mind! You seem to understand so much approximately this, like you wrote the e-book in it or something. I think that you simply could do with some % to pressure the message house a bit, however other than that, this is fantastic blog. An excellent read. I’ll definitely be back.
Моментально возводимые здания: коммерческая выгода в каждой составляющей!
В современном обществе, где часы – финансовые ресурсы, здания с высокой скоростью строительства стали решением, спасающим для коммерческой деятельности. Эти современные объекты обладают повышенную прочность, эффективное расходование средств и мгновенную сборку, что позволяет им лучшим выбором для различных бизнес-проектов.
[url=https://bystrovozvodimye-zdanija-moskva.ru/]Быстровозводимые здания[/url]
1. Высокая скорость возвода: Минуты – основной фактор в коммерческой деятельности, и скоро возводимые строения обеспечивают существенное уменьшение сроков стройки. Это чрезвычайно полезно в условиях, когда актуально быстро начать вести дело и начать монетизацию.
2. Экономичность: За счет совершенствования производственных процессов элементов и сборки на площадке, бюджет на сооружения быстрого монтажа часто бывает ниже, по отношению к традиционным строительным проектам. Это дает возможность сэкономить деньги и получить лучшую инвестиционную отдачу.
Подробнее на [url=https://bystrovozvodimye-zdanija-moskva.ru/]scholding.ru[/url]
В заключение, сооружения быстрого монтажа – это великолепное решение для коммерческих проектов. Они сочетают в себе эффективное строительство, экономию средств и устойчивость, что дает им возможность первоклассным вариантом для профессионалов, готовых к мгновенному началу бизнеса и извлекать прибыль. Не упустите возможность сэкономить время и средства, выбрав быстровозводимые здания для ваших будущих проектов!
Nice post. I learn something new and challenging on blogs I stumbleupon every day. It will always be helpful to read content from other writers and practice a little something from their sites.
Скоростроительные здания: финансовая выгода в каждой части!
В сегодняшнем обществе, где секунды – доллары, объекты быстрого возвода стали настоящим выходом для предпринимательства. Эти новейшие строения сочетают в себе устойчивость, финансовую эффективность и быстрый монтаж, что обуславливает их отличным выбором для разных коммерческих начинаний.
[url=https://bystrovozvodimye-zdanija-moskva.ru/]Построить быстровозводимое здание[/url]
1. Быстрота монтажа: Минуты – основной фактор в предпринимательстве, и сооружения моментального монтажа позволяют существенно уменьшить временные рамки строительства. Это преимущественно важно в моменты, когда срочно требуется начать бизнес и начать получать прибыль.
2. Экономичность: За счет оптимизации процессов производства элементов и сборки на месте, расходы на скоростройки часто бывает менее, по сравнению с традиционными строительными проектами. Это дает возможность сэкономить деньги и обеспечить более высокий доход с инвестиций.
Подробнее на [url=https://bystrovozvodimye-zdanija-moskva.ru/]www.scholding.ru[/url]
В заключение, скоростроительные сооружения – это лучшее решение для бизнес-мероприятий. Они объединяют в себе быстроту возведения, экономичность и повышенную надежность, что делает их оптимальным решением для предпринимателей, имеющих целью быстрый бизнес-старт и обеспечивать доход. Не упустите шанс экономии времени и денег, выбрав быстровозводимые здания для ваших будущих проектов!
I visited many web pages but the audio quality for audio songs present at this site is actually marvelous.
This is very interesting, You are an overly professional blogger. I have joined your feed and look forward to in search of more of your magnificent post. Also, I have shared your site in my social networks
Hi there, this weekend is nice designed for me, since this occasion i am reading this enormous informative post here at my house.
Ощутите волнение от высоких полетов с лаки джет официальный сайт! Присоединяйтесь к тем, кто уже выбрал этот путь к удаче через 1win.
I’m not sure why but this website is loading extremely slow for me. Is anyone else having this issue or is it a problem on my end? I’ll check back later and see if the problem still exists.
Hеllo, I enjoy reading all of your article post.
I wanted to write ɑ littlе comment to support yߋu.
Забота о домашнем пространстве – это забота о приятности. Термомодернизация фасадов – это не только изысканный облик, но и обеспечение сохранения тепла в вашем уединенном уголке. Профессионалы, коллектив экспертов, предлагаем вам сделать ваш дом в прекрасное место для жизни.
Наши проекты – это не просто утепление, это творческий подход к каждому деталю. Мы стремимся к гармонии между красотой и практичностью, чтобы ваше жилище превратилось не только теплым, но и прекрасным.
И самое важное – доступные расценки! Мы верим, что качественные услуги не должны быть сверхдорогими. [url=https://ppu-prof.ru/]Ремонт домов утепление фасадов[/url] начинается всего от 1250 рублей за кв. метр.
Инновационные технологии и материалы высокого стандарта позволяют нам создавать теплоизоляцию, долговечную и надежную. Забудьте о холодных стенах и дополнительных расходах на отопление – наше утепление станет вашим надежным барьером от холода.
Подробнее на [url=https://ppu-prof.ru/]www.ppu-prof.ru[/url]
Не откладывайте на потом заботу о радости жизни в вашем жилье. Обращайтесь к профессионалам, и ваш дом станет настоящим художественным произведением, которое принесет вам не только тепло. Вместе мы создадим обители, где вам будет по-настоящему комфортно!
I really like and appreciate your blog.Really thank you! Cool.
Good day! Woᥙld you mind if I share уour blog
witһ my twitter group? There’s a lot of people that I think would rеally enjoy your content.
Pleɑsе let me knoᴡ. Thank you
CGMiner ist eines der ersten Bitcoin-Schürfprogramme auf dem Markt. Es ist ein Open-Source-Mining-Tool, das mit einer Vielzahl von Betriebssystemen und Mining-Hardware-Setups funktioniert. Da es sich um eine Open-Source-Software handelt, kannst du sie nach Belieben verändern und es gibt keine lizenzbedingten Nutzungsbeschränkungen. Darüber hinaus verfügt TurboMiner – BTC Cloud Mining über ein Wallet-System, mit dem Sie Ihr Geld abheben können – wenn auch nicht einfach. Es sucht nach vielen Anforderungen, bevor Sie auszahlen können. Im Gegensatz zu Binance: Bitcoin Marketplace Crypto Wallet und MetaMask bietet diese App keine Option zum Handeln. Trotz der potenziellen Risiken kann eine Investition in TurboMiner – BTC Cloud Mining für Anfänger vorteilhaft sein. Die App bietet kostenloses Mining und ist relativ einfach zu bedienen. Wenn Sie jedoch das Bitcoin-Mining auf die nächste Stufe bringen möchten, müssen Sie bei Ihren Entscheidungen Vorsicht walten lassen. Ein weiterer Faktor, der berücksichtigt werden sollte, ist, dass die App keine Auszahlung Ihrer Einnahmen zu jeder Zeit zulässt.
https://www.vanilla.in.th/member.cgi?mid=1701334414
Ob der Hype auch darüber hinaus anhält, hängt insbesondere vom Ethereum-Kurs ab. Fällt dieser stark, was jederzeit passieren kann, fahren die Krypto-Miner ihre Operationen zurück und fluten den Markt mit gebrauchten Grafikkarten. Steigt er jedoch weiter, bleiben AMD-Grafikkarten die nachgefragteste Hardware der Tech-Welt. Die Chancen dafür stehen gut: Allein im August stieg der Ethereum-Eurokurs um 60 Prozent an. Welche Kryptowährungen es neben Ethereum und Bitcoin gibt, zeigen wir euch in unserer Galerie: Von Alexander Schmid *) Bei Proof-of-Work-Blockchains (bspw. Bitcoin sowie Ethereum vor „The Merge“) gewinnt dabei der Schnellste und Stärkste diesen Wettbewerb, d.h. der Miner mit der größten Rechenleistung, was zu hohem Energieverbrauch führt. Der Nebras Hotspot Miner (HNT) ist der weltweit erste heliumbetriebene, hochfrequenzfähige Miner, der wesentlich weniger Energie verbraucht als herkömmliche Miner auf Siliziumbasis. Infolgedessen ist die Rentabilität gestiegen und es ist eine umweltfreundlichere Mining-Lösung entstanden.
Do you have a spam issue on this site; I also am a blogger, and I was curious about your situation; many of us have created some nice procedures and we are looking to trade strategies with other folks, why not shoot me an e-mail if interested.
If you want to increase your familiarity only keep visiting this site and be updated with the latest gossip posted here.
What’s up friends, how is all, and what you wish for to say regarding this article, in my view its really awesome designed for me.
Great delivery. Solid arguments. Keep up the good effort.
Very good post.Really looking forward to read more. Great.
My website: порно студенток
It is appropriate time to make some plans for the future and it is time to be happy. I have read this post and if I could I want to suggest you few interesting things or advice. Perhaps you could write next articles referring to this article. I wish to read more things about it!
Currently it looks like BlogEngine is the top blogging platform out there right now. (from what I’ve read) Is that what you’re using on your blog?
Very good post.Really looking forward to read more. Great.
My website: порно пьяные
Hello there! This post couldn’t be written any better! Reading this post reminds me of my good old room mate! He always kept talking about this. I will forward this post to him. Pretty sure he will have a good read. Thanks for sharing!
Hi friends, pleasant article and good arguments commented here, I am really enjoying by these.
I got what you intend,bookmarked, very decent website.
My website: онлайн порно
My partner and I absolutely love your blog and find a lot of your post’s to be just what I’m looking for. Do you offer guest writers to write content available for you? I wouldn’t mind publishing a post or elaborating on some of the subjects you write about here. Again, awesome blog!
Your method of describing all in this post is really pleasant, all be able to easily understand it, Thanks a lot.
Thanks for sharing your thoughts on %meta_keyword%. Regards
always i used to read smaller articles which also clear their motive, and that is also happening with this piece of writing which I am reading at this place.
Excellent blog here! Also your site loads up fast! What host are you using? Can I get your affiliate link to your host? I wish my site loaded up as fast as yours lol
Hey! Do you know if they make any plugins to protect against hackers? I’m kinda paranoid about losing everything I’ve worked hard on. Any recommendations?
I always spent my half an hour to read this weblog’s articles or reviews every day along with a cup of coffee.
As the admin of this website is working, no uncertainty very soon it will be famous, due to its quality contents.
My relatives always say that I am wasting my time here at net, but I know I am getting familiarity everyday by reading such pleasant articles or reviews.
My coder is trying to persuade me to move to .net from PHP. I have always disliked the idea because of the expenses. But he’s tryiong none the less. I’ve been using Movable-type on a variety of websites for about a year and am worried about switching to another platform. I have heard great things about blogengine.net. Is there a way I can transfer all my wordpress content into it? Any kind of help would be really appreciated!
Appreciating the hard work you put into your site and in depth information you provide. It’s awesome to come across a blog every once in a while that isn’t the same unwanted rehashed material. Fantastic read! I’ve saved your site and I’m including your RSS feeds to my Google account.
Thank you for the auspicious writeup. It in fact was a amusement account it. Look advanced to far added agreeable from you! By the way, how can we communicate?
When I originally commented I seem to have clicked the -Notify me when new comments are added- checkbox and now every time a comment is added I get four emails with the same comment. Is there a means you can remove me from that service? Thank you!
Hello there, simply was aware of your blog through Google, and found that it is really informative. I’m gonna watch out for brussels. I will appreciate when you continue this in future. Lots of other people will be benefited from your writing. Cheers!
wonderful issues altogether, you just gained a emblem new reader. What might you suggest in regards to your post that you made a few days ago? Any sure?
A lot of blog writers nowadays yet just a few have blog posts worth spending time on reviewing.
My website: секс смотреть бесплатно на русском
Hey there, You have done a fantastic job. I will definitely digg it and personally recommend to my friends. I am sure they will be benefited from this site.
Can I simply say what a relief to discover a person that really knows what they’re talking about online. You definitely understand how to bring an issue to light and make it important. More people have to look at this and understand this side of the story. It’s surprising you aren’t more popular since you surely have the gift.
Hi there, i read your blog occasionally and i own a similar one and i was just wondering if you get a lot of spam feedback? If so how do you reduce it, any plugin or anything you can advise? I get so much lately it’s driving me insane so any help is very much appreciated.
Remarkable! Its really awesome piece of writing, I have got much clear idea concerning from this piece of writing.
Appreciation to my father who told me concerning this website, this website is really awesome.
I gotta favorite this site it seems very beneficial handy
My website: порномассаж
An impressive share! I have just forwarded this onto a colleague who was doing a little research on this. And he in fact bought me breakfast because I discovered it for him… lol. So let me reword this…. Thank YOU for the meal!! But yeah, thanx for spending time to discuss this matter here on your site.
Major thanks for the article post. Much thanks again.
My website: смотреть порно русское
It is appropriate time to make a few plans for the future and it is time to be happy. I have read this post and if I may just I wish to suggest you few interesting things or advice. Perhaps you could write next articles referring to this article. I wish to read more things approximately it!
Saved as a favorite, I like your web site!
Good article! We will be linking to this great article on our site. Keep up the good writing.
Pretty section of content. I just stumbled upon your web site and in accession capital to assert that I acquire in fact enjoyed account your blog posts. Any way I’ll be subscribing to your augment and even I achievement you access consistently fast.
My website: русское порно видео смотреть бесплатно
Pretty part of content. I simply stumbled upon your web site and in accession capital to say that I acquire in fact enjoyed account your blog posts. Any way I’ll be subscribing on your augment or even I fulfillment you access persistently fast.
As a Newbie, I am continuously exploring online for articles that can be of assistance to me.
My website: порно русское массаж
Thank you for the auspicious writeup. It in fact was a amusement account it. Look advanced to far added agreeable from you! By the way, how can we communicate?
Asking questions are in fact pleasant thing if you are not understanding anything fully, but this post gives pleasant understanding even.
I have read so many articles or reviews regarding the blogger lovers but this piece of writing is truly a good article, keep it up.
Yesterday, while I was at work, my sister stole my iPad and tested to see if it can survive a 40 foot drop, just so she can be a youtube sensation. My iPad is now broken and she has 83 views. I know this is completely off topic but I had to share it with someone!
Hey There. I found your blog the use of msn. This is an extremely well written article. I will be sure to bookmark it and come back to read more of your useful information. Thank you for the post. I will definitely comeback.
Having read this I thought it was really informative. I appreciate you taking the time and effort to put this information together. I once again find myself spending way too much time both reading and commenting. But so what, it was still worth it!
Incredible quest there. What occurred after? Thanks!
Your method of describing everything in this piece of writing is really nice, all be able to effortlessly know it, Thanks a lot.
My brotһer suggested I might like this website. He used to be entirely right.
This post aсtually made my day. Y᧐u can not consider simply how so much time
I had spent for this information! Thanks!
I reckon something truly special in this website.
My website: учителя порно
A round of applause for your article. Much thanks again.
My website: ебут пьяную
A round of applause for your article. Much thanks again.
My website: секс бесплатный секс русский
Very good post.Really looking forward to read more. Great.
My website: порно учитель русский
As a Newbie, I am continuously exploring online for articles that can be of assistance to me.
My website: секс со шлюхой
I got what you intend,bookmarked, very decent website.
My website: анальный оргазм жены
Wohh precisely what I was searching for, regards for putting up.
My website: лижет жопу бабе
Rainbow Riches casino was made specifically for Rainbow Riches slot series fans, so it didn’t surprise us when we found that the online casino offers a smaller game collection compared to other relatively new online casinos. One of the UK’s most-loved online slots, Rainbow Riches is a mainstay of the UK’s biggest online casino operators. Usually available with generous bonuses and promotions, let’s take a look at the best online casinos to play Rainbow Riches in the UK. If you use the Rainbow Riches Casino iOS app, you’ll be pleased to know that you can conveniently deposit and withdraw funds using the secure Apple Pay payment system. With Apple Pay, the minimum deposit and withdrawal amount is set at £10, ensuring flexibility for players. However, it’s important to note that the maximum withdrawal limit per transaction is £5,000. Keep in mind that when utilising Apple Pay for withdrawals, it may take up to one working day for the funds to fully clear and be available in your designated account.
https://zionuana986498.blogs-service.com/54613314/best-live-roulette-casinos
The company, which started its work with the creation of slots for land-based casinos, should have other examples of casino games. This company is, of course, Novomatic and we would like to say that the Novomatic list of online casino games really exists. If you are at CasinoHEX Canada and read this article, then you want to know more about these types of Novomatic products and we are ready to help you. PariMatch Casino is among the leading casinos in the list of Novomatic casinos as well as one of our best casinos, as it offers the widest range of Novomatic slots as well as the best optimization for them. You can play these and many other titles from the Austrian developer in any Novomatic online casino. Free play Novomatic slots should be your starting point – it’s best to try the goods before you buy them. You can find top slot sites with Novamatic software on our list compiled by a team of experts.
I got what you intend,bookmarked, very decent website.
My website: порно на пляже
Definitely, what a great blog and revealing posts, I definitely will bookmark your site. Best Regards!
My website: мамочка хочет секса
A round of applause for your article. Much thanks again.
My website: порно кастинг жесткое
Ponto IPTV a melhor programacao de canais IPTV do Brasil, filmes, series, futebol
My website: порно кончают толпой
Respect to post author, some fantastic information
My website: порно онлайн бдсм
The 7-day moving average of the average transaction fee on Bitcoin has surpassed that on Ethereum since Nov. 9, Stevens noted, adding that the gap is now much wider than when they briefly flipped in early October. As mempool volume increases, Bitcoin challenges Ethereum in transaction fee totals. Always keep in mind that gas charges, network and trade fees will be included in the total cost of the transaction. The actual fee you have to pay varies and depends on the network If you are afraid that the mempool might feel when you expect it the least and your transaction may lose priority, then you can also choose to use the “Replace-By-Fee” (RBF) option. This means that you can bump the fee after your transaction gets broadcast and registered in the mempool, so that it becomes a priority for miners.
http://uniform-wiki.win/index.php?title=Comp_crypto_news
All rights reserved © 2021 CoinCheckup ECOMI’s Secure Wallet is the native cold wallet to OMI tokens, but you can also use any other crypto wallet compatible with the ERC-20 tokens such as MetaMask and Coinbase browser wallet. You can also use Ledger cold storage devices for your OMI holdings alongside the Ledger Live desktop app. ECOMI Price History The ECOMI Discord Server is officially live, and will serve as the new community hub for all things ECOMI and OMI tokens moving forward. We are incredibly excited to create this space for everyone to come together, share their knowledge, and experience all this community offers. Through the ECOMI Discord… The ECOMI Secure Wallet has always been one of the simplest ways to store and secure your OMI tokens. With the pending introduction of OMI Reward Tiers in the VeVe digital collectibles app, you may want to move some of your tokens from cold storage to begin earning additional Master…
Muchos Gracias for your article.Really thank you! Cool.
My website: лижет пизду жене
A round of applause for your article. Much thanks again.
My website: порно довел до оргазма
I think the admin of this site is actually working hard in favor of his site, because here every data is quality based stuff.
of course like your website however you need to test the spelling on quite a few of your posts. A number of them are rife with spelling problems and I in finding it very bothersome to tell the truth however I will certainly come back again.
Muchos Gracias for your article.Really thank you! Cool.
My website: смотреть бесплатно порно мать
Ηello thеre! This blog post could not be written any better!
Looking at this pоst reminds me of my previous roommatе!
He always kept talking aЬout this. I most certainly will
send this information to him. Fairly certain he will have a
good reaԁ. Thank you for sharing!
Wow that was strange. I just wrote an really long comment but after I clicked submit my comment didn’t show up. Grrrr… well I’m not writing all that over again. Regardless, just wanted to say great blog!
As a Newbie, I am always searching online for articles that can help me. Thank you
My website: порно трахает брюнетку
Terrific article! This is the type of information that are supposed to be shared around the internet. Disgrace on the seek engines for now not positioning this publish upper! Come on over and discuss with my site . Thank you =)
Why people still use to read news papers when in this technological world everything is accessible on net?
Thanks-a-mundo for the post.Really thank you! Awesome.
My website: суй глубже
I know this website offers quality based posts and other information, is there any other web site which provides these things in quality?
Hey! Do you use Twitter? I’d like to follow you if that would be ok. I’m undoubtedly enjoying your blog and look forward to new updates.
Ridiculous quest there. What occurred after? Good luck!
A lot of blog writers nowadays yet just a few have blog posts worth spending time on reviewing.
My website: супруга сосет
Hey I am so thrilled I found your webpage, I really found you by error, while I was browsing on Aol for something else, Nonetheless I am here now and would just like to say thanks a lot for a fantastic post and a all round enjoyable blog (I also love the theme/design), I dont have time to browse it all at the minute but I have saved it and also added in your RSS feeds, so when I have time I will be back to read a lot more, Please do keep up the awesome jo.
My website: Порно связанных
A round of applause for your article. Much thanks again.
My website: анальная ебля
Your method of explaining all in this article is actually pleasant, all be able to without difficulty know it, Thanks a lot.
A lot of blog writers nowadays yet just a few have blog posts worth spending time on reviewing.
My website: порно видео зрелые
A lot of blog writers nowadays yet just a few have blog posts worth spending time on reviewing.
My website: красивый анал бесплатно
I got what you intend,bookmarked, very decent website.
My website: русское порно 18
I’m extremely pleased to discover this website. I wanted to thank you for ones time just for this fantastic read!
My website: кончи мне в рот
Superb blog you have here but I was wondering if you
knew of any forums that cover the same topics talked
about here? I’d really love to be a part of online community
where I can get responses from other experienced people that
share the same interest. If you have any suggestions, please let me know.
Kudos! I saw similar here: sklep internetowy and also here:
dobry sklep
Very good post.Really looking forward to read more. Great.
My website: дрочка члена
Major thanks for the article post. Much thanks again.
My website: смотреть порно камшоты
Thank you ever so for you blog. Really looking forward to read more.
My website: смотреть порно анал
I gotta favorite this site it seems very beneficial handy
My website: жесткое порно онлайн
As a Newbie, I am always searching online for articles that can help me. Thank you
My website: секс с девушкой на улице
I reckon something truly special in this website.
My website: анилингус онлайн
Major thanks for the article post. Much thanks again.
My website: секс зрелых
canadian viagra online pharmacy see post
canada online pharmacy viagra [url=http://canadianphrmacy23.com/]canadian online pharmacies[/url]
A lot of blog writers nowadays yet just a few have blog posts worth spending time on reviewing.
My website: секс видео блондинка
This site definitely has all of the information I needed about this subject
My website: секс с блондиночкой
Wohh precisely what I was searching for, regards for putting up.
My website: секс с красивой сестрой
Definitely, what a great blog and revealing posts, I definitely will bookmark your site. Best Regards!
My website: инцест трахает сестру
Heya are using WordPress for your blog platform? I’m new to the blog world but I’m trying to get started and create my own. Do you need any coding knowledge to make your own blog? Any help would be greatly appreciated!
Hi there, after reading this remarkable post i am also happy to share my experience here with friends.
What’s up, its pleasant post about media print, we all know media is a impressive source of information.
Hi my family member! I want to say that this article is awesome, great written and come with almost all significant infos. I’d like to see more posts like this .
Wow, amazing blog format! How long have you been blogging for? you make blogging glance easy. The full glance of your site is wonderful, let alonewell as the content!
Your style is very unique compared to other people I have read stuff from. Thank you for posting when you have the opportunity, Guess I will just bookmark this page.
Nice post. I learn something new and challenging on sites I stumbleupon every day. It will always be helpful to read content from other writers and practice a little something from their websites.
Hi there would you mind stating which blog platform you’re working with? I’m planning to start my own blog in the near future but I’m having a difficult time making a decision between BlogEngine/Wordpress/B2evolution and Drupal. The reason I ask is because your design and style seems different then most blogs and I’m looking for something completely unique. P.S Apologies for getting off-topic but I had to ask!
I’m now not positive where you are getting your info, however good topic. I needs to spend a while studying more or understanding more. Thank you for great information I used to be looking for this information for my mission.
Hi there, for all time i used to check website posts here early in the break of day, since i like to gain knowledge of more and more.
This is the right site for anybody who would like to find out about this topic. You realize so much its almost hard to argue with you (not that I personally would want toHaHa). You definitely put a new spin on a topic that has been written about for a long time. Great stuff, just great!
Good day! I know this is kind of off topic but I was wondering if you knew where I could get a captcha plugin for my comment form? I’m using the same blog platform as yours and I’m having difficulty finding one? Thanks a lot!
Thank you for any other informative website. Where else may just I am getting that kind of info written in such a perfect approach? I have a undertaking that I am simply now running on, and I have been at the glance out for such information.
I used to be recommended this website via my cousin. I am now not positive whether this post is written by means of him as no one else recognise such distinct approximately my problem. You are wonderful! Thank you!
Good answer back in return of this issue with solid arguments and describing all about that.
Aviator Spribe играть по стратегии казино
It is simply matchless 🙂
Добро пожаловать в захватывающий мир авиаторов! Aviator – это увлекательная игра, которая позволит вам окунуться в атмосферу боевых действий на небе. Необычные графика и захватывающий сюжет сделают ваше путешествие по воздуху неповторимым.
Встречайте новый автомат Aviator Spribe играть бесплатно и выигрывайте крупные суммы!
Aviator игра позволит вам почувствовать себя настоящим пилотом. Вам предстоит совершить невероятные маневры, выполнять сложные задания и сражаться с противниками. Улучшайте свой самолет, чтобы быть готовым к любым ситуациям и становиться настоящим мастером.
Основные особенности Aviator краш игры:
1. Реалистичная графика и физика – благодаря передовой графике и реалистичной физике вы почувствуете себя настоящим пилотом.
2. Разнообразные режимы игры и миссии – в Aviator краш игре вы сможете выбрать различные режимы игры, такие как гонки, симулятор полетов и захватывающие воздушные бои. Кроме того, каждая миссия будет предлагать свои собственные вызовы и задачи.
3. Улучшение и модернизация самолетов – в игре доступны различные модели самолетов, которые можно покупать и улучшать. Вы сможете устанавливать новое оборудование, улучшать двигательность и мощность своего самолета, а также выбирать различные варианты окраски и декорации.
Aviator краш игра – это возможность испытать себя в роли авиатора и преодолеть все сложности и опасности воздушного пространства. Почувствуйте настоящую свободу и адреналин в Aviator краш игре онлайн!
Играйте в «Авиатор» в онлайн-казино Pin-Up
Aviator краш игра онлайн предлагает увлекательную и захватывающую игровую атмосферу, где вы становитесь настоящим авиатором и сражаетесь с самыми опасными искусственными интеллектами.
В этой игре вы должны показать свое мастерство и смекалку, чтобы преодолеть сложности многочисленных локаций и уровней. Вам предстоит собирать бонусы, уклоняться от препятствий и сражаться с врагами, используя свои навыки пилотирования и стрельбы.
Каждый уровень игры Aviator краш имеет свою уникальную атмосферу и задачи. Будьте готовы к неожиданностям, так как вас ждут захватывающие повороты сюжета и сложные испытания. Найдите все пути к победе и станьте настоящим героем авиатором!
Авиатор игра является прекрасным способом провести время и испытать настоящий адреналиновый разряд. Готовы ли вы стать лучшим авиатором? Не упустите свой шанс и начните играть в Aviator краш прямо сейчас!
Aviator – играй, сражайся, побеждай!
Aviator Pin Up (Авиатор Пин Ап ) – игра на деньги онлайн Казахстан
Aviator игра предлагает увлекательное и захватывающее разнообразие врагов и уровней, которые не оставят равнодушными даже самых требовательных геймеров.
Враги в Aviator краш игре онлайн представлены в самых разных формах и размерах. Здесь вы встретите группы из маленьких и быстрых врагов, а также огромных боссов с мощным вооружением. Разнообразие врагов позволяет игрокам использовать разные тактики и стратегии для победы.
Кроме того, Aviator игра предлагает разнообразие уровней сложности. Выберите легкий уровень, чтобы насладиться игровым процессом, или вызовите себе настоящий вызов, выбрав экспертный уровень. Независимо от выбранного уровня сложности, вы получите максимум удовольствия от игры и окунетесь в захватывающий мир авиаторов.
Играйте в Aviator и наслаждайтесь разнообразием врагов и уровней, которые позволят вам почувствовать себя настоящим авиатором.
YourDoll株式会社 実用的なダッチワイフでベッドの上で最高の楽しさと喜びを手に入れようダッチワイフのような人生であなたの仮定以上のものを手に入れようBuscasMuñecasRealistasdeSilicona?HablamosEspañol!ダッチワイフを購入するときにトリックを避ける方法は?
Наша бригада искусных исполнителей подготовлена предоставлять вам актуальные методы, которые не только предоставят прочную покров от холодных воздействий, но и подарят вашему жилью трендовый вид.
Мы деятельны с новыми веществами, сертифицируя прочный запас использования и выдающиеся результаты. Утепление внешней обшивки – это не только сбережение на тепле, но и забота о природной среде. Энергосберегающие технологические решения, какие мы внедряем, способствуют не только жилищу, но и сохранению природных ресурсов.
Самое первоочередное: [url=https://ppu-prof.ru/]Утепление дома цена за квадратный метр работа[/url] у нас стартует всего от 1250 рублей за м²! Это доступное решение, которое превратит ваш дом в подлинный теплый уголок с минимальными тратами.
Наши проекты – это не исключительно изоляция, это постройка площади, в где каждый элемент преломляет ваш собственный модель. Мы примем во внимание все ваши пожелания, чтобы осуществить ваш дом еще еще больше дружелюбным и привлекательным.
Подробнее на [url=https://ppu-prof.ru/]https://www.ppu-prof.ru/[/url]
Не откладывайте занятия о своем доме на потом! Обращайтесь к квалифицированным работникам, и мы сделаем ваш корпус не только более теплым, но и стильным. Заинтересовались? Подробнее о наших трудах вы можете узнать на веб-сайте. Добро пожаловать в мир удобства и качественной работы.
Наша команда опытных исполнителей подготовлена выдвинуть вам инновационные системы, которые не только обеспечат прочную безопасность от холодных воздействий, но и дарят вашему жилищу оригинальный вид.
Мы занимаемся с современными веществами, гарантируя долгосрочный продолжительность использования и прекрасные эффекты. Изолирование внешнего слоя – это не только экономия на тепле, но и заботливость о окружающей природе. Энергосберегающие технологические решения, какие мы осуществляем, способствуют не только дому, но и сохранению природы.
Самое основополагающее: [url=https://ppu-prof.ru/]Сколько стоит утепление стен снаружи[/url] у нас открывается всего от 1250 рублей за квадратный метр! Это бюджетное решение, которое метаморфозирует ваш жилище в реальный теплый местечко с небольшими затратами.
Наши пособия – это не лишь изоляция, это формирование помещения, в где любой член отразит ваш личный манеру. Мы возьмем во внимание все ваши пожелания, чтобы осуществить ваш дом еще больше приятным и привлекательным.
Подробнее на [url=https://ppu-prof.ru/]http://www.ppu-prof.ru/[/url]
Не откладывайте занятия о своем корпусе на потом! Обращайтесь к экспертам, и мы сделаем ваш дворец не только согретым, но и стильнее. Заинтересовались? Подробнее о наших работах вы можете узнать на веб-ресурсе. Добро пожаловать в универсум спокойствия и качественного исполнения.
I blog frequently and I genuinely appreciate your content. This article has really peaked my interest. I am going to bookmark your website and keep checking for new information about once a week. I subscribed to your RSS feed as well.
Hello very nice blog!! Guy .. Beautiful .. Amazing .. I will bookmark your web site and take the feeds also? I am satisfied to seek out numerous useful information here in the submit, we need develop more strategies in this regard, thank you for sharing. . . . . .
Hey there I am so excited I found your webpage, I really found you by mistake, while I was searching on Bing for something else, Nonetheless I am here now and would just like to say many thanks for a incredible post and a all round interesting blog (I also love the theme/design), I don’t have time to go through it all at the minute but I have saved it and also added in your RSS feeds, so when I have time I will be back to read a lot more, Please do keep up the fantastic job.
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
Hi there to all, how is everything, I think every one is getting more from this site, and your views are pleasant in favor of new people.
https://gruzmash1.ru
I am in fact happy to read this blog posts which includes lots of helpful information, thanks for providing such information.